Korean Circ J.
2011 Dec;41(12):754-758. 10.4070/kcj.2011.41.12.754.
Very Late Stent Thrombosis due to Neointimal Rupture After Paclitaxel-Eluting Stent Implantation
- Affiliations
-
- 1The Heart Research Center Nominated by Korea Ministry of Health and Welfare, Chonnam National University Hospital, Gwangju, Korea. myungho@chollian.net
- KMID: 1776253
- DOI: http://doi.org/10.4070/kcj.2011.41.12.754
Abstract
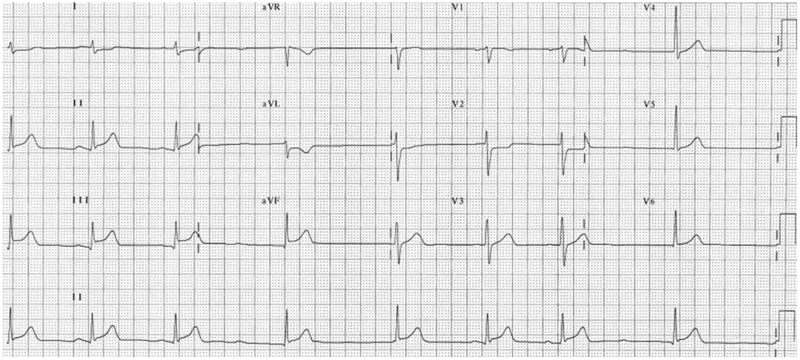
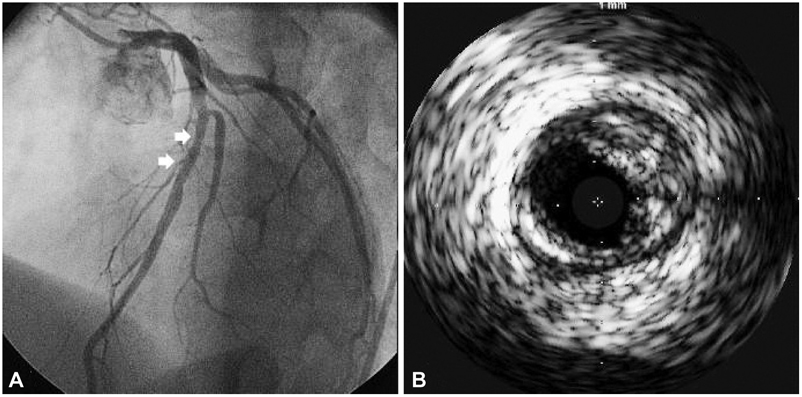
- We report our experience of very late stent thrombosis (VLST) in a young male patient who underwent implantation of two paclitaxel-eluting stents (PES) six years ago. The patient was compliant with standard dual antiplatelet therapy, but he presented with acute myocardial infarction which was associated with VLST. Intravascular ultrasound showed neointimal rupture with thrombus within the PES implanted in the right coronary artery. The lesion was successfully treated with balloon angioplasty without complications, however he was found to be hyporesponsive to clopidogrel when tested for adenosine diphosphate-induced platelet aggregation. The patient was discharged after uneventful recovery with triple anti-platelet therapy using aspirin, clopidogrel and cilostazol. To the best of our knowledge, a time interval of 2,223 days is the longest reported time interval between PES deployment and VLST occurrence. VLST may indeed occur in clinically stable patients, as multiple factors can influence the pathological mechanisms of VLST.
Keyword
MeSH Terms
Figure
Reference
-
1. Farb A, Heller PF, Shroff S, et al. Pathological analysis of local delivery of paclitaxel via a polymer-coated stent. Circulation. 2001. 104:473–479.2. Rogers C, Parikh S, Seifert P, Edelman ER. Endogenous cell seeding: remnant endothelium after stenting enhances vascular repair. Circulation. 1996. 94:2909–2914.3. Jensen LO, Maeng M, Kaltoft A, et al. Stent thrombosis, myocardial infarction, and death after drug-eluting and bare-metal stent coronary interventions. J Am Coll Cardiol. 2007. 50:463–470.4. Seol SH, Kim DI, Han YC, et al. Multiple sequential complications after sirolimus-eluting stent implantation: very late stent thrombosis, stent fracture, in-stent restenosis, and peri-stent aneurysm. Korean Circ J. 2009. 39:439–442.5. Kim SS, Jeong MH, Sim DS, et al. Very late thrombosis of a drug-eluting stent after discontinuation of dual antiplatelet therapy in a patient treated with both drug-eluting and bare-metal stents. Korean Circ J. 2009. 39:205–208.6. Ahn YS, Cho JH, Kim DH, et al. A fatal case of simultaneous, very late thrombosis involving three drug-eluting stents in three coronary arteries. Korean Circ J. 2008. 38:564–569.7. Nam CW, Kim KB, Chung IS. Very late stent thrombosis related to fracture of a sirolimus-eluting stent. Korean Circ J. 2007. 37:385–387.8. Mauri L, Hsieh WH, Massaro JM, Ho KK, D'Agostino R, Cutlip DE. Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med. 2007. 356:1020–1029.9. Ellis SG, Colombo A, Grube E, et al. Incidence, timing, and correlates of stent thrombosis with the polymeric paclitaxel drug-eluting stent: a TAXUS II, IV, V, and VI meta-analysis of 3,445 patients followed for up to 3 years. J Am Coll Cardiol. 2007. 49:1043–1051.10. Wenaweser P, Daemen J, Zwahlen M, et al. Incidence and correlates of drug-eluting stent thrombosis in routine clinical practice. 4-year results from a large 2-institutional cohort study. J Am Coll Cardiol. 2008. 52:1134–1140.11. Joner M, Finn AV, Farb A, et al. Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. J Am Coll Cardiol. 2006. 48:193–202.12. Yokoyama S, Takano M, Sakai S, et al. Difference in neointimal proliferation between ruptured and non-ruptured segments after bare metal stent implantation. Int Heart J. 2010. 51:7–12.13. Higo T, Ueda Y, Oyabu J, et al. Atherosclerotic and thrombogenic neointima formed over sirolimus drug-eluting stent: an angioscopic study. JACC Cardiovascular Imaging. 2009. 2:616–624.14. Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005. 293:2126–2130.15. Müller I, Besta F, Schulz C, Massberg S, Schönig A, Gawaz M. Prevalence of clopidogrel non-responders among patients with stable angina pectoris scheduled for elective coronary stent placement. Thromb Haemos. 2003. 89:783–787.16. Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, et al. Identification of low responders to a 300 mg clopidogrel loading dose in patients undergoing coronary stenting. Thromb Res. 2005. 115:101–108.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Late Stent Thrombosis Associated with Late Stent Malapposition after Drug-Eluting Stenting: A Case Report
- Very Late Stent Thrombosis Related to Fracture of a Sirolimus-Eluting Stent
- Late Stent Thrombosis After Drug-Eluting Stent Implantation: A Rare Case of Accelerated Neo-Atherosclerosis and Early Manifestation of Neointimal Rupture
- A Case of Stent Thrombosis Occurred at 5 Years after Sirolimus-Eluting Stent Implantation
- Stent Thrombosis in the Era of the Drug-Eluting Stent