Patient-controlled Epidural Analgesia with Ropivacaine and Fentanyl: Experience with 2,276 Surgical Patients
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea. ysshin@yuhs.ac
- KMID: 1779022
- DOI: http://doi.org/10.3344/kjp.2013.26.1.39
Abstract
- BACKGROUND
Good postoperative pain control is an important part of adequate postoperative care. Patient-controlled epidural analgesia (PCEA) provided better postoperative analgesia compared to other conventional analgesic methods, but several risks have been observed as well. We therefore surveyed the efficacy and safety of PCEA in this retrospective observational study.
METHODS
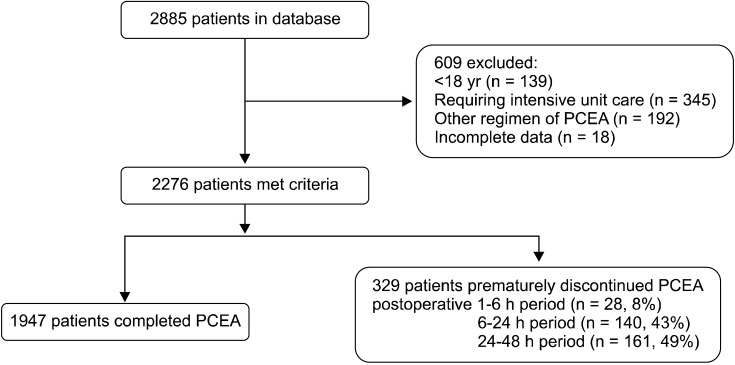
We analyzed collected data on 2,276 elective surgical patients who received PCEA with ropivacaine and fentanyl. Patients were assessed by a PCA service team in the post-anesthesia care unit (PACU), at 1-6 h, 6-24 h, and 24-48 h postoperatively for adequate pain control. The presence of PCEA-related adverse events was also assessed.
RESULTS
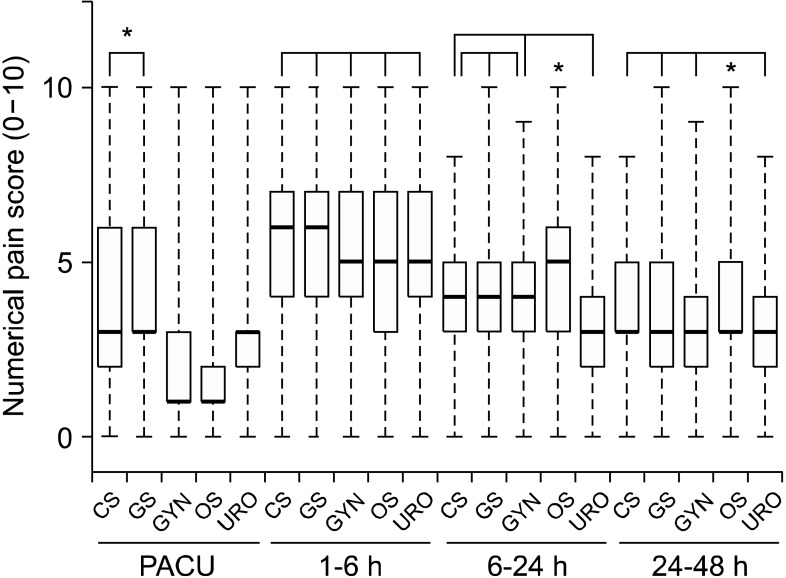
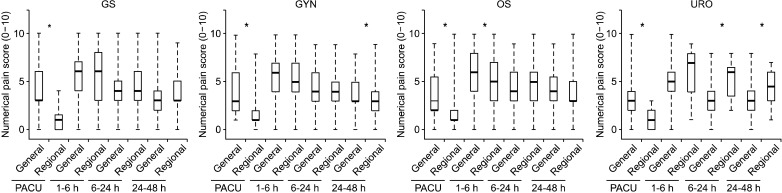
Numerical pain score (median [interquartile range]) were 3 [1-4], 5 [4-7], 4 [3-5], and 3 [3-5] in the PACU, at 1-6 h, 6-24 h, and 24-48 h postoperatively. Median pain scores in patients underwent major abdominal or thoracic surgery were higher than other surgical procedure in the PACU, at 1-6 h after surgery. Nausea and vomiting (20%) and numbness and motor weakness (15%) were revealed as major PCEA-related adverse events during the postoperative 48 h period. There were 329 patients (14%) for whom PCEA was ceased within 48 h following surgery.
CONCLUSIONS
Our data suggest that the use of PCEA provides proper analgesia in the postoperative 48 h period after a wide variety of surgical procedures and that is associated with few serious complications. However, more careful pain management and sustainable PCEA monitoring considering the type of surgical procedure undergone is needed in patients with PCEA.
MeSH Terms
Figure
Cited by 4 articles
-
Evaluation of the Efficacy of Methylprednisolone, Etoricoxib and a Combination of the Two Substances to Attenuate Postoperative Pain and PONV in Patients Undergoing Laparoscopic Cholecystectomy: A Prospective, Randomized, Placebo-controlled Trial
Sujeet Gautam, Amita Agarwal, Pravin Kumar Das, Anil Agarwal, Sanjay Kumar, Sandeep Khuba
Korean J Pain. 2014;27(3):278-284. doi: 10.3344/kjp.2014.27.3.278.The Impact of Educational Status on the Postoperative Perception of Pain
Sophocles Lanitis, Christina Mimigianni, Demetris Raptis, Gionous Sourtse, George Sgourakis, Constantine Karaliotas
Korean J Pain. 2015;28(4):265-274. doi: 10.3344/kjp.2015.28.4.265.Analysis of thoracic epidurography and correlating factors affecting the extent of contrast medium spread
Ji Hee Hong, Jung Hue Oh, Ki Bum Park
Korean J Pain. 2016;29(4):255-261. doi: 10.3344/kjp.2016.29.4.255.Allopregnanolone suppresses mechanical allodynia and internalization of neurokinin-1 receptors at the spinal dorsal horn in a rat postoperative pain model
Masahide Fujita, Taeko Fukuda, Yasuhiro Sato, Toshifumi Takasusuki, Makoto Tanaka
Korean J Pain. 2018;31(1):10-15. doi: 10.3344/kjp.2018.31.1.10.
Reference
-
1. Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Br J Anaesth. 2001; 87:62–72. PMID: 11460814.
Article2. Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003; 97:534–540. PMID: 12873949.
Article3. Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA Jr, Wu CL. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA. 2003; 290:2455–2463. PMID: 14612482.4. Liu S, Carpenter RL, Neal JM. Epidural anesthesia and analgesia. Their role in postoperative outcome. Anesthesiology. 1995; 82:1474–1506. PMID: 7793661.5. Kim DH. Effective continuous infusion and bolus doses for patient-controlled epidural analgesia using ropivacaine. J Korean Pain Soc. 2002; 15:75–79.6. Pöpping DM, Zahn PK, Van Aken HK, Dasch B, Boche R, Pogatzki-Zahn EM. Effectiveness and safety of postoperative pain management: a survey of 18 925 consecutive patients between 1998 and 2006 (2nd revision): a database analysis of prospectively raised data. Br J Anaesth. 2008; 101:832–840. PMID: 18945716.
Article7. Chen PP, Chui PT, Ma M, Gin T. A prospective survey of patients after cessation of patient-controlled analgesia. Anesth Analg. 2001; 92:224–227. PMID: 11133632.
Article8. Liu SS, Allen HW, Olsson GL. Patient-controlled epidural analgesia with bupivacaine and fentanyl on hospital wards: prospective experience with 1,030 surgical patients. Anesthesiology. 1998; 88:688–695. PMID: 9523813.
Article9. Scott DA, Beilby DS, McClymont C. Postoperative analgesia using epidural infusions of fentanyl with bupivacaine. A prospective analysis of 1,014 patients. Anesthesiology. 1995; 83:727–737. PMID: 7574052.10. de Leon-Casasola OA, Parker B, Lema MJ, Harrison P, Massey J. Postoperative epidural bupivacaine-morphine therapy. Experience with 4,227 surgical cancer patients. Anesthesiology. 1994; 81:368–375. PMID: 8053587.
Article11. Cha YD, Song JH, Song JH, Kim TJ, Lee HS, Lee CS, et al. Is initial loading dose necessary for continuous epidural analgesia after brief surgery? J Korean Pain Soc. 2000; 13:44–48.12. Brennum J, Arendt-Nielsen L, Secher NH, Jensen TS, Bjerring P. Quantitative sensory examination in human epidural anaesthesia and analgesia: effects of lidocaine. Pain. 1992; 51:27–34. PMID: 1454401.
Article13. Liu SS, Moore JM, Luo AM, Trautman WJ, Carpenter RL. Comparison of three solutions of ropivacaine/fentanyl for postoperative patient-controlled epidural analgesia. Anesthesiology. 1999; 90:727–733. PMID: 10078673.
Article14. Moon DE, Shim JY, Lim YG, Kim YS, Kim BC, Kim SN. Neurologic complications following epidural analgesia. J Korean Pain Soc. 1997; 10:291–295.15. Talu GK, Erdine S. Complications of epidural neuroplasty: a retrospective evaluation. Neuromodulation. 2003; 6:237–247. PMID: 22151070.
Article16. Visser WA, Lee RA, Gielen MJ. Factors affecting the distribution of neural blockade by local anesthetics in epidural anesthesia and a comparison of lumbar versus thoracic epidural anesthesia. Anesth Analg. 2008; 107:708–721. PMID: 18633056.
Article17. Burstal R, Wegener F, Hayes C, Lantry G. Epidural analgesia: prospective audit of 1062 patients. Anaesth Intensive Care. 1998; 26:165–172. PMID: 9564395.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A comparison of 0.075% and 0.15% of ropivacaine with fentanyl for postoperative patient controlled epidural analgesia after laparoscopic gynecologic surgery
- Small Dose of Midazolam Added to Fentanyl-Ropivacaine for Patient Controlled Epidural Analgesia after Subtotal Gastrectomy
- Comparison of Sufentanil and Fentanyl Added to Ropivacaine for Patient-Controlled Thoracic Epidural Analgesia
- A Double-blind Comparison of 0.125% Ropivacaine with Fentanyl and 0.125% Bupivacine with Fentanyl for Labor Analgesia Using Patient-Controlled Epidural Infusion
- Comparison of 0.15% Ropivacaine/Fentanyl and 0.1% Levobupivacaine/Fentanyl Infused for Postoperative Epidural Analgesia