Korean Circ J.
2011 Jun;41(6):313-320. 10.4070/kcj.2011.41.6.313.
Prevalence of Echocardiographic Features Suggesting Cardiac Sarcoidosis in Patients With Pacemaker or Implantable Cardiac Defibrillator
- Affiliations
-
- 1Division of Cardiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jksong@amc.seoul.kr
- KMID: 1776188
- DOI: http://doi.org/10.4070/kcj.2011.41.6.313
Abstract
- BACKGROUND AND OBJECTIVES
Basal septal thinning or localized aneurysmal dilatation without coronary artery disease has been described as a characteristic finding suggestive of cardiac sarcoidosis. We sought to assess the prevalence of this characteristic echocardiographic finding in patients with pacemaker (PM) or implantable cardiac defibrillator (ICD).
SUBJECTS AND METHODS
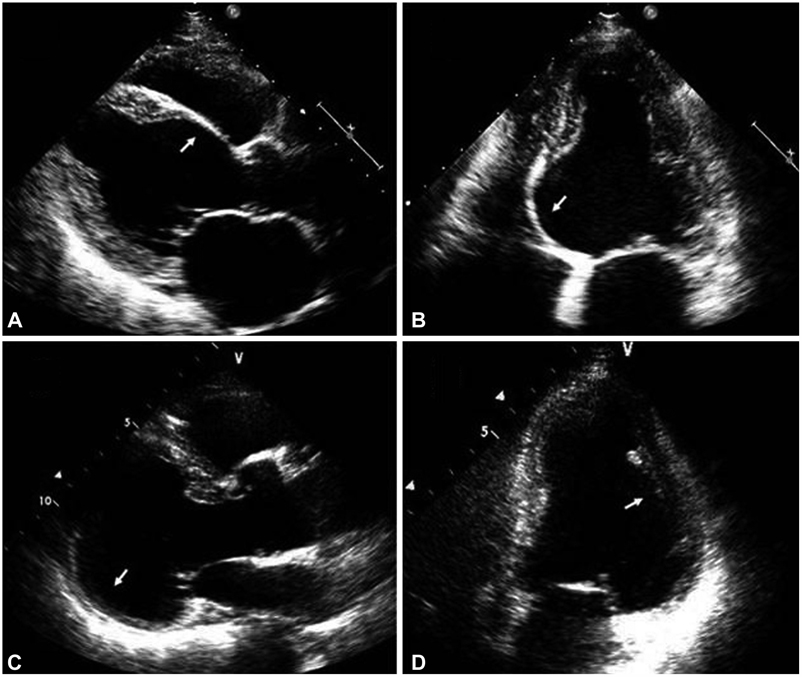
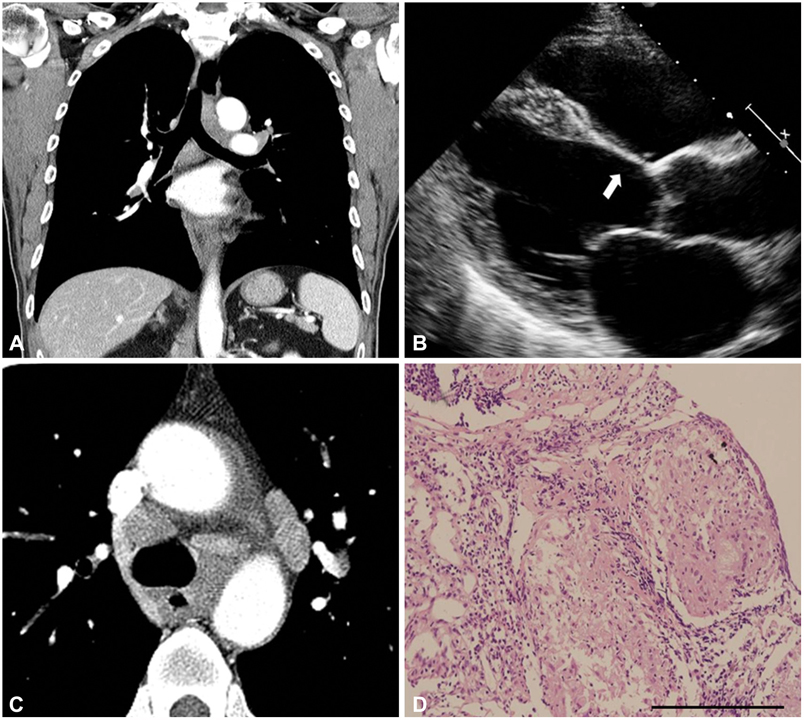
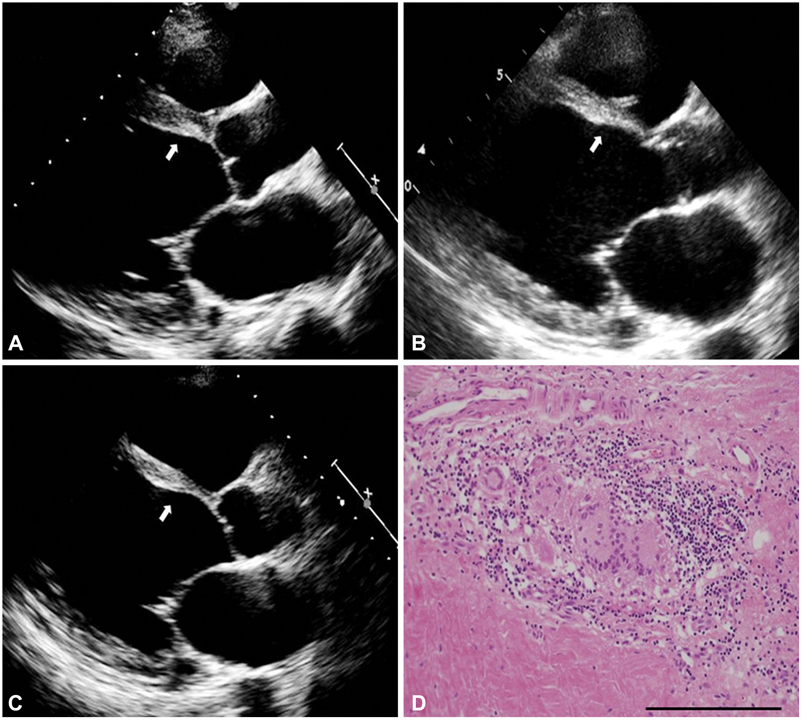
Echocardiography of patients who received PM or ICD were retrospectively analyzed. Patients with marked thinning and akinesia confined to the basal septum (type 1), or posterolateral wall resulting in localized aneurysmal outward bulging (type 2) without history of myocardial infarction or significant coronary stenosis were included for analysis.
RESULTS
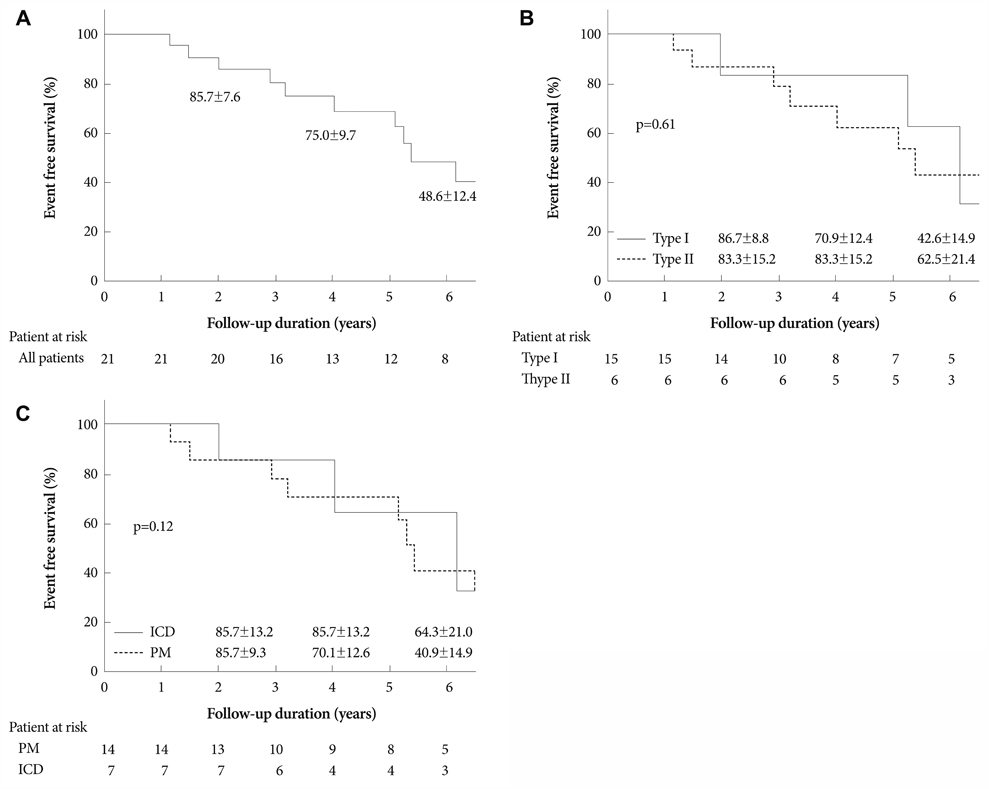
Among 1,357 consecutive patients, 21 exhibited suggestive echocardiographic findings (type 1/2=15/6) with a mean ejection fraction of 37+/-11%. The prevalence was 1.2% in the PM group and 4.0% in the ICD group. Only 3 patients showed histologically confirmable sarcoidosis in lymph nodes, lung and heart, respectively. Endomyocardial biopsy was attempted in 6 patients, but failed to demonstrate sarcoidosis. The 1-, 2-, 4- and 6-year clinical events (death, cardiac transplantation and hospital admission)-free survival rates were 100%, 85.7+/-7.6%, 75.0+/-9.7% and 48.6+/-12.4%, respectively. During follow-up, two patients with PM underwent ICD implantation, and another underwent heart transplantation.
CONCLUSION
Prevalence of echocardiographic features suggesting prevalence of cardiac sarcoidosis is low in patients who underwent device implantation. However, considering the very low yield of endomyocardial biopsy and the rare extracardiac manifestations in cardiac sarcoidosis, characteristic echocardiographic findings could be an adjunctive diagnostic criterion in these patients.
MeSH Terms
Figure
Cited by 1 articles
-
Indirect pathological indicators for cardiac sarcoidosis on endomyocardial biopsy
Myung-Jin Cha, Jeong-Wook Seo, Seil Oh, Eun-Ah Park, Sang-Han Lee, Moon Young Kim, Jae-Young Park
J Pathol Transl Med. 2020;54(5):396-410. doi: 10.4132/jptm.2020.06.10.
Reference
-
1. Dubrey SW, Bell A, Mittal TK. Sarcoid heart disease. Postgrad Med J. 2007. 83:618–623.2. Bargout R, Kelly RF. Sarcoid heart disease: clinical course and treatment. Int J Cardiol. 2004. 97:173–182.3. Sekiguchi M, Yazaki Y, Isobe M, Hiroe M. Cardiac sarcoidosis: diagnostic, prognostic, and therapeutic considerations. Cardiovasc Drugs Ther. 1996. 10:495–510.4. Lewin RF, Mor R, Spitzer S, Arditti A, Hellman C, Agmon J. Echocardiographic evaluation of patients with systemic sarcoidosis. Am Heart J. 1985. 110:116–122.5. Roberts WC, McAllister HA Jr, Ferrans VJ. Sarcoidosis of the heart. A clinicopathologic study of 35 necropsy patients (group 1) and review of 78 previously described necropsy patients (group 11). Am J Med. 1977. 63:86–108.6. Silverman KJ, Hutchins GM, Bulkley BH. Cardiac sarcoid: a clinicopathologic study of 84 unselected patients with systemic sarcoidosis. Circulation. 1978. 58:1204–1211.7. Yamano T, Nakatani S. Cardiac sarcoidosis: what can we know from echocardiography? J Echocardiogr. 2007. 5:1–10.8. Hiraga H, Yuwai K, Hiroe M. Guidelines for the diagnosis of cardiac sarcoidosis: study report of diffuse pulmonary diseases. 1993. Tokyo: Japanese Ministry of Health and Welfare;23–24.9. Tawarahara K, Kurata C, Okayama K, Kobayashi A, Yamazaki N. Thallium-201 and gallium 67 single photon emission computed tomographic imaging in cardiac sarcoidosis. Am Heart J. 1992. 124:1383–1384.10. Tellier P, Paycha F, Antony I, et al. Reversibility by dipyridamole of thallium-201 myocardial scan defects in patients with sarcoidosis. Am J Med. 1988. 85:189–193.11. Rybicki BA, Major M, Popovich J, Maliarik MJ, Iannuzzi MC. Racial differences in sarcoidosis incidence: a 5-year study in a health maintenance organization. Am J Epidemiol. 1997. 145:234–241.12. Kim DS. Sarcoidosis in Korea: report of the Second Nationwide Survey. Sarcoidosis Vasc Diffuse Lung Dis. 2001. 18:176–180.13. Matsui Y, Iwai K, Tachibana T, et al. Clinicopathological study of fatal myocardial sarcoidosis. Ann N Y Acad Sci. 1976. 278:455–469.14. Siltzbach LE, James DG, Neville E, et al. Course and prognosis of sarcoidosis around the world. Am J Med. 1974. 57:847–852.15. Choi JH, Kim J, Park TI, et al. Two cases of an implantation of a permanent pacemaker using a transaxillary incision. Korean Circ J. 2008. 38:500–504.16. Uemura A, Morimoto S, Hiramitsu S, Kato Y, Ito T, Hishida H. Histologic diagnostic rate of cardiac sarcoidosis: evaluation of endomyocardial biopsies. Am Heart J. 1999. 138:299–302.17. Judson MA, Baughman RP, Teirstein AS, Terrin ML, Yeager H Jr. Defining organ involvement in sarcoidosis: the ACCESS proposed instrument. ACCESS Research Group. A Case Control Etiologic Study of Sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 1999. 16:75–86.18. Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007. 357:2153–2165.19. Nelson JE, Kirschner PA, Teirstein AS. Sarcoidosis presenting as heart disease. Sarcoidosis Vasc Diffuse Lung Dis. 1996. 13:178–182.20. Chiu CZ, Nakatani S, Zhang G, et al. Prevention of left ventricular remodeling by long-term corticosteroid therapy in patients with cardiac sarcoidosis. Am J Cardiol. 2005. 95:143–146.21. Valantine H, McKenna WJ, Nihoyannopoulos P, et al. Sarcoidosis: a pattern of clinical and morphological presentation. Br Heart J. 1987. 57:256–263.22. Cho Y. Arrhythmogenic right ventricular cardiomyopathy/dysplasia. Korean Circ J. 2008. 38:514–523.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent Advancement in the Management of the Cardiac Arrhythmia
- Transvenous Implantation of an Implantable Cardioverter Defibrillator in a Patient Who Had Undergone Tricuspid Valve Replacement
- Management of Arrhythmias Associated with Cardiac Sarcoidosis
- Implantable cardioverter defibrillator as a treatment for massive left ventricular fibroma-induced ventricular arrhythmia in a child
- Implantable Cardioverter-Defibrillator (ICD) Therapy: Initial Clinical Experience in 6 Patients