J Korean Med Sci.
2013 Oct;28(10):1461-1467. 10.3346/jkms.2013.28.10.1461.
Association between Central Obesity and Circadian Parameters of Blood Pressure from the Korean Ambulatory Blood Pressure Monitoring Registry: Kor-ABP Registry
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, School of Medicine, Ewha Womans University, Seoul, Korea. pwb423@ewha.ac.kr
- 2Division of Cardiology, Department of Internal Medicine, School of Medicine, Hanyang University, Seoul, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 1777682
- DOI: http://doi.org/10.3346/jkms.2013.28.10.1461
Abstract
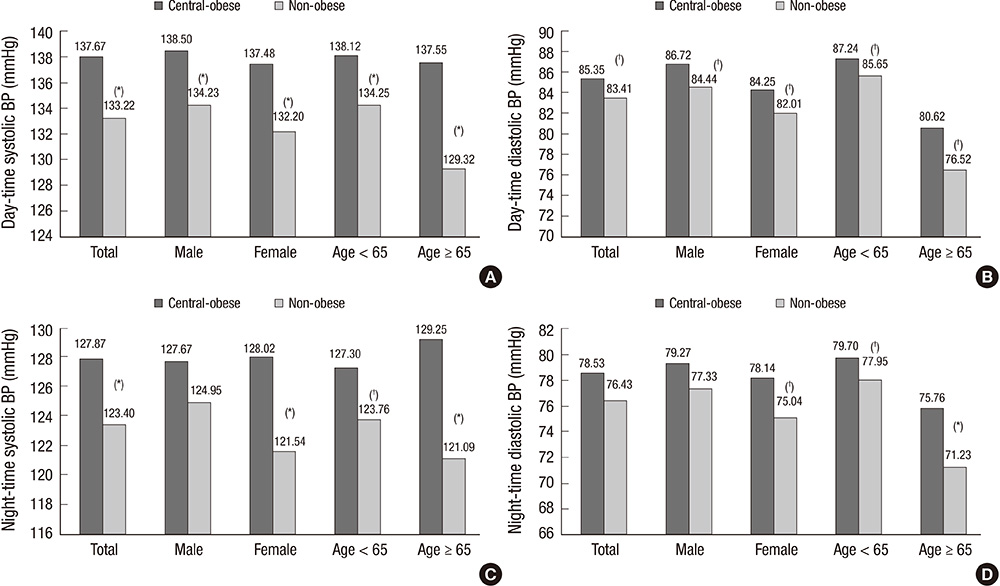
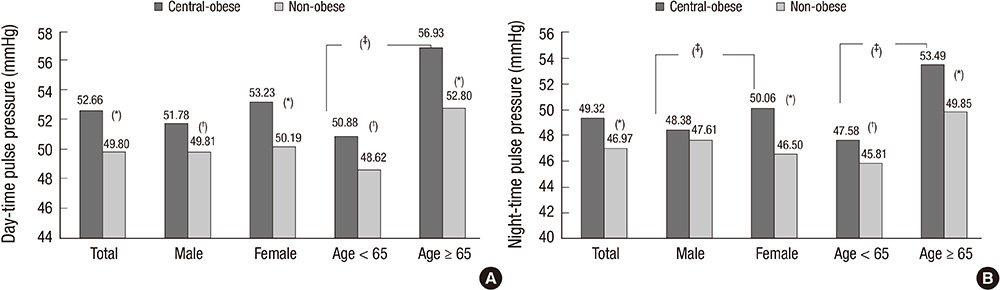
- Central obesity has been reported as a risk for atherosclerosis and metabolic syndrome. The influence of central obesity on diurnal blood pressure (BP) has not been established. In this study, we investigated the influence of central obesity on the circadian parameters of BP by 24 hr ambulatory BP monitoring. Total 1,290 subjects were enrolled from the Korean Ambulatory BP registry. Central obesity was defined as having a waist circumference> or =90 cm in males and > or =85 cm in females. The central-obese group had higher daytime systolic BP (SBP), nighttime SBP and diastolic BP (DBP) than the non-obese group (all, P<0.001). There were no differences in nocturnal dipping (ND) patterns between the groups. Female participants showed a higher BP mean difference (MD) than male participants with concerns of central obesity (daytime SBP MD 5.28 vs 4.27, nighttime SBP MD 6.48 vs 2.72) and wider pulse pressure (PP). Central obesity within the elderly (> or =65 yr) also showed a higher BP MD than within the younger group (daytime SBP MD 8.23 vs 3.87, daytime DBP 4.10 vs 1.59). In conclusion, central obesity has no influence on nocturnal dipping patterns. However, higher SBP and wider PP are associated with central obesity, which is accentuated in women.
MeSH Terms
-
Adult
Age Factors
Aged
Asian Continental Ancestry Group
Blood Pressure/physiology
*Blood Pressure Monitoring, Ambulatory
Circadian Rhythm/*physiology
Female
Humans
Hypertension/*complications/epidemiology
Male
Middle Aged
Obesity, Abdominal/*complications/*epidemiology/pathology
Registries
Republic of Korea/epidemiology
Sex Factors
Waist Circumference
Figure
Reference
-
1. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003; 289:2560–2572.2. Verdecchia P, Schillaci G, Borgioni C, Ciucci A, Pede S, Porcellati C. Ambulatory pulse pressure: a potent predictor of total cardiovascular risk in hypertension. Hypertension. 1998; 32:983–988.3. Franklin SS, Khan SA, Wong ND, Larson MG, Levy D. the Framingham Heart Study. Is pulse pressure useful in predicting risk for coronary heart Disease? Circulation. 1999; 100:354–360.4. Vaccarino V, Berger AK, Abramson J, Black HR, Setaro JF, Davey JA, Krumholz HM. Pulse pressure and risk of cardiovascular events in the systolic hypertension in the elderly program. Am J Cardiol. 2001; 88:980–986.5. Franklin SS, Gustin W 4th, Wong ND, Larson MG, Weber MA, Kannel WB, Levy D. Hemodynamic patterns of age-related changes in blood pressure: the Framingham Heart Study. Circulation. 1997; 96:308–315.6. Pi-Sunyer FX. Medical hazards of obesity. Ann Intern Med. 1993; 119:655–660.7. Hu FB. Overweight and obesity in women: health risks and consequences. J Womens Health (Larchmt). 2003; 12:163–172.8. Holecki M, Dulawa J, Chudek J. Resistant hypertension in visceral obesity. Eur J Intern Med. 2012; 23:643–648.9. Drøyvold WB, Midthjell K, Nilsen TI, Holmen J. Change in body mass index and its impact on blood pressure: a prospective population study. Int J Obes (Lond). 2005; 29:650–655.10. Wilsgaard T, Schirmer H, Arnesen E. Impact of body weight on blood pressure with a focus on sex differences: the Tromso Study, 1986-1995. Arch Intern Med. 2000; 160:2847–2853.11. Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg. 2008; 207:928–934.12. Nordstrand N, Hertel JK, Hofsø D, Sandbu R, Saltvedt E, Røislien J, Os I, Hjelmesaeth J. A controlled clinical trial of the effect of gastric bypass surgery and intensive lifestyle intervention on nocturnal hypertension and the circadian blood pressure rhythm in patients with morbid obesity. Surgery. 2012; 151:674–680.13. Lee S, Park HS, Kim SM, Kwon HS, Kim DY, Kim DJ, Cho GJ, Han JH, Kim SR, Park CY, et al. Cut-off points of waist circumference for defining abdominal obesity in the Korean population. Korean J Obes. 2006; 15:1–9.14. Nishiyama A, Imai Y, Ohkubo T, Tsuji I, Nagai K, Kikuchi N, Kato J, Sekino M, Aihara A, Kikuya M, et al. Determinants of circadian blood pressure variation: a community-based study in Ohasama. Tohoku J Exp Med. 1997; 183:1–20.15. Kurukulasuriya LR, Stas S, Lastra G, Manrique C, Sowers JR. Hypertension in obesity. Med Clin North Am. 2011; 95:903–917.16. Lee HT, Lim YH, Kim BK, Lee KW, Lee JU, Kim KS, Kim SG, Kim JH, Lim HK, Shin J, et al. The relationship between ambulatory arterial stiffness index and blood pressure variability in hypertensive patients. Korean Circ J. 2011; 41:235–240.17. Nordstrand N, Gjevestad E, Dinh KN, Hofsø D, Røislien J, Saltvedt E, Os I, Hjelmesæth J. The relationship between various measures of obesity and arterial stiffness in morbidly obese patients. BMC Cardiovasc Disord. 2011; 11:7.18. Domanski M, Mitchell G, Pfeffer M, Neaton JD, Norman J, Svendsen K, Grimm R, Cohen J, Stamler J. MRFIT Research Group. Pulse pressure and cardiovascular disease-related mortality: follow-up study of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA. 2002; 287:2677–2683.19. Staessen JA, Thijs L, O'Brien ET, Bulpitt CJ, de Leeuw PW, Fagard RH, Nachev C, Palatini P, Parati G, Tuomilehto J, et al. Ambulatory pulse pressure as predictor of outcome in older patients with systolic hypertension. Am J Hypertens. 2002; 15:835–843.20. Khattar RS, Acharya DU, Kinsey C, Senior R, Lahiri A. Longitudinal association of ambulatory pulse pressure with left ventricular mass and vascular hypertrophy in essential hypertension. J Hypertens. 1997; 15:737–743.21. Ammar KA, Redfield MM, Mahoney DW, Johnson M, Jacobsen SJ, Rodeheffer RJ. Central obesity: association with left ventricular dysfunction and mortality in the community. Am Heart J. 2008; 156:975–981.22. Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gend Med. 2009; 6:60–75.23. Carey DG, Jenkins AB, Campbell LV, Freund J, Chisholm DJ. Abdominal fat and insulin resistance in normal and overweight women: direct measurements reveal a strong relationship in subjects at both low and high risk of NIDDM. Diabetes. 1996; 45:633–638.24. Ayala DE, Moyá A, Crespo JJ, Castiñeira C, Domínguez-Sardiña M, Gomara S, Sineiro E, Mojón A, Fontao MJ, Hermida RC. Circadian pattern of ambulatory blood pressure in hypertensive patients with and without type 2 diabetes. Chronobiol Int. 2013; 30:99–115.25. Hermida RC, Ayala DE, Fernández JR, Mojón A. Sleep-time blood pressure: prognostic value and relevance as a therapeutic target for cardiovascular risk reduction. Chronobiol Int. 2013; 30:68–86.26. Birkenhäger AM, van den Meiracker AH. Causes and consequences of a non-dipping blood pressure profile. Neth J Med. 2007; 65:127–131.27. Kario K, Schwartz JE, Pickering TG. Changes of nocturnal blood pressure dipping status in hypertensives by nighttime dosing of alpha-adrenergic blocker, doxazosin: results from the HALT Study. Hypertension. 2000; 35:787–794.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Significance of Nighttime Blood Pressure
- Diurnal Variation of Blood Pressure; the Difference between before and after Removal of Pheochromocytoma: Evaluation by Ambulatory Blood Pressure Monitoring
- The Cprrelation between LVH, LV Function and 24-hour Ambulatory Blood Pressure Monitoring in Patients with Newly Diagnosed Hypertension
- Office orthostatic blood pressure measurements and ambulatory blood pressure monitoring in the prediction of autonomic dysfunction
- Differing Impact of Weight Cycling on Ambulatory Blood Pressure versus Conventional Blood Pressure Assessment: A Possible Explanation to Controversy