Yonsei Med J.
2012 Jan;53(1):198-203. 10.3349/ymj.2012.53.1.198.
Lipid-Emulsion Propofol Less Attenuates the Regulation of Body Temperature than Micro-Emulsion Propofol or Sevoflurane in the Elderly
- Affiliations
-
- 1Departments of Anesthesiology and Pain Medicine, Chonnam National University Medical School, Gwangju, Korea. mhyoon@jnu.ac.kr
- KMID: 1779707
- DOI: http://doi.org/10.3349/ymj.2012.53.1.198
Abstract
- PURPOSE
Anesthesia and surgery commonly cause hypothermia, and this caused by a combination of anesthetic-induced impairment of thermoregulatory control, a cold operation room environment and other factors that promote heat loss. All the general anesthetics markedly impair normal autonomic thermoregulatory control. The aim of this study is to evaluate the effect of two different types of propofol versus inhalation anesthetic on the body temperature.
MATERIALS AND METHODS
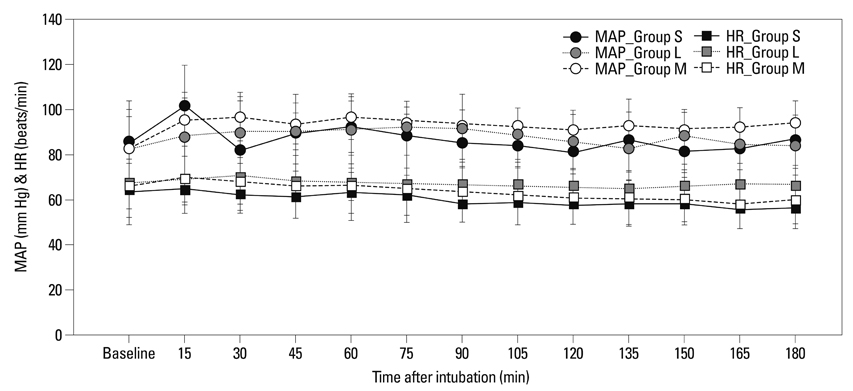
In this randomized controlled study, 36 patients scheduled for elective laparoscopic gastrectomy were allocated into three groups; group S (sevoflurane, n=12), group L (lipid-emulsion propofol, n=12) and group M (micro-emulsion propofol, n=12). Anesthesia was maintained with typical doses of the study drugs and all the groups received continuous remifentanil infusion. The body temperature was continuously monitored after the induction of general anesthesia until the end of surgery.
RESULTS
The body temperature was decreased in all the groups. The temperature gradient of each group (group S, group L and group M) at 180 minutes from induction of anesthesia was 2.5+/-0.6degrees C, 1.6+/-0.5degrees C and 2.3+/-0.6degrees C, respectively. The body temperature of group L was significantly higher than that of group S and group M at 30 minutes and 75 minute after induction of anesthesia, respectively. There were no temperature differences between group S and group M.
CONCLUSION
The body temperature is maintained at a higher level in elderly patients anesthetized with lipid-emulsion propofol.
Keyword
MeSH Terms
-
Aged
Aging
Anesthesia, General/*methods
Anesthetics, Combined/administration & dosage
Anesthetics, Inhalation/*administration & dosage
Anesthetics, Intravenous/*administration & dosage
Body Temperature/*drug effects
Body Temperature Regulation/drug effects
Fat Emulsions, Intravenous
Female
Humans
Male
Methyl Ethers/*administration & dosage
Middle Aged
Propofol/*administration & dosage
Figure
Reference
-
1. Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996. 334:1209–1215.
Article2. Frank SM, Beattie C, Christopherson R, Norris EJ, Perler BA, Williams GM, et al. Unintentional hypothermia is associated with postoperative myocardial ischemia. The Perioperative Ischemia Randomized Anesthesia Trial Study Group. Anesthesiology. 1993. 78:468–476.
Article3. Forstot RM. The etiology and management of inadvertent perioperative hypothermia. J Clin Anesth. 1995. 7:657–674.
Article4. Sessler DI. Miller RD, editor. Temperature Monitoring. Miller's Anesthesia. 2005. 6th ed. Philadelphia: Elsevier Churchill Livingston;1571–1597.5. Insler SR, Sessler DI. Perioperative thermoregulation and temperature monitoring. Anesthesiol Clin. 2006. 24:823–837.
Article6. Ozaki M, Sessler DI, Matsukawa T, Ozaki K, Atarashi K, Negishi C, et al. The threshold for thermoregulatory vasoconstriction during nitrous oxide/sevoflurane anesthesia is reduced in the elderly. Anesth Analg. 1997. 84:1029–1033.
Article7. Matsukawa T, Kurz A, Sessler DI, Bjorksten AR, Merrifield B, Cheng C. Propofol linearly reduces the vasoconstriction and shivering thresholds. Anesthesiology. 1995. 82:1169–1180.
Article8. Han J, Davis SS, Washington C. Physical properties and stability of two emulsion formulations of propofol. Int J Pharm. 2001. 215:207–220.
Article9. Kim KM, Choi BM, Park SW, Lee SH, Christensen LV, Zhou J, et al. Pharmacokinetics and pharmacodynamics of propofol microemulsion and lipid emulsion after an intravenous bolus and variable rate infusion. Anesthesiology. 2007. 106:924–934.
Article10. Morey TE, Modell JH, Shekhawat D, Grand T, Shah DO, Gravenstein N, et al. Preparation and anesthetic properties of propofol microemulsions in rats. Anesthesiology. 2006. 104:1184–1190.
Article11. Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology. 1997. 86:10–23.
Article12. Annadata R, Sessler DI, Tayefeh F, Kurz A, Dechert M. Desflurane slightly increases the sweating threshold but produces marked, nonlinear decreases in the vasoconstriction and shivering thresholds. Anesthesiology. 1995. 83:1205–1211.
Article13. Ikeda T, Sessler DI, Kikura M, Kazama T, Ikeda K, Sato S. Less core hypothermia when anesthesia is induced with inhaled sevoflurane than with intravenous propofol. Anesth Analg. 1999. 88:921–924.
Article14. Iwata T, Inoue S, Kawaguchi M, Takahashi M, Sakamoto T, Kitaguchi K, et al. Comparison of the effects of sevoflurane and propofol on cooling and rewarming during deliberate mild hypothermia for neurosurgery. Br J Anaesth. 2003. 90:32–38.
Article15. Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008. 109:318–338.
Article16. Kurz A, Plattner O, Sessler DI, Huemer G, Redl G, Lackner F. The threshold for thermoregulatory vasoconstriction during nitrous oxide/isoflurane anesthesia is lower in elderly than in young patients. Anesthesiology. 1993. 79:465–469.
Article17. Elliott P, O'Hare R, Bill KM, Phillips AS, Gibson FM, Mirakhur RK. Severe cardiovascular depression with remifentanil. Anesth Analg. 2000. 91:58–61.
Article18. Komatsu R, Turan AM, Orhan-Sungur M, McGuire J, Radke OC, Apfel CC. Remifentanil for general anaesthesia: a systematic review. Anaesthesia. 2007. 62:1266–1280.
Article19. Kus V, Prazak T, Brauner P, Hensler M, Kuda O, Flachs P, et al. Induction of muscle thermogenesis by high-fat diet in mice: association with obesity-resistance. Am J Physiol Endocrinol Metab. 2008. 295:E356–E367.
Article20. Jessen K. An assessment of human regulatory nonshivering thermogenesis. Acta Anaesthesiol Scand. 1980. 24:138–143.
Article21. Vaillancourt E, Haman F, Weber JM. Fuel selection in Wistar rats exposed to cold: shivering thermogenesis diverts fatty acids from re-esterification to oxidation. J Physiol. 2009. 587:4349–4359.
Article22. Selldén E, Lindahl SG. Amino acid-induced thermogenesis reduces hypothermia during anesthesia and shortens hospital stay. Anesth Analg. 1999. 89:1551–1556.
Article23. Kasai T, Nakajima Y, Matsukawa T, Ueno H, Sunaguchi M, Mizobe T. Effect of preoperative amino acid infusion on thermoregulatory response during spinal anaesthesia. Br J Anaesth. 2003. 90:58–61.
Article24. Gottschling S, Meyer S, Krenn T, Kleinschmidt S, Reinhard H, Graf N, et al. Effects of short-term propofol administration on pancreatic enzymes and triglyceride levels in children. Anaesthesia. 2005. 60:660–663.
Article25. Jagla A, Schrezenmeir J. Postprandial triglycerides and endothelial function. Exp Clin Endocrinol Diabetes. 2001. 109:S533–S547.
Article26. Gosmanov AR, Smiley DD, Robalino G, Siquiera J, Khan B, Le NA, et al. Effects of oral and intravenous fat load on blood pressure, endothelial function, sympathetic activity, and oxidative stress in obese healthy subjects. Am J Physiol Endocrinol Metab. 2010. 299:E953–E958.
Article27. Belani K, Sessler DI, Sessler AM, Schroeder M, McGuire J, Merrifield B, et al. Leg heat content continues to decrease during the core temperature plateau in humans anesthetized with isoflurane. Anesthesiology. 1993. 78:856–863.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevention of pain during injection of microemulsion propofol: application of lidocaine mixture and the optimal dose of lidocaine
- Comparison of the effects of sevoflurane and propofol on core body temperature during laparoscopic abdominal surgery
- Effect of Inhaled Sevoflurane and Intravenous Propofol with Remifentanil on the Core Body Temperature in Burn Patients
- Correction of target-controlled infusion following wrong selection of emulsion concentrations of propofol
- Difference in Core temperature in response to propofol-remifentanil anesthesia and sevoflurane-remifentanil anesthesia