J Korean Med Sci.
2013 May;28(5):693-699. 10.3346/jkms.2013.28.5.693.
Differentiated Thyroid Carcinoma of Children and Adolescents: 27-Year Experience in the Yonsei University Health System
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. jungjongj@yuhs.ac
- KMID: 1777556
- DOI: http://doi.org/10.3346/jkms.2013.28.5.693
Abstract
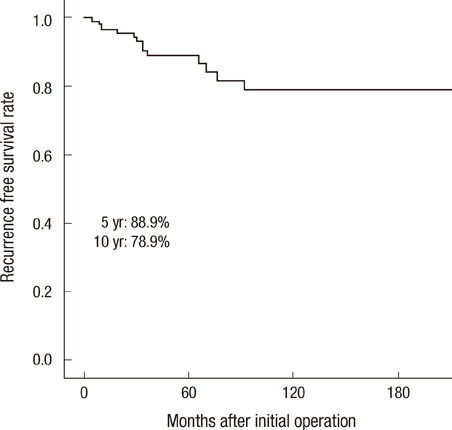
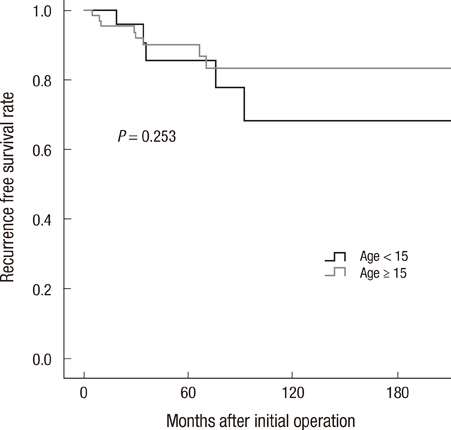
- Thyroid carcinomas are uncommon in childhood and adolescence. The aim of this study was to analyze clinical features and clinical outcomes of thyroid cancer in the pediatric population treated in the Yonsei University Health System. From September 1982 to June 2009, 90 patients (75 females, 15 males; female:male ratio of 5:1) with differentiated thyroid carcinoma were identified in our institute. The mean age at diagnosis was 15.8 yr old (range 4.8-19.9 yr). Cervical masses were most common clinical manifestations at diagnosis in 65 patients (72.2%). Forty-two patients underwent less than total thyroidectomy and 18 patients underwent total thyroidectomy. Thirty patients (33.3%) had lateral neck lymph node metastasis and seven patients (7.8%) had lung metastasis at the time of surgery. Among the 90 patients, recurrence occurred in 14 patients (15.5%). Mean follow-up period for patients with differentiated thyroid carcinoma was 81.6 months (13-324 months). No patients died of differentiated thyroid carcinoma. Patients with differentiated thyroid carcinoma who were < 20-yr-of-age were present with aggressive local disease and a high frequency of lymph node and distant metastasis. It is recommended that pediatric thyroid cancer should be managed mostly using proper surgical approach with thyroidectomy and lymph node dissection when indicated.
Keyword
MeSH Terms
-
Adolescent
Age Factors
Carcinoma/*pathology/surgery
Child
Child, Preschool
Female
Follow-Up Studies
Hospitals, University
Humans
Iodine Radioisotopes/therapeutic use
Lung Neoplasms/diagnosis/secondary
Lymph Node Excision
Lymph Nodes/surgery
Lymphatic Metastasis
Male
Recurrence
Survival Rate
Thyroid Neoplasms/*pathology/radiotherapy/surgery
Thyroidectomy
Young Adult
Iodine Radioisotopes
Figure
Cited by 1 articles
-
Usefulness of dynamic risk stratification in pediatric patients with differentiated thyroid carcinoma
Kwangsoon Kim, Won Woong Kim, Jung Bum Choi, Min Jhi Kim, Cho Rok Lee, Jandee Lee, Sang-Wook Kang, Kee-Hyun Nam, Woong Youn Chung, Jong Ju Jeong
Ann Surg Treat Res. 2018;95(4):222-229. doi: 10.4174/astr.2018.95.4.222.
Reference
-
1. Millman B, Pellitteri PK. Thyroid carcinoma in children and adolescents. Arch Otolaryngol Head Neck Surg. 1995. 121:1261–1264.2. Thompson GB, Hay ID. Current strategies for surgical management and adjuvant treatment of childhood papillary thyroid carcinoma. World J Surg. 2004. 28:1187–1198.3. Haveman JW, van Tol KM, Rouwé CW, Piers DA, Plukker JT. Surgical experience in children with differentiated thyroid carcinoma. Ann Surg Oncol. 2003. 10:15–20.4. Borson-Chazot F, Causeret S, Lifante JC, Augros M, Berger N, Peix JL. Predictive factors for recurrence from a series of 74 children and adolescents with differentiated thyroid cancer. World J Surg. 2004. 28:1088–1092.5. Howe HL, Wu X, Ries LA, Cokkinides V, Ahmed F, Jemal A, Miller B, Williams M, Ward E, Wingo PA, et al. Annual report to the nation on the status of cancer, 1975-2003, featuring cancer Hispanic/Latino populations. Cancer. 2006. 107:1711–1742.6. Chadha NK, Forte V. Pediatric head and neck malignancies. Curr Opin Otolaryngol Head Neck Surg. 2009. 17:471–476.7. La Quaglia MP, Corbally MT, Heller G, Exelby PR, Brennan MF. Recurrence and morbidity in differentiated thyroid carcinoma in children. Surgery. 1988. 104:1149–1156.8. Zimmerman D, Hay ID, Gough IR, Goellner JR, Ryan JJ, Grant CS, Mc-Conahey WM. Papillary thyroid carcinoma in children and adults: longterm follow-up of 1039 patients conservatively treated at one institution during three decades. Surgery. 1988. 104:1157–1166.9. Koo JS, Hong S, Park CS. Diffuse sclerosing variant is a major subtype of papillary thyroid carcinoma in the young. Thyroid. 2009. 19:1225–1231.10. Welch Dinauer CA, Tuttle RM, Robie DK, McClellan DR, Francis GL. Extensive surgery improves recurrence-free survival for children and young patients with class I papillary thyroid carcinoma. J Pediatr Surg. 1999. 34:1799–1804.11. Stael AP, Plukker JT, Piers DA, Rouwé CW, Vermey A. Total thyroidectomy in the treatment of thyroid carcinoma in childhood. Br J Surg. 1995. 82:1083–1085.12. Steinmüller T, Klupp J, Wenking S, Neuhaus P. Complications associated with different surgical approaches to differentiated thyroid carcinoma. Langenbecks Arch Surg. 1999. 384:50–53.13. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009. 19:1167–1214.14. Viswanathan K, Gierlowski TC, Schneider AB. Childhood thyroid cancer: characteristics and long-term outcome in children irradiated for benign conditions of the head and neck. Arch Pediatr Adolesc Med. 1994. 148:260–265.15. Buckwalter JA, Thomas CG, Freeman JB. Is childhood thyroid cancer a lethal disease? Ann Surg. 1975. 181:632–639.16. Xing M. BRAF mutation in thyroid cancer. Endocr Relat Cancer. 2005. 12:245–262.17. Nikiforov YE. RET/PTC rearrangement in thyroid tumors. Endocr Pathol. 2002. 13:3–16.18. Nikiforov YE, Rowland JM, Bove KE, Monforte-Munoz H, Fagin JA. Distinct pattern of ret oncogene rearrangements in morphological variants of radiation-induced and sporadic thyroid papillary carcinomas in children. Cancer Res. 1997. 57:1690–1694.19. Noguchi S, Noguchi A, Murakami N. Papillary carcinoma of the thyroid: I. developing pattern of metastasis. Cancer. 1970. 26:1053–1060.20. Attie JN, Khafif RA, Steckler RM. Elective neck dissection in papillary carcinoma of the thyroid. Am J Surg. 1971. 122:464–471.21. Handkiewicz-Junak D, Wloch J, Roskosz J, Krajewska J, Kropinska A, Pomorski L, Kukulska A, Prokurat A, Wygoda Z, Jarzab B. Total thyroidectomy and adjuvant radioiodine treatment independently decrease locoregional recurrence risk in childhood and adolescent differentiated thyroid cancer. J Nucl Med. 2007. 48:879–888.22. Bramley MD, Harrison BJ. Papillary microcarcinoma of the thyroid gland. Br J Surg. 1996. 83:1674–1683.23. Harach HR, Franssila KO, Wasenius VM. Occult papillary carcinoma of the thyroid: a "normal" finding in Finland: a systematic autopsy study. Cancer. 1985. 56:531–538.24. Pelizzo MR, Boschin IM, Toniato A, Pagetta C, Piotto A, Bernante P, Casara D, Pennelli G, Rubello D. Natural history, diagnosis, treatment and outcome of papillary thyroid microcarcinoma (PTMC): a mono-institutional 12-year experience. Nucl Med Commun. 2004. 25:547–552.25. Hallwirth U, Flores J, Kaserer K, Niederle B. Differentiated thyroid cancer in children and adolescents: the importance of adequate surgery and review of literature. Eur J Pediatr Surg. 1999. 9:359–363.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A 20 years, experience with well differentiated thyroid carcinoma in children & teenagers
- rhTSH-aided Radioiodine Treatment in Differentiated Thyroid Carcinoma
- Fine Needle Aspiration Biopsy of Thyroid Nodules in Children and Adolescents
- Preoperative Staging of Well Differentiated Thyroid Cancer: US Is Enough?
- A Case of Differentiated Thyroid Carcinoma with Internal Jugular Vein Tumor Thrombus