Korean J Pain.
2012 Apr;25(2):112-115. 10.3344/kjp.2012.25.2.112.
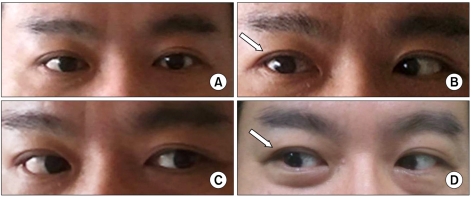
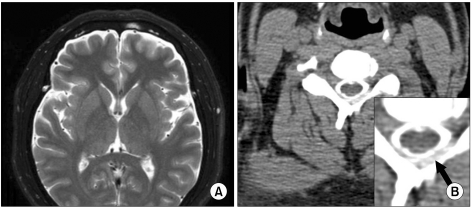
Epidural Blood Patch for the Treatment of Abducens Nerve Palsy due to Spontaneous Intracranial Hypotension: A Case Report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Yonsei University Health System, Seoul, Korea. kbyoon@yuhs.ac
- 2Anesthesia and Pain Research Institute, Yonsei University Health System, Seoul, Korea.
- KMID: 1778996
- DOI: http://doi.org/10.3344/kjp.2012.25.2.112
Abstract
- Intracranial hypotension is characterized by a postural headache which is relieved in a supine position and worsened in a sitting or standing position. Although less commonly reported than postural headache, sixth nerve palsy has also been observed in intracranial hypotension. The epidural blood patch (EBP) has been performed for postdural puncture headache, but little is known about the proper timing of EBP in the treatment of sixth nerve palsy due to intracranial hypotension. This article reports a case of sixth nerve palsy due to spontaneous intracranial hypotension which was treated by EBP 10 days after the onset of palsy.
MeSH Terms
Figure
Cited by 1 articles
-
Epidural blood patch treatment of diplopia that developed after headache resolution in a patient with spontaneous intracranial hypotension
Myung-Su Lee, Sookyung Lee, Dong-Kyun Seo, Syn-Hae Yoon, Seong-Soo Choi
J Dent Anesth Pain Med. 2018;18(4):255-259. doi: 10.17245/jdapm.2018.18.4.255.
Reference
-
1. Schievink WI, Dodick DW, Mokri B, Silberstein S, Bousser MG, Goadsby PJ. Diagnostic criteria for headache due to spontaneous intracranial hypotension: a perspective. Headache. 2011; 51:1442–1444. PMID: 21658029.
Article2. Schwedt TJ, Dodick DW. Spontaneous intracranial hypotension. Curr Pain Headache Rep. 2007; 11:56–61. PMID: 17214923.
Article3. Zada G, Solomon TC, Giannotta SL. A review of ocular manifestations in intracranial hypotension. Neurosurg Focus. 2007; 23:E8. PMID: 18004970.
Article4. Nishio I, Williams BA, Williams JP. Diplopia: a complication of dural puncture. Anesthesiology. 2004; 100:158–164. PMID: 14695737.5. Koeppen AH. Abducens palsy after lumbar puncture. Proc Wkly Semin Neurol. 1967; 17:68–76. PMID: 4907858.6. Schober P, Loer SA, Schwarte LA. Paresis of cranial nerve VI (N. abducens) after thoracic dural perforation. Minerva Anestesiol. 2010; 76:1085–1087. PMID: 20838373.7. Béchard P, Perron G, Larochelle D, Lacroix M, Labourdette A, Dolbec P. Case report: epidural blood patch in the treatment of abducens palsy after a dural puncture. Can J Anaesth. 2007; 54:146–150. PMID: 17272255.
Article8. Kim KS, Lee DI, Kang WJ, Shin OY, Kwon MI. A case of cervical epidural blood patch for treatment of spontaneous intracranial hypotension. J Korean Pain Soc. 2002; 15:198–203.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed-Onset Subdural Hematoma and Oculomotor Nerve Palsy After Improving Spontaneous Intracranial Hypotension
- Abducens Nerve Palsy in Patient with Intracranial Hypotension After SpineSurgery
- Epidural blood patch treatment of diplopia that developed after headache resolution in a patient with spontaneous intracranial hypotension
- A Case of Spontaneous Intracranial Hypotension presented as Bilateral Abducens Nerve Palsy without Postural Headache
- Intracranial Hypertension Following Epidural Blood Patch in a Patient With Spontaneous Intracranial Hypotension