Ann Lab Med.
2013 Mar;33(2):125-129. 10.3343/alm.2013.33.2.125.
A Case of Systemic Mastocytosis Associated with Acute Myeloid Leukemia Terminating as Aleukemic Mast Cell Leukemia after Allogeneic Hematopoietic Stem Cell Transplantation
- Affiliations
-
- 1Department of Laboratory Medicine, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea. cjpark@amc.seoul.kr
- 2Department of Internal Medicine, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea.
- KMID: 1781312
- DOI: http://doi.org/10.3343/alm.2013.33.2.125
Abstract
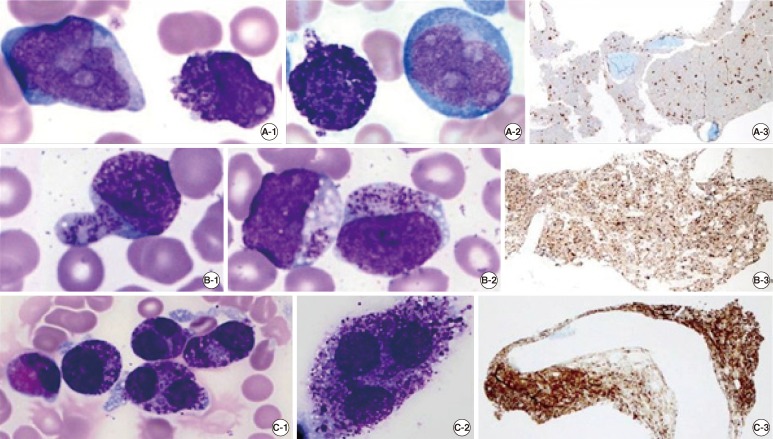
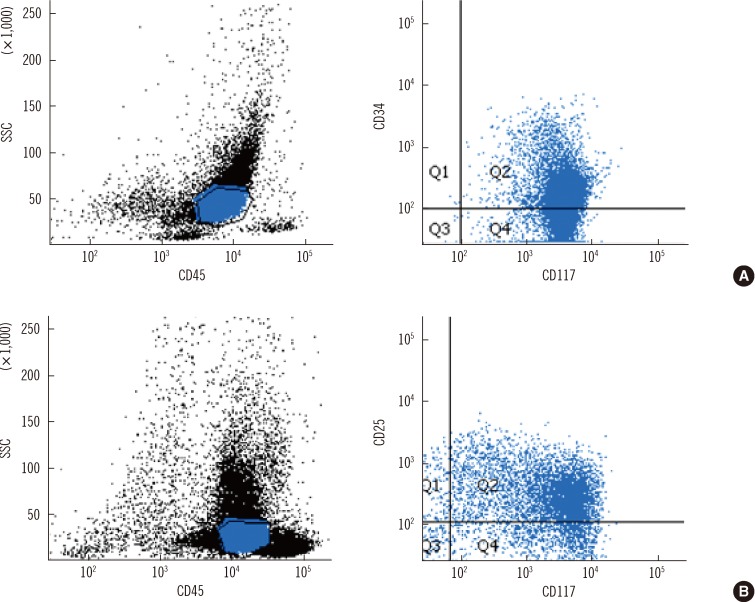
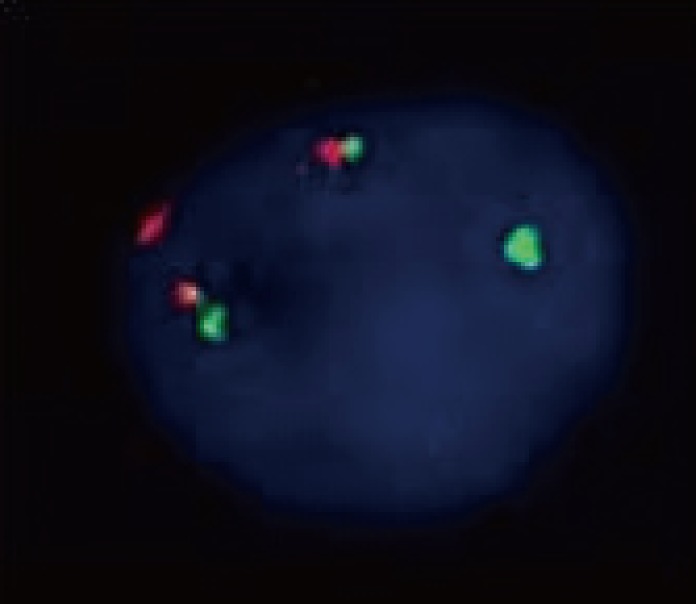
- In up to 40% of systemic mastocytosis (SM) cases, an associated clonal hematological non-mast cell lineage disease such as AML is diagnosed before, simultaneously with, or after the diagnosis of SM. A 40-yr-old man was diagnosed with AML with t(8;21)(q22;q22). Mast cells were not noted at diagnosis, but appeared as immature forms at relapse. After allogeneic hematopoietic stem cell transplantation (HSCT), leukemic myeloblasts were not observed; however, neoplastic metachromatic blasts strikingly proliferated during the state of bone marrow aplasia, and finally, aleukemic mast cell leukemia developed. As the disease progressed, we observed serial morphologic changes from immature mast cells with myeloblasts to only metachromatic blasts and atypical mast cells as mast cell leukemia; FISH analysis showed that the neoplastic mast cells originated from the same clone as the leukemic myeloblasts of AML.
Keyword
MeSH Terms
-
Adult
Bone Marrow Cells/pathology
Chromosomes, Human, Pair 21
Chromosomes, Human, Pair 8
*Hematopoietic Stem Cell Transplantation
Humans
In Situ Hybridization, Fluorescence
Leukemia, Mast-Cell/diagnosis/etiology
Leukemia, Myeloid, Acute/complications/*diagnosis/therapy
Leukocytes, Mononuclear/pathology
Male
Mastocytosis, Systemic/*diagnosis/etiology
Recurrence
Translocation, Genetic
Transplantation, Homologous
Figure
Cited by 2 articles
-
De novo Leukemic Variant of Mast Cell Leukemia WithKIT D816V
Hae In Bang, Rojin Park, Eun Su Park, In Ho Choi, Kyoung Ha Kim, Jeong Won Shin, Tae Youn Choi, Kyungja Han, Jong-Ho Won
Ann Lab Med. 2015;35(2):260-262. doi: 10.3343/alm.2015.35.2.260.The roles of mast cells in allergic inflammation and mast cell-related disorders
Hee-Kyoo Kim
Allergy Asthma Respir Dis. 2017;5(5):248-255. doi: 10.4168/aard.2017.5.5.248.
Reference
-
1. Horny HP, Metcalfe DD, Bennett JM, Bain BJ, Akin C, Escribano L, et al. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, editors. Mastocytosis. WHO classification of tumours of haematopoietic and lymphoid tissues. 2008. 4th ed. Lyon: IARC Press;p. 54–63.2. Lim KH, Tefferi A, Lasho TL, Finke C, Patnaik M, Butterfield JH, et al. Systemic mastocytosis in 342 consecutive adults: survival studies and prognostic factors. Blood. 2009; 113:5727–5736. PMID: 19363219.
Article3. Valent P, Akin C, Sperr WR, Mayerhofer M, Födinger M, Fritsche-Polanz R, et al. Mastocytosis: pathology, genetics, and current options for therapy. Leuk Lymphoma. 2005; 46:35–48. PMID: 15621779.
Article4. Schnittger S, Kohl TM, Haferlach T, Kern W, Hiddemann W, Spiekermann K, et al. KIT-D816 mutations in AML1-ETO-positive AML are associated with impaired event-free and overall survival. Blood. 2006; 107:1791–1799. PMID: 16254134.
Article5. Valent P, Horny HP, Escribano L, Longley BJ, Li CY, Schwartz LB, et al. Diagnostic criteria and classification of mastocytosis: a consensus proposal. Leuk Res. 2001; 25:603–625. PMID: 11377686.
Article6. Sperr WR, Walchshofer S, Horny HP, Födinger M, Simonitsch I, Fritsche-Polanz R, et al. Systemic mastocytosis associated with acute myeloid leukaemia: report of two cases and detection of the c-kit mutation Asp-816 to Val. Br J Haematol. 1998; 103:740–749. PMID: 9858225.
Article7. Escribano L, Garca-Montero A, Núñez-Lopez R, López-Jiménez J, Almeida J, Prados A, et al. Systemic mastocytosis associated with acute myeloid leukemia: case report and implications for disease pathogenesis. J Allergy Clin Immunol. 2004; 114:28–33. PMID: 15241340.
Article8. Bernd HW, Sotlar K, Lorenzen J, Osieka R, Fabry U, Valent P, et al. Acute myeloid leukaemia with t(8;21) associated with "occult" mastocytosis. Report of an unusual case and review of the literature. J Clin Pathol. 2004; 57:324–328. PMID: 14990611.
Article9. Pullarkat V, Bedell V, Kim Y, Bhatia R, Nakamura R, Forman S, et al. Neoplastic mast cells in systemic mastocytosis associated with t(8;21) acute myeloid leukemia are derived from the leukemic clone. Leuk Res. 2007; 31:261–265. PMID: 16876862.
Article10. Nagai S, Ichikawa M, Takahashi T, Sato H, Yokota H, Oshima K, et al. The origin of neoplastic mast cells in systemic mastocytosis with AML1/ETO-positive acute myeloid leukemia. Exp Hematol. 2007; 35:1747–1752. PMID: 17976525.
Article11. Paschka P, Marcucci G, Ruppert AS, Mrózek K, Chen H, Kittles RA, et al. Adverse prognostic significance of KIT mutations in adult acute myeloid leukemia with inv(16) and t(8;21): a Cancer and Leukemia Group B Study. J Clin Oncol. 2006; 24:3904–3911. PMID: 16921041.12. Sperr WR, Drach J, Hauswirth AW, Ackermann J, Mitterbauer M, Mitterbauer G, et al. Myelomastocytic leukemia: evidence for the origin of mast cells from the leukemic clone and eradication by allogeneic stem cell transplantation. Clin Cancer Res. 2005; 11:6787–6792. PMID: 16203765.
Article13. Chen TY, Chen JS, Huang WT, Su WC, Tsao CJ. Rapid engraftment of mast cells of donor origin in a case of acute myeloid leukemia with mast cell leukemia after allogeneic stem cell transplantation. Bone Marrow Transplant. 2003; 32:111–114. PMID: 12815487.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Report of the Second de Novo Acute Myeloid Leukemia (AML) Following Allogeneic Stem Cell Transplantation in a Patient with the First AML
- Ultrasound and MR Findings of Aleukemic Leukemia Cutis in a Patient with Complete Remission of Acute Lymphoblastic Leukemia: A Case Report
- A Case of Double-unit Cord Blood Transplantation in Primary Refractory Acute Myeloid Leukemia
- Chronic graft versus host disease with small bowel obstruction after unrelated hematopoietic stem cell transplantation in a patient with acute myeloid leukemia
- Four cases of chloroma treated with hematopoietic stem cell transplantation