Korean J Radiol.
2006 Jun;7(2):87-96. 10.3348/kjr.2006.7.2.87.
Added Value of Coronal Reformations for Duty Radiologists and for Referring Physicians or Surgeons in the CT Diagnosis of Acute Appendicitis
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Institute of Radiation Medicine, Seoul National University Medical Research Center, Gyeonggi-do, Korea. yhk@snubhrad.snu.ac.kr
- 2Medical Research Collaborating Center, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Gyeonggi-do, Korea.
- 4Emergency Department, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Gyeonggi-do, Korea.
- KMID: 1782181
- DOI: http://doi.org/10.3348/kjr.2006.7.2.87
Abstract
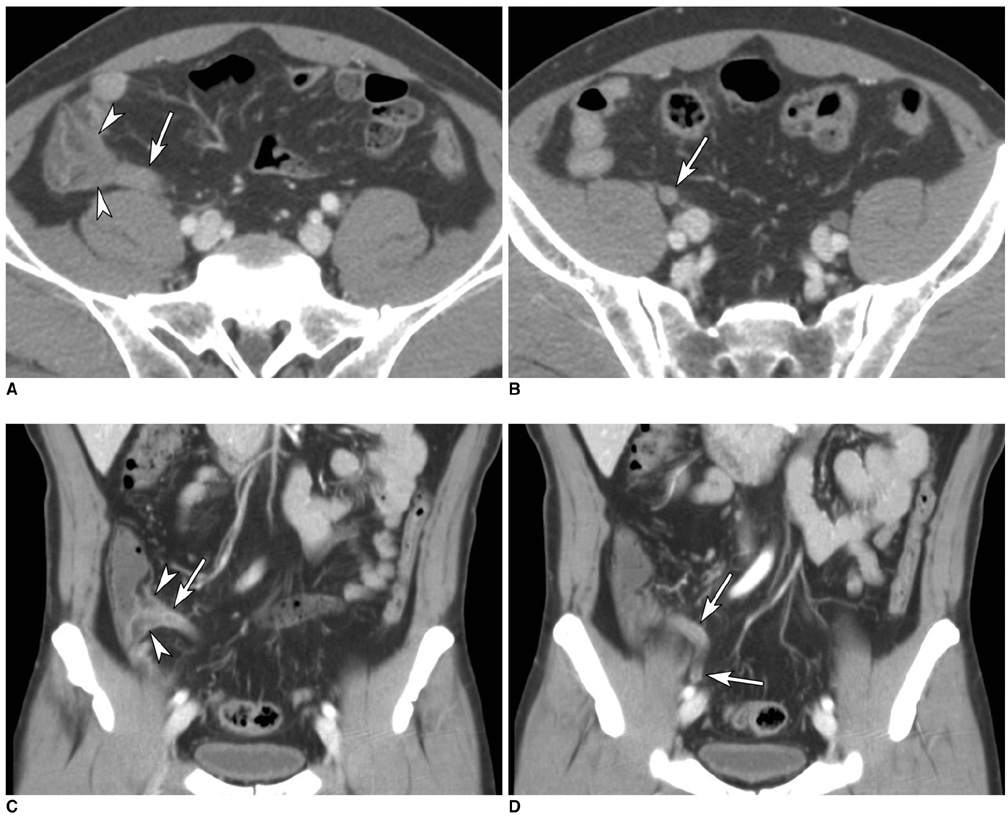
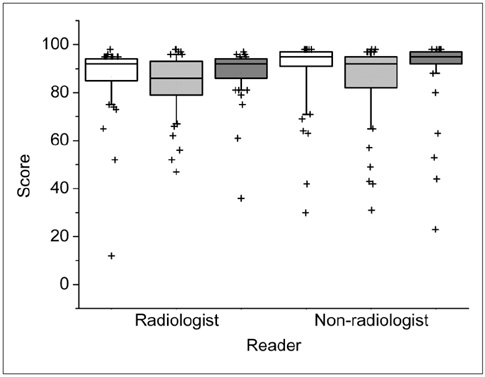
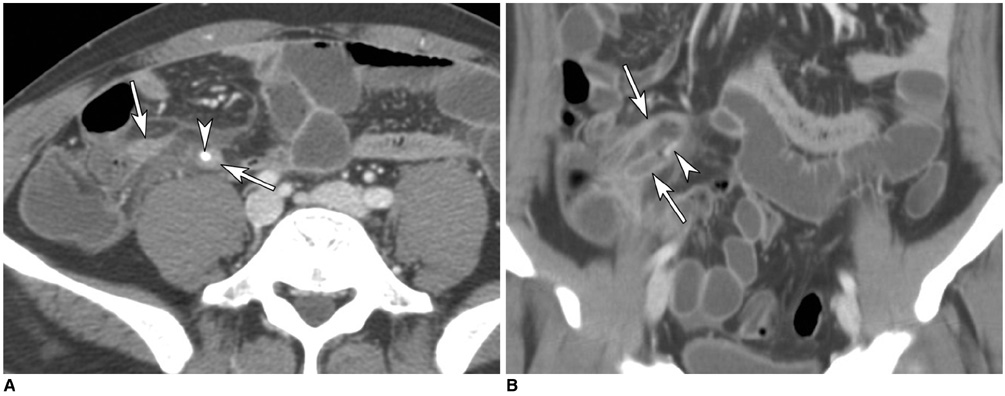
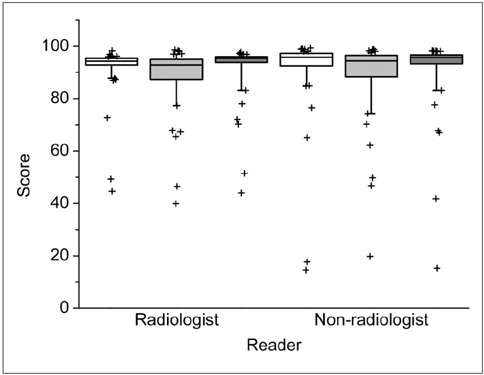
OBJECTIVE
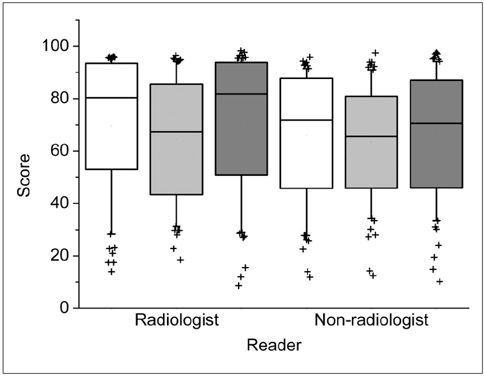
To assess the added value of coronal reformation for radiologists and for referring physicians or surgeons in the CT diagnosis of acute appendicitis. MATERIALS AND METHODS: Contrast-enhanced CT was performed using 16-detector-row scanners in 110 patients, 46 of whom had appendicitis. Transverse (5-mm thickness, 4-mm increment), coronal (5-mm thickness, 4-mm increment), and combined transverse and coronal sections were interpreted by four radiologists, two surgeons and two emergency physicians. The area under the receiver operating characteristic curve (Az value), sensitivity, specificity (McNemar test), diagnostic confidence and appendiceal visualization (Wilcoxon signed rank test) were compared. RESULTS: For radiologists, the additional coronal sections tended to increase the Az value (0.972 vs. 0.986, p = 0.076) and pooled sensitivity (92% [95% CI: 88, 96] vs. 96% [93, 99]), and enhanced appendiceal visualization in true-positive cases (p = 0.031). For non-radiologists, no such enhancement was observed, and the confidence for excluding acute appendicitis declined (p = 0.013). Coronal sections alone were inferior to transverse sections for diagnostic confidence as well as appendiceal visualization for each reader group studied (p < 0.05). CONCLUSION: The added value of coronal reformation is more apparent for radiologists compared to referring physicians or surgeons in the CT diagnosis of acute appendicitis.
Keyword
MeSH Terms
Figure
Reference
-
1. Raptopoulos V, Katsou G, Rosen MP, Siewert B, Goldberg SN, Kruskal JB. Acute appendicitis: effect of increased use of CT on selecting patients earlier. Radiology. 2003. 226:521–526.2. Rhea JT, Halpern EF, Ptak T, Lawrason JN, Sacknoff R, Novelline RA. The status of appendiceal CT in an Urban Medical Center 5 years after its introduction: experience with 753 patients. AJR Am J Roentgenol. 2005. 184:1802–1808.3. Kaiser S, Frenckner B, Jorulf HK. Suspected appendicitis in children: US and CT--a prospective randomized study. Radiology. 2002. 223:633–638.4. Poortman P, Lohle PN, Schoemaker CM, Oostvogel HJ, Teepen HJ, Zwinderman KA, et al. Comparison of CT and sonography in the diagnosis of acute appendicitis: a blinded prospective study. AJR Am J Roentgenol. 2003. 181:1355–1359.5. Wijetunga R, Tan BS, Rouse JC, Bigg-Wither GW, Doust BD. Diagnostic accuracy of focused appendiceal CT in clinically equivocal cases of acute appendicitis. Radiology. 2001. 221:747–753.6. Wise SW, Labuski MR, Kasales CJ, Blebea JS, Meilstrup JW, Holley GP, et al. Comparative assessment of CT and sonographic techniques for appendiceal imaging. AJR Am J Roentgenol. 2001. 176:933–941.7. Checkoff JL, Wechsler RJ, Nazarian LN. Chronic inflammatory appendiceal conditions that mimic acute appendicitis on helical CT. AJR Am J Roentgenol. 2002. 179:731–734.8. Lowe LH, Draud KS, Hernanz-Schulman M, Newton MR, Heller RM, Stein SM, et al. Nonenhanced limited CT in children suspected of having appendicitis: prospective comparison of attending and resident interpretations. Radiology. 2001. 221:755–759.9. Albano MC, Ross GW, Ditchek JJ, Duke GL, Teeger S, Sostman HD, et al. Resident interpretation of emergency CT scans in the evaluation of acute appendicitis. Acad Radiol. 2001. 8:915–918.10. Rao PM, Rhea JT, Novelline RA, McCabe CJ, Lawrason JN, Berger DL, et al. Helical CT technique for the diagnosis of appendicitis: prospective evaluation of a focused appendix CT examination. Radiology. 1997. 202:139–144.11. Jacobs JE, Birnbaum BA, Macari M, Megibow AJ, Israel G, Maki DD, et al. Acute appendicitis: comparison of helical CT diagnosis focused technique with oral contrast material versus nonfocused technique with oral and intravenous contrast material. Radiology. 2001. 220:683–690.12. Weltman DI, Yu J, Krumenacker J Jr, Huang S, Moh P. Diagnosis of acute appendicitis: comparison of 5- and 10-mm CT sections in the same patient. Radiology. 2000. 216:172–177.13. Lane MJ, Liu DM, Huynh MD, Jeffrey RB Jr, Mindelzun RE, Katz DS. Suspected acute appendicitis: nonenhanced helical CT in 300 consecutive patients. Radiology. 1999. 213:341–346.14. Keyzer C, Tack D, de Maertelaer V, Bohy P, Gevenois PA, Van Gansbeke D. Acute appendicitis: comparison of low-dose and standard-dose unenhanced multi-detector row CT. Radiology. 2004. 232:164–172.15. Lane MJ, Katz DS, Ross BA, Clautice-Engle TL, Mindelzun RE, Jeffrey RB Jr. Unenhanced helical CT for suspected acute appendicitis. AJR Am J Roentgenol. 1997. 168:405–409.16. Mullins ME, Kircher MF, Ryan DP, Doody D, Mullins TC, Rhea JT, et al. Evaluation of suspected appendicitis in children using limited helical CT and colonic contrast material. AJR Am J Roentgenol. 2001. 176:37–41.17. Paulson EK, Harris JP, Jaffe TA, Haugan PA, Nelson RC. Acute appendicitis: added diagnostic value of coronal reformations from isotropic voxels at multi-detector row CT. Radiology. 2005. 235:879–885.18. Paulson EK, Jaffe TA, Thomas J, Harris JP, Nelson RC. MDCT of patients with acute abdominal pain: a new perspective using coronal reformations from submillimeter isotropic voxels. AJR Am J Roentgenol. 2004. 183:899–906.19. Bendeck SE, Nino-Murcia M, Berry GJ, Jeffrey RB Jr. Imaging for suspected appendicitis: negative appendectomy and perforation rates. Radiology. 2002. 225:131–136.20. Nikolaidis P, Hwang CM, Miller FH, Papanicolaou N. The nonvisualized appendix: incidence of acute appendicitis when secondary inflammatory changes are absent. AJR Am J Roentgenol. 2004. 183:889–892.21. Deeks JJ. Systematic reviews in health care: Systematic reviews of evaluations of diagnostic and screening tests. BMJ. 2001. 323:157–162.22. Callahan MJ, Rodriguez DP, Taylor GA. CT of appendicitis in children. Radiology. 2002. 224:325–332.23. Guidry SP, Poole GV. The anatomy of appendicitis. Am J Surg. 1994. 60:68–71.24. Wagner JM, McKinney WP, Carpenter JL. Does this patient have appendicitis? JAMA. 1996. 276:1589–1594.25. Motulsky H. Intuitive biostatistics. 1995. New York: Oxford University Press;106–112.26. Malone AJ Jr, Wolf CR, Malmed AS, Melliere BF. Diagnosis of acute appendicitis: value of unenhanced CT. AJR Am J Roentgenol. 1993. 160:763–766.27. Rao PM, Rhea JT, Novelline RA, Mostafavi AA, Lawrason JN, McCabe CJ. Helical CT combined with contrast material administered only through the colon for imaging of suspected appendicitis. AJR Am J Roentgenol. 1997. 169:1275–1280.28. Balthazar EJ, Birnbaum BA, Yee J, Megibow AJ, Roshkow J, Gray C. Acute appendicitis: CT and US correlation in 100 patients. Radiology. 1994. 190:31–35.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Benefit of Added Coronal Reformation Images in the MDCT Diagnosis of Acute Appendicitis for Emergency Physicians
- CT Findings of Acute Appendicitis in Children
- Added Value of Using a CT Coronal Reformation to Diagnose Adnexal Torsion
- Accuracy of Emergency Physician's Ultrasonography in the Diagnosis of Acute Appendicitis
- Radiologic Reports: Attitudes, Preferred Type, and Opinion of Referring Physicians