J Korean Med Sci.
2009 Oct;24(5):894-903. 10.3346/jkms.2009.24.5.894.
Positional Reproducibility and Effects of a Rectal Balloon in Prostate Cancer Radiotherapy
- Affiliations
-
- 1Department of Radiation Oncology, Yonsei Cancer Center, Yonsei University Health System, Seoul, Korea. gekim@yuhs.ac
- 2Division of Clinical Data Management System and Bioinformatics, Clinical Trials Center, Yonsei University Health System, Seoul, Korea.
- KMID: 1782013
- DOI: http://doi.org/10.3346/jkms.2009.24.5.894
Abstract
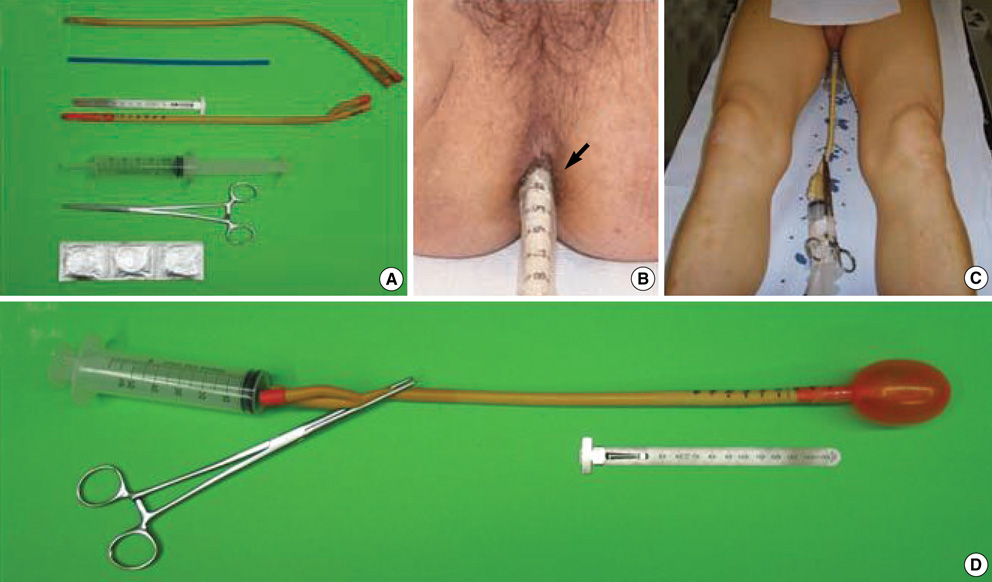
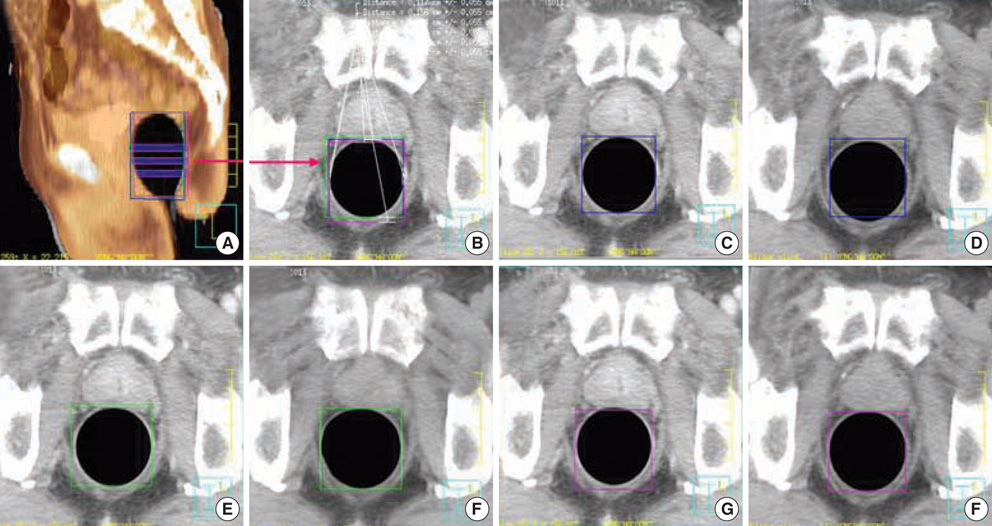
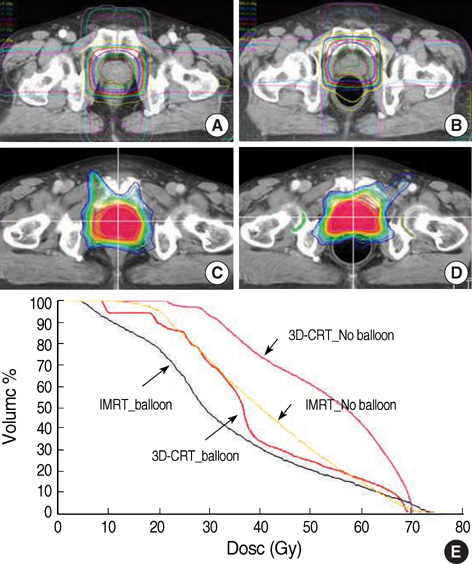
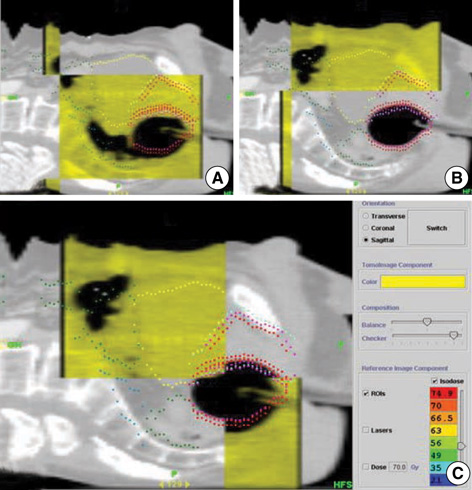
- Despite the increasing use of the rectal balloon in prostate cancer radiotherapy, many issues still remain to be verified objectively including its positional reproducibility and relevance to treatment morbidity. We have developed a custom rectal balloon that has a scale indicating the depth of insertion and dilates symmetrically ensuring positional reproducibility. Fifty patients with prostate cancer treated by definitive 3D-conformal radiotherapy (3D-CRT) or intensity-modulated radiotherapy (IMRT) with rectal balloon were analyzed. Each of first five patients undergone computed tomography (CT) three times with a rectal balloon. The positional reproducibility was tested by Intraclass Correlation Coefficient (ICC) from the CT-to-CT fusion images. Planning variables and clinical acute toxicities were compared between when or not applying balloon. An ICC of greater than 0.9 in all directions revealed an excellent reproducibility of the balloon. Rectal balloon improved considerably the mean dose and V(45Gy)-V(65Gy) in plan comparison, and especially in 3D-CRT the rectal volume exposed to more than 60 Gy dropped from 41.3% to 19.5%. Clinically, the balloon lowered acute toxicity, which was lowest when both the balloon and IMRT were applied simultaneously. The rectal balloon carries excellent reproducibility and reduces acute toxicity in 3D-CRT and IMRT for prostate cancer.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Toxicity of Tomotherapy-Based Simultaneous Integrated Boost in Whole-Pelvis Radiation for Prostate Cancer
Sei Hwan You, Jong Young Lee, Chang Geol Lee
Yonsei Med J. 2015;56(2):510-518. doi: 10.3349/ymj.2015.56.2.510.
Reference
-
1. Hanks GE, Hanlon AL, Schultheiss TE, Pinover WH, Movsas B, Epstein BE, Hunt MA. Dose escalation with 3D conformal treatment: five year outcomes, treatment optimization, and future directions. Int J Radiat Oncol Biol Phys. 1998. 41:501–510.
Article2. Pollack A, Hanlon AL, Horwitz EM, Feigenberg SJ, Uzzo RG, Hanks GE. Prostate cancer radiotherapy dose response: an update of the fox chase experience. J Urol. 2004. 171:1132–1136.
Article3. Zelefsky MJ, Leibel SA, Gaudin PB, Kutcher GJ, Fleshner NE, Venkatramen ES, Reuter VE, Fair WR, Ling CC, Fuks Z. Dose escalation with three-dimensional conformal radiation therapy affects the outcome in prostate cancer. Int J Radiat Oncol Biol Phys. 1998. 41:491–500.
Article4. Cahlon O, Zelefsky MJ, Shippy A, Chan H, Fuks Z, Yamada Y, Hunt M, Greenstein S, Amols H. Ultra-high dose (86.4 Gy) IMRT for localized prostate cancer: toxicity and biochemical outcomes. Int J Radiat Oncol Biol Phys. 2008. 71:330–337.
Article5. Vigneault E, Pouliot J, Laverdiere J, Roy J, Dorion M. Electronic portal imaging device detection of radioopaque markers for the evaluation of prostate position during megavoltage irradiation: a clinical study. Int J Radiat Oncol Biol Phys. 1997. 37:205–212.
Article6. Balter JM, Lam KL, Sandler HM, Littles JF, Bree RL, Ten Haken RK. Automated localization of the prostate at the time of treatment using implanted radiopaque markers: technical feasibility. Int J Radiat Oncol Biol Phys. 1995. 33:1281–1286.
Article7. Lattanzi J, McNeeley S, Pinover W, Horwitz E, Das I, Schultheiss TE, Hanks GE. A comparison of daily CT localization to a daily ultrasound-based system in prostate cancer. Int J Radiat Oncol Biol Phys. 1999. 43:719–725.
Article8. Bastasch MD, Teh BS, Mai WY, McGary JE, Grant WH 3rd, Butler EB. Tolerance of endorectal balloon in 396 patients treated with intensity-modulated radiation therapy (IMRT) for prostate cancer. Am J Clin Oncol. 2006. 29:8–11.
Article9. D'Amico AV, Manola J, McMahon E, Loffredo M, Lopes L, Ching J, Albert M, Hurwitz M, Suh WW, Vivenzio TA, Beard C. A prospective evaluation of rectal bleeding after dose-escalated three-dimensional conformal radiation therapy using an intrarectal balloon for prostate gland localization and immobilization. Urology. 2006. 67:780–784.10. Teh BS, Mai WY, Uhl BM, Augspurger ME, Grant WH 3rd, Lu HH, Woo SY, Carpenter LS, Chiu JK, Butler EB. Intensity-modulated radiation therapy (IMRT) for prostate cancer with the use of a rectal balloon for prostate immobilization: acute toxicity and dose-volume analysis. Int J Radiat Oncol Biol Phys. 2001. 49:705–712.
Article11. Wachter S, Gerstner N, Dorner D, Goldner G, Colotto A, Wambersie A, Potter R. The influence of a rectal balloon tube as internal immobilization device on variations of volumes and dose-volume histograms during treatment course of conformal radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2002. 52:91–100.
Article12. Teh BS, McGary JE, Dong L, Mai WY, Carpenter LS, Lu HH, Chiu JK, Woo SY, Grant WH, Butler EB. The use of rectal balloon during the delivery of intensity modulated radiotherapy (IMRT) for prostate cancer: more than just a prostate gland immobilization device? Cancer J. 2002. 8:476–483.13. Patel RR, Orton N, Tome WA, Chappell R, Ritter MA. Rectal dose sparing with a balloon catheter and ultrasound localization in conformal radiation therapy for prostate cancer. Radiother Oncol. 2003. 67:285–294.
Article14. van Lin EN, Kristinsson J, Philippens ME, de Jong DJ, van der Vight LP, Kaanders JH, Leer JW, Visser AG. Reduced late rectal mucosal changes after prostate three-dimensional conformal radiotherapy with endorectal balloon as observed in repeated endoscopy. Int J Radiat Oncol Biol Phys. 2007. 67:799–811.
Article15. Court LE, D'Amico AV, Kadam D, Cormack R. Motion and shape change when using an endorectal balloon during prostate radiation therapy. Radiother Oncol. 2006. 81:184–189.
Article16. Ciernik IF, Baumert BG, Egli P, Glanzmann C, Lutolf UM. On-line correction of beam portals in the treatment of prostate cancer using an endorectal balloon device. Radiother Oncol. 2002. 65:39–45.
Article17. van Lin EN, van der Vight LP, Witjes JA, Huisman HJ, Leer JW, Visser AG. The effect of an endorectal balloon and off-line correction on the interfraction systematic and random prostate position variations: a comparative study. Int J Radiat Oncol Biol Phys. 2005. 61:278–288.
Article18. El-Bassiouni M, Davis JB, El-Attar I, Studer GM, Lutolf UM, Ciernik IF. Target motion variability and on-line positioning accuracy during external-beam radiation therapy of prostate cancer with an endorectal balloon device. Strahlenther Onkol. 2006. 182:531–536.
Article19. Munro BH. Statistical methods for health care research. 2005. 5th ed. Philadelphia: Lippincott Williams & Wilkins.20. Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998. 17:101–110.
Article21. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995. 31:1341–1346.
Article22. Goldner G, Geinitz H, Wachter S, Becker G, Zimmermann F, Wachter-Gerstner N, Glocker S, Potzi R, Wambersie A, Bamberg M, Molls M, Feldmann H, Potter R. 3-D Conformal radiotherapy of localized prostate cancer within an Austrian-German multicenter trial: a prospective study of patients' acceptance of the rectal balloon during treatment. Wien Klin Wochenschr. 2006. 118:224–229.
Article23. Kupelian PA, Reddy CA, Carlson TP, Altsman KA, Willoughby TR. Preliminary observations on biochemical relapse-free survival rates after short-course intensity-modulated radiotherapy (70 Gy at 2.5 Gy/fraction) for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2002. 53:904–912.
Article24. Zelefsky MJ, Fuks Z, Hunt M, Yamada Y, Marion C, Ling CC, Amols H, Venkatraman ES, Leibel SA. High-dose intensity modulated radiation therapy for prostate cancer: early toxicity and biochemical outcome in 772 patients. Int J Radiat Oncol Biol Phys. 2002. 53:1111–1116.
Article25. Pollack A, Zagars GK, Starkschall G, Childress CH, Kopplin S, Boyer AL, Rosen II. Conventional vs. conformal radiotherapy for prostate cancer: preliminary results of dosimetry and acute toxicity. Int J Radiat Oncol Biol Phys. 1996. 34:555–564.
Article26. Pollack A, Hanlon AL, Horwitz EM, Feigenberg SJ, Konski AA, Movsas B, Greenberg RE, Uzzo RG, Ma CM, McNeeley SW, Buyyounouski MK, Price RA Jr. Dosimetry and preliminary acute toxicity in the first 100 men treated for prostate cancer on a randomized hypofractionation dose escalation trial. Int J Radiat Oncol Biol Phys. 2006. 64:518–526.
Article27. De Meerleer G, Vakaet L, Meersschout S, Villeirs G, Verbaeys A, Oosterlinck W, De Neve W. Intensity-modulated radiotherapy as primary treatment for prostate cancer: acute toxicity in 114 patients. Int J Radiat Oncol Biol Phys. 2004. 60:777–787.
Article28. Sanghani MV, Ching J, Schultz D, Cormack R, Loffredo M, McMahon E, Beard C, D'Amico AV. Impact on rectal dose from the use of a prostate immobilization and rectal localization device for patients receiving dose escalated 3D conformal radiation therapy. Urol Oncol. 2004. 22:165–168.
Article29. Ronson BB, Yonemoto LT, Rossi CJ, Slater JM, Slater JD. Patient tolerance of rectal balloons in conformal radiation treatment of prostate cancer. Int J Radiat Oncol Biol Phys. 2006. 64:1367–1370.
Article30. Hille A, Schmidberger H, Tows N, Weiss E, Vorwerk H, Hess CF. The impact of varying volumes in rectal balloons on rectal dose sparing in conformal radiation therapy of prostate cancer. A prospective three-dimensional analysis. Strahlenther Onkol. 2005. 181:709–716.31. Teh BS, Dong L, McGary JE, Mai WY, Grant W 3rd, Butler EB. Rectal wall sparing by dosimetric effect of rectal balloon used during intensity-modulated radiation therapy (IMRT) for prostate cancer. Med Dosim. 2005. 30:25–30.
Article32. Kupelian PA, Thakkar VV, Khuntia D, Reddy CA, Klein EA, Mahadevan A. Hypofractionated intensity-modulated radiotherapy (70 gy at 2.5 Gy per fraction) for localized prostate cancer: long-term outcomes. Int J Radiat Oncol Biol Phys. 2005. 63:1463–1468.
Article33. Livsey JE, Cowan RA, Wylie JP, Swindell R, Read G, Khoo VS, Logue JP. Hypofractionated conformal radiotherapy in carcinoma of the prostate: five-year outcome analysis. Int J Radiat Oncol Biol Phys. 2003. 57:1254–1259.
Article34. Brenner DJ, Hall EJ. Fractionation and protraction for radiotherapy of prostate carcinoma. Int J Radiat Oncol Biol Phys. 1999. 43:1095–1101.
Article35. Fowler JF, Ritter MA, Chappell RJ, Brenner DJ. What hypofractionated protocols should be tested for prostate cancer? Int J Radiat Oncol Biol Phys. 2003. 56:1093–1104.
Article36. Craig T, Moiseenko V, Battista J, Van Dyk J. The impact of geometric uncertainty on hypofractionated external beam radiation therapy of prostate cancer. Int J Radiat Oncol Biol Phys. 2003. 57:833–842.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment outcome of localized prostate cancer by 70 Gy hypofractionated intensity-modulated radiotherapy with a customized rectal balloon
- Colorectal Perforation After Anorectal Manometry for Low Anterior Resection Syndrome
- Choroidal Metastasis from Prostate Cancer
- Controversial issues in radiotherapy for rectal cancer: a systematic review
- The prostate specific antigen in detection of the prostate cancer