Yonsei Med J.
2009 Feb;50(1):112-121. 10.3349/ymj.2009.50.1.112.
Epidemiology and Risk Factors for Bacteremia in 144 Consecutive Living-Donor Liver Transplant Recipients
- Affiliations
-
- 1Department of Internal Medicine, Kangnam St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Surgery, Kangnam St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. kimdg@catholic.ac.kr
- KMID: 1782976
- DOI: http://doi.org/10.3349/ymj.2009.50.1.112
Abstract
- PURPOSE
Bacteremia is a major infectious complication associated with mortality in liver transplant recipients. The causative organisms and clinical courses differ between medical centers due to variations in regional bacterial epidemiology and posttransplant care. Further, living donors in Korea contribute to 83% of liver transplants, and individualized data are required to improve survival rates.
PATIENTS AND METHODS
We retrospectively analyzed 104 subjects who had undergone living-donor liver transplant from 2005 to 2007.
RESULTS
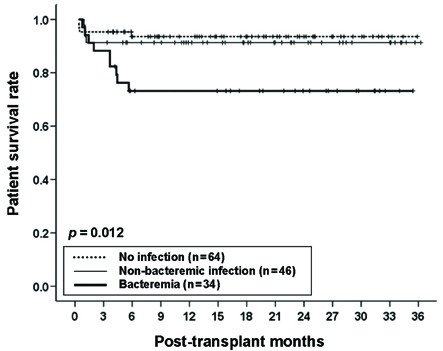
Among the 144 consecutive living-donor liver transplant recipients, 24% (34/144) developed bacteremia, 32% (46/144) developed non-bacteremic infections, and 44% (64/144) did not develop any infectious complications. Forty episodes of bacteremia occurred in 34 recipients. The major sources of bacteremia were intravascular catheter (30%; 12/40), biliary tract (30%; 12/40), and abdomen (22.5%; 9/40). Gram-positive cocci were more common (57.5%; 23/40) than Gram-negative rods (32.5 %; 13/40) and fungi (10%; 4/40). The data revealed that the following factors were significantly different between the bacteremia, non-bacteremic infection, and no infection groups: age (p = 0.024), posttransplant hemodialysis (p = 0.002), ICU stay (p = 0.012), posttransplant hospitalization (p < 0.0001), and duration of catheterization (p < 0.0001). The risk factors for bacteremia were older than 55 years (odds ratio, 6.1; p = 0.003), catheterization for more than 22 days (odds ratio, 4.0; p = 0.009), UNOS class IIA (odds ratio, 6.6; p = 0.039), and posttransplant hemodialysis (odds ratio, 23.1; p = 0.001). One-year survival rates in the bacteremic, non-bacteremic infection, and no infection groups were 73.2%, 91.3%, and 93.5%, respectively.
CONCLUSION
Early catheter removal and preservation of renal function should focus for improving survival after transplant.
MeSH Terms
-
Adult
Bacteremia/etiology/*mortality
Catheterization/adverse effects/statistics & numerical data
Female
Humans
Korea/epidemiology
Liver Transplantation/*mortality/statistics & numerical data
Living Donors
Male
Middle Aged
Postoperative Complications/etiology/*mortality
Predictive Value of Tests
Risk Factors
Survival Analysis
Figure
Cited by 2 articles
-
Epidemiology and Clinical Features of Post-Transplant Bloodstream Infection: An Analysis of 222 Consecutive Liver Transplant Recipients
Hyun Kyung Kim, Yong Keun Park, Hee-Jung Wang, Bong Wan Kim, So Youn Shin, Seung-Kwan Lim, Young Hwa Choi
Infect Chemother. 2013;45(3):315-324. doi: 10.3947/ic.2013.45.3.315.Impact of Early Positive Culture Results on the Short-term Outcomes of Liver Transplants
In Cho, Jin Joo Dong, Myoung Soo Kim, Dong Eun Yong, Kyu Ha Huh, Hong Choi Gi, Sub Choi Jin, Il Kim Soon
J Korean Soc Transplant. 2011;25(4):257-263. doi: 10.4285/jkstn.2011.25.4.257.
Reference
-
1. Fishman JA, Rubin RH. Infection in organ-transplant recipients. N Engl J Med. 1998. 338:1741–1751.2. Snydman DR. Infection in solid organ transplantation. Transpl Infect Dis. 1999. 1:21–28.3. Kwak EJ, Kusne S. Bowden RA, Ljungman P, Paya CV, editors. Risks and epidemiology of infections after liver transplantation. Transplant infection. 2003. 2nd ed. Philadelphia: Lippincott Williams & Wilkins;120.4. Wade JJ, Rolando N, Hayllar K, Philpott-Howard J, Casewell MW, Williams R. Bacterial and fungal infections after liver transplantation: an analysis of 284 patients. Hepatology. 1995. 21:1328–1336.
Article5. Singh N, Gayowski T, Wagener MM, Marino IR. Predictors and outcome of early-versus late-onset major bacterial infections in liver transplant recipients receiving tacrolimus (FK506) as primary immunosuppression. Eur J Clin Microbiol Infect Dis. 1997. 16:821–826.
Article6. Singh N, Wagener MM, Obman A, Cacciarelli TV, de Vera ME, Gayowski T. Bacteremias in liver transplant recipients: shift toward gram-negative bacteria as predominant pathogens. Liver Transpl. 2004. 10:844–849.
Article7. George DL, Arnow PM, Fox AS, Baker AL, Thistlethwaite JR, Emond JC, et al. Bacterial infection as a complication of liver transplantation: epidemiology and risk factors. Rev Infect Dis. 1991. 13:387–396.
Article8. Kusne S, Dummer JS, Singh N, Iwatsuki S, Makowka L, Esquivel C, et al. Infections after liver transplantation. An analysis of 101 consecutive cases. Medicine (Baltimore). 1988. 67:132–143.9. Wagener MM, Yu VL. Bacteremia in transplant recipients: a prospective study of demographics, etiologic agents, risk factors, and outcomes. Am J Infect Control. 1992. 20:239–247.10. Paya CV, Hermans PE, Washington JA 2nd, Smith TF, Anhalt JP, Wiesner RH, et al. Incidence, distribution, and outcome of episodes of infection in 100 orthotopic liver transplantations. Mayo Clin Proc. 1989. 64:555–564.11. Kawecki D, Chmura A, Pacholczyk M, Lagiewska B, Adadynski L, Wasiak D, et al. Etiological agents of bacteremia in the early period after liver transplantation. Transplant Proc. 2007. 39:2816–2821.
Article12. Singh N, Paterson DL, Gayowski T, Wagener MM, Marino IR. Predicting bacteremia and bacteremic mortality in liver transplant recipients. Liver Transpl. 2000. 6:54–61.13. Annual Report 2007. Korean Network for Organ Sharing. accessed 1 June 2008. Available from: URL: http://www.konos.go.kr.14. Cho WH, Kim YS. Landmarks in clinical transplantation in Korea. Yonsei Med J. 2004. 45:963–967.
Article15. Moon DB, Lee SG. Adult-to-adult living donor liver transplantation at the Asan medical center. Yonsei Med J. 2004. 45:1162–1168.
Article16. Chang FY, Singh N, Gayowski T, Wagener MM, Marino IR. Fever in liver transplant recipients: changing spectrum of etiologic agents. Clin Infect Dis. 1998. 26:59–65.17. Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988. 16:128–140.
Article18. Simon DM, Levin S. Infectious complications of solid organ transplantations. Infect Dis Clin North Am. 2001. 15:521–549.
Article19. Habib S, Berk B, Chang CC, Demetris AJ, Fontes P, Dvorchik I, et al. MELD and prediction of post-liver transplantation survival. Liver Transpl. 2006. 12:440–447.
Article20. Mellors JW, Horwitz RI, Harvey MR, Horwitz SM. A simple index to identify occult bacterial infection in adults with acute unexplained fever. Arch Intern Med. 1987. 147:666–671.
Article21. Candel FJ, Grima E, Matesanz M, Cervera C, Soto G, Almela M, et al. Bacteremia and septic shock after solid-organ transplantation. Transplant Proc. 2005. 37:4097–4099.
Article22. Bedini A, Codeluppi M, Cocchi S, Guaraldi G, Di Benedetto F, Venturelli C, et al. Gram-positive bloodstream infections in liver transplant recipients: incidence, risk factors, and impact on survival. Transplant Proc. 2007. 39:1947–1949.
Article23. Al Riyami D, Alam A, Badovinac K, Ivis F, Trpeski L, Cantarovich M. Decreased survival in liver transplant patients requiring chronic dialysis: a Canadian experience. Transplantation. 2008. 85:1277–1280.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ABO incompatibility is a risk factor for cytomegalovirus infection with living donor liver transplantation
- Liver retransplantation for adult recipients
- Unilateral Versus Bilateral Biliary Drainage for Post-Transplant Anastomotic Stricture
- Liver transplantation: a 10-year low-volume transplant center experience in Kazakhstan
- Donor’s quality of life after living donor liver transplantation and influencing factors in Mongolia