J Korean Med Sci.
2009 Jan;24(Suppl 1):S129-S134. 10.3346/jkms.2009.24.S1.S129.
Minimal Proteinuria One Year after Transplant is a Risk Factor for Graft Survival in Kidney Transplantation
- Affiliations
-
- 1Division of Nephrology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. hayoung.oh@samsung.com
- 2Division of Transplantation Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1778152
- DOI: http://doi.org/10.3346/jkms.2009.24.S1.S129
Abstract
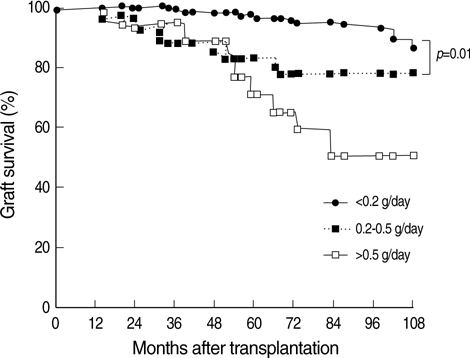
- It is generally accepted that one-year post-transplant proteinuria over 0.5 gm per day has a negative impact on renal graft survival. In this study, the effects of minimal proteinuria less than 0.5 g/day were analyzed in 272 renal recipients who had survived for one year with a functioning graft. Recipients were classified by one-year posttransplant proteinuria: no proteinuria group (<0.2 g/day), minimal proteinuria group (0.2-0.5 g/day), and overt proteinuria group (> or =0.5 g/day). Recipients were followed up for 87.1+/-21 months after transplantation and 38 (13.9%) lost their graft during follow-up. Fifteen percent of patients had minimal proteinuria and 7.8% had overt proteinuria. Five-year graft survival in the minimal proteinuria group was 83.0%, and that in the overt proteinuria group was 70%, in contrast to 97.1% in the no proteinuria group (p=0.01 for trend). In a multivariate analysis, the minimal proteinuria group (relative risk [RR], 4.90; 95% confidence interval [CI], 2.09-11.46) and the overt proteinuria group (RR, 8.75; 95% CI, 3.29-23.29) had higher risks of graft failure than the no proteinuria group. Even minimal proteinuria at one year after transplantation was strongly associated with poor graft outcome. Therefore, it appears logical to consider a low level of proteinuria as a risk factor for graft survival in renal recipients.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Improved Gastrointestinal Symptoms and Quality of Life after Conversion from Mycophenolate Mofetil to Enteric-Coated Mycophenolate Sodium in Renal Transplant Patients Receiving Tacrolimus
Hyeon Seok Hwang, Bok Jin Hyoung, Sol Kim, Ha Young Oh, Yon Su Kim, Jung Kyung Kim, Yeong Hoon Kim, Yong Lim Kim, Chan Duck Kim, Gyu Tae Shin, Chul Woo Yang
J Korean Med Sci. 2010;25(12):1759-1765. doi: 10.3346/jkms.2010.25.12.1759.
Reference
-
1. Hariharan S, Johnson CP, Bresnahan BA, Taranto SE, McIntosh MJ, Stablein D. Improved graft survival after renal transplantation in the United States, 1988 to 1996. N Engl J Med. 2000. 342:605–612.
Article2. Nankivell BJ, Borrows RJ, Fung CL, O'Connell PJ, Allen RD, Chapman JR. The natural history of chronic allograft nephropathy. N Engl J Med. 2003. 349:2326–2333.
Article3. Roodnat JI, Mulder PG, Rischen-Vos J, van Riemsdijk IC, van Gelder T, Zietse R, IJzermans JN, Weimar W. Proteinuria after renal transplantation affects not only graft survival but also patient survival. Transplantation. 2001. 72:438–444.
Article4. Fernandez-Fresnedo G, Escallada R, Rodrigo E, De Francisco AL, Cotorruelo JG, Sanz De Castro S, Zubimendi JA, Ruiz JC, Arias M. The risk of cardiovascular disease associated with proteinuria in renal transplant patients. Transplantation. 2002. 73:1345–1348.
Article5. Fernández-Fresnedo G, Plaza JJ, Sánchez-Plumed J, Sanz-Guajardo A, Palomar-Fontanet R, Arias M. Proteinuria: a new marker of long-term graft and patient survival in kidney transplantation. Nephrol Dial Transplant. 2004. 19:Suppl 3. iii47–iii51.6. K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004. 43:5 Suppl 1. S1–S290.7. Heinze G, Mitterbauer C, Regele H, Kramar R, Winkelmayer WC, Curhan GC, Oberbauer R. Angiotensin-converting enzyme inhibitor or angiotensin II type 1 receptor antagonist therapy is associated with prolonged patient and graft survival after renal transplantation. J Am Soc Nephrol. 2006. 17:889–899.
Article8. de Zeeuw D. Albuminuria, not only a cardiovascular/renal risk marker, but also a target for treatment? Kidney Int Suppl. 2004. S2–S6.
Article9. Ruggenenti P, Perna A, Remuzzi G. Retarding progression of chronic renal disease: the neglected issue of residual proteinuria. Kidney Int. 2003. 63:2254–2261.
Article10. Sulanc E, Lane JT, Puumala SE, Groggel GC, Wrenshall LE, Stevens RB. New-onset diabetes after kidney transplantation: an application of 2003 International Guidelines. Transplantation. 2005. 80:945–952.
Article11. Gaspari F, Ferrari S, Stucchi N, Centemeri E, Carrara F, Pellegrino M, Gherardi G, Gotti E, Segoloni G, Salvadori M, Rigotti P, Valente U, Donati D, Sandrini S, Sparacino V, Remuzzi G, Perico N. Performance of different prediction equations for estimating renal function in kidney transplantation. Am J Transplant. 2004. 4:1826–1835.
Article12. Poggio ED, Wang X, Weinstein DM, Issa N, Dennis VW, Braun WE, Hall PM. Assessing glomerular filtration rate by estimation equations in kidney transplant recipients. Am J Transplant. 2006. 6:100–108.
Article13. Massy ZA, Guijarro C, Wiederkehr MR, Ma JZ, Kasiske BL. Chronic renal allograft rejection: immunologic and nonimmunologic risk factors. Kidney Int. 1996. 49:518–524.
Article14. Hohage H, Kleyer U, Bruckner D, August C, Zidek W, Spieker C. Influence of proteinuria on long-term transplant survival in kidney transplant recipients. Nephron. 1997. 75:160–165.
Article15. Halimi JM, Laouad I, Buchler M, Al-Najjar A, Chatelet V, Houssaini TS, Nivet H, Lebranchu Y. Early low-grade proteinuria: causes, short-term evolution and long-term consequences in renal transplantation. Am J Transplant. 2005. 5:2281–2288.
Article16. Halimi JM, Buchler M, Al-Najjar A, Laouad I, Chatelet V, Marliere JF, Nivet H, Lebranchu Y. Urinary albumin excretion and the risk of graft loss and death in proteinuric and non-proteinuric renal transplant recipients. Am J Transplant. 2007. 7:618–625.
Article17. Dinneen SF, Gerstein HC. The association of microalbuminuria and mortality in non-insulin-dependent diabetes mellitus. A systematic overview of the literature. Arch Intern Med. 1997. 157:1413–1418.
Article18. Keane WF, Brenner BM, de Zeeuw D, Grunfeld JP, McGill J, Mitch WE, Ribeiro AB, Shahinfar S, Simpson RL, Snapinn SM, Toto R. The risk of developing end-stage renal disease in patients with type 2 diabetes and nephropathy: the RENAAL study. Kidney Int. 2003. 63:1499–1507.
Article19. Palatini P, Mormino P, Dorigatti F, Santonastaso M, Mos L, De Toni R, Winnicki M, Dal Follo M, Biasion T, Garavelli G, Pessina AC. Glomerular hyperfiltration predicts the development of microalbuminuria in stage 1 hypertension: the HARVEST. Kidney Int. 2006. 70:578–584.
Article20. Gross ML, Hanke W, Koch A, Ziebart H, Amann K, Ritz E. Intraperitoneal protein injection in the axolotl: the amphibian kidney as a novel model to study tubulointerstitial activation. Kidney Int. 2002. 62:51–59.
Article21. Rosenkranz AR, Mayer G. Proteinuria in the transplanted patient. Nephrol Dial Transplant. 2000. 15:1290–1292.
Article22. Kasiske BL, Guijarro C, Massy ZA, Wiederkehr MR, Ma JZ. Cardiovascular disease after renal transplantation. J Am Soc Nephrol. 1996. 7:158–165.
Article23. Kasiske BL, Vazquez MA, Harmon WE, Brown RS, Danovitch GM, Gaston RS, Roth D, Scandling JD, Singer GG. Recommendations for the outpatient surveillance of renal transplant recipients. American Society of Transplantation. J Am Soc Nephrol. 2000. 11:Suppl 15. S1–S86.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association of posttransplantation proteinuria with allograft loss in transplant kidney biopsy-proven recipients
- The Outcome and Risk Factors of Renal Retransplantation
- Outcome of living donor kidney transplant and deceased donor kidney transplant: a retrospective cohort study at national kidney and transplant institute
- The Effect of Hypercholesterolemia and Hypertension on Long-term Renal Allograft Survival
- Risk of graft loss on once-daily versus twice-daily tacrolimus in kidney transplant patients: a meta-analysis