J Korean Med Sci.
2009 Aug;24(4):708-714. 10.3346/jkms.2009.24.4.708.
Changes of Ocular Version with Aging in Normal Korean Population
- Affiliations
-
- 1Department of Ophthalmology & Visual Science, Holy Family Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. nyeokang@catholic.ac.kr
- KMID: 1779208
- DOI: http://doi.org/10.3346/jkms.2009.24.4.708
Abstract
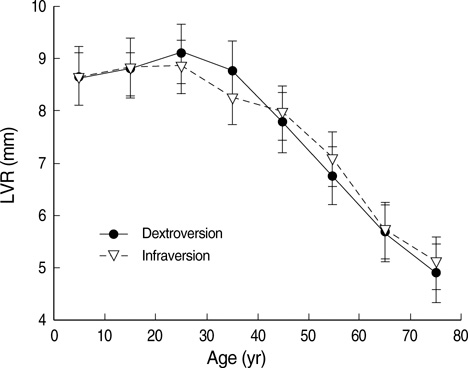
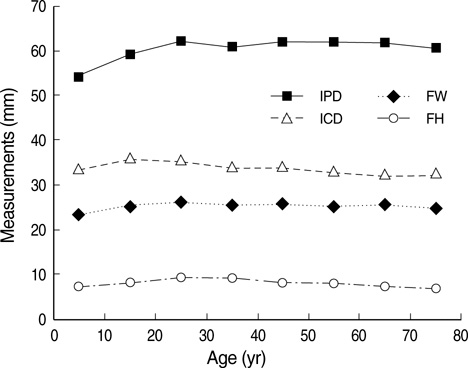
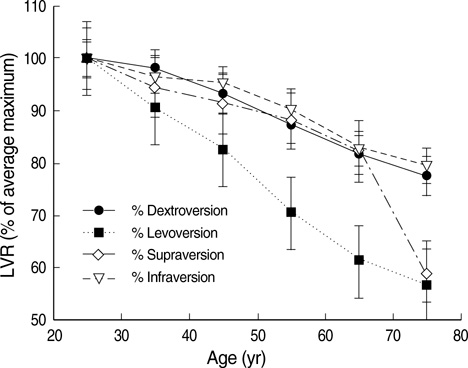
- The purpose of this study is to estimate normative values of maximum versions in healthy Koreans and investigate age-associated changes in eye movement, using lateral and vertical version light-reflex (LVR) test. Two hundred forty normal healthy subjects whose corrected visual acuity was better than 20/50 in both eyes, from 4 to 79 yr old (30 subjects in each decade) were studied. Maximum sustained values of dextroversion, levoversion, supraversion, and infraversion in each eye were measured using LVR test. Changes of versions according to age were analyzed. Mean normal value of dextroversion, levoversion, supraversion, and infraversion in normal Koreans was 7.7 mm, 41.6degrees, 33.9degrees, and 7.7 mm respectively. Contrary to values of Caucasians, levoversion (adductive movement) was more excessive and infraversion (depression) was smaller in Koreans. All versions were decreased with aging (P<0.001 for all). Levoversion had the largest decrease with aging compared with other versions (P<0.001, respectively) and infraversion had the least decrease with age than levoversion (P<0.001), supraversion (P<0.001). All maximal sustained versions were decreased with aging but the ranges of ocular movements in Koreans were different with Caucasians as version least affected and most affected by age was infraversion and levoversion in Koreans. The study standardized normal maximal versions and aging changes of versions in Koreans.
MeSH Terms
Figure
Reference
-
1. Von Noorden GK. Von Noorden GK, Campos EC, editors. Examination of the patient-II. Binocular vision and ocular motility: Theory and management of Strabismus. 2002. 6th ed. St Louis: Mosby;199–200.2. Guibor GP. Squint and allied conditions. 1959. New York: Grune & Stratton;28.3. Kestenbaum A. The clinical methods of neuro-ophthalmologic examination. 1961. 2nd ed. New York: Grune & Stratton;237.4. Urist MJ. A lateral version light-reflex test. Am J Ophthalmol. 1967. 63:808–815.
Article5. Urist MJ. Midline vertical versions in paretic deviations measured by a vertical version light-reflex test. Am J Ophthalmol. 1967. 64:253–260.6. Urist MJ. A lateral version light-reflex test. II. Value in the study of lateral rectus muscle palsy. Am J Ophthalmol. 1967. 64:70–77.7. Ziffer AJ, Isenberg SJ, Elliott RL, Apt L. The effect of anterior transposition of the inferior oblique muscle. Am J Ophthalmol. 1993. 116:224–227.
Article8. Hanada AL, De Souza EN Jr, Moribe I, Curze AA. Comparison of palpebral fissure obliquity in three different racial groups. Ophthal Plast Reconstr Surg. 2001. 17:423–426.
Article9. Kang JS. Plastic surgery. 2004. 3rd ed. Seoul: Koonja;865–866.10. Kono R, Poukens V, Demer JL. Quantitative analysis of the structure of the human extraocular muscle pulley system. Invest Ophthalmol Vis Sci. 2002. 43:2923–2932.11. Sharpe JA, Sylvester TO. Effect of aging on horizontal smooth pursuit. Invest Ophthalmol Vis Sci. 1978. 17:465–468.12. Spooner JW, Sakala SM, Baloh RW. Effect of aging on eye tracking. Arch Neurol. 1980. 37:575–576.
Article13. Chamberlain W. Restriction in upward gaze with advancing age. Am J Ophthalmol. 1971. 1:341–346.
Article14. Yamashiro M. Objective measurement of the limit of uniocular movement. Jpn J Ophthalmol. 1957. 1:130–135.15. Oguro H, Okada K, Suyama N, Yamashita K, Yamaguchi S, Kobayashi S. Decline of vertical gaze and convergence with aging. Gerontology. 2004. 50:177–181.
Article16. Clark RA, Isenberg SJ. The range of ocular movements decreases with aging. J AAPOS. 2001. 5:26–30.
Article17. Koh HJ, Yoo JM. The amounts of horizontal ocular movement in Korean people and comparison according to methods of measurement. J Korean Ophthalmol Soc. 2003. 44:1370–1375.18. Clark RA, Demer JL. Effect of aging on human rectus extraocular muscle paths demonstrated by magnetic resonance imaging. Am J Ophthalmol. 2002. 134:872–878.
Article19. Del Monte MA, Richard JM, Mets MB, Wilson ME, Wight KW. Denny M, editor. Section 6: Pediatric ophthalmology and strabismus. Basic and Clinical Science Course. 1994. Vol 6. San Fransisco: American Academy of Ophthalmology;237–277.20. Park DM, Song JW, Han KH, Kang JS. Anthropometry of normal Korean eyelids. J Korean Soc Plast Reconstr Surg. 1990. 17:822–834.21. Kim CJ, Han KS, Kim Y, Cho YJ. A facial anthropometric study on the Korean youths. J Korean Soc Plast Reconstr Surg. 1988. 15:427–436.22. Oh SJ, Koh IC, Lee YH, Lew JD. Somatometric study on the face of the Korean. J Korean Soc Plast Reconstr Surg. 1975. 2:15–22.23. Cho JH, Han KH, Kang JS. Normal anthropometric values and standardized templates of Korean face and head. J Korean Soc Plast Reconstr Surg. 1993. 20:995–1004.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Amounts of Horizontal Ocular Movement in Korean People and Comparison According to Methods of Measurement
- Range of Eye Movement in a Normal Population and Its Relationship to Age
- Changes Seen on Echocardiography in Elderly Population
- Aging and Ocular Dimensions
- Can we rejuvenate? Implications of biological aging research