Korean J Gastroenterol.
2012 Jan;59(1):44-47. 10.4166/kjg.2012.59.1.44.
A Case of Primary Colon Amyloidosis Presenting as Hematochezia
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea. sw-jeon@hanmail.net
- KMID: 1775832
- DOI: http://doi.org/10.4166/kjg.2012.59.1.44
Abstract
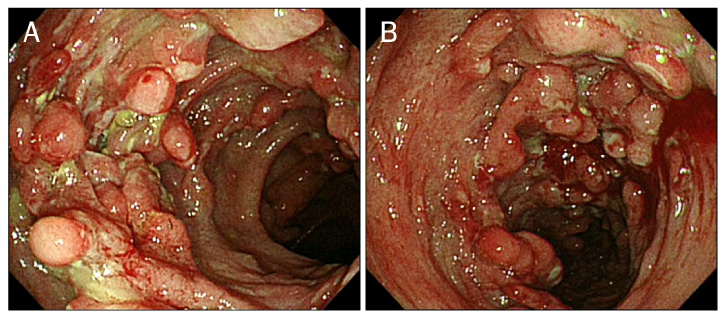
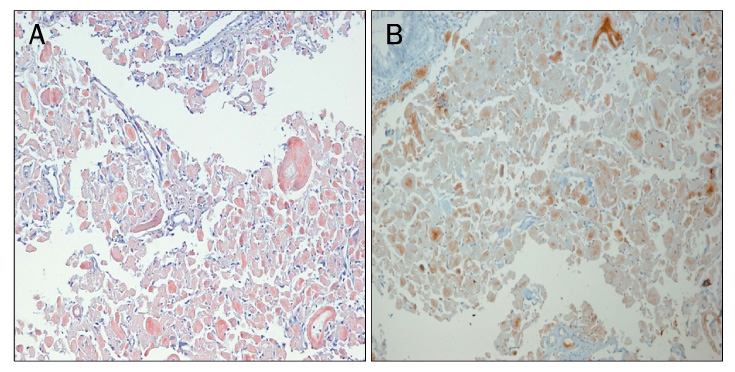
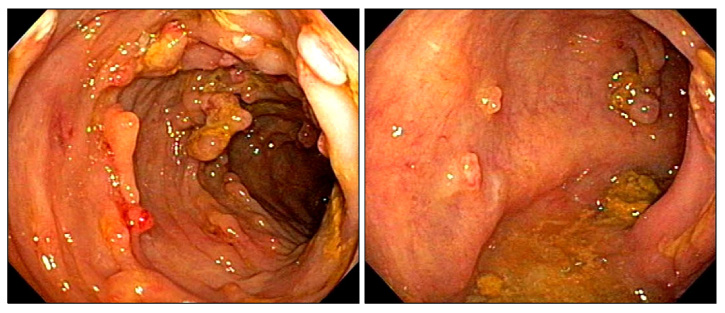
- Amyloidosis is characterized by a deposition of insoluble fibrils in various organs and tissues. Amyloid deposition, in the gastrointestinal track, provokes a dysfunction of the organ, due to an accumulation of fibrils, and causes a variety of clinical symptoms and endoscopic findings. Primary amyloidosis in the gastrointestinal tract is rarely reported in Korea. We experienced a case of recurrent intestinal bleeding, in a 59-year-old female patient with primary amyloidosis. A colonoscopy revealed the presence of multiple large circular ulcers. In the entire colon, diffuse nodular lesions with edema and bleeding were found. A colonoscopic biopsy established the diagnosis of amyloidosis, to the exclusion of other disease components. We concluded that the patient had localized amyloidosis. Though a definitive therapeutic strategy has not been established for localized gastrointestinal amyloidosis, the patient has been successfully treated with a high-dose of steroids and azathioprine.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A Case of Primary Gastric Amyloidosis with Fulminant Heart Failure
Seonghun Hong, Young-Woon Chang, Jong Kyu Byun, Min Je Kim, Jung Min Chae, Sun Hee Park, Chi Hyuk Oh, Yong-Koo Park
Korean J Gastroenterol. 2015;66(4):227-230. doi: 10.4166/kjg.2015.66.4.227.
Reference
-
1. Scott PP, Scott WW Jr, Siegelman SS. Amyloidosis: an overview. Semin Roentgenol. 1986. 21:103–112.2. Kyle RA, Bayrd ED. Amyloidosis: review of 236 cases. Medicine (Baltimore). 1975. 54:271–299.3. Glenner GG, Ein D, Terry WD. The immunoglobulin origin of amyloid. Am J Med. 1972. 52:141–147.4. Gertz MA, Lacy MQ, Dispenzieri A, Hayman SR. Amyloidosis. Best Pract Res Clin Haematol. 2005. 18:709–727.5. Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. N Engl J Med. 1997. 337:898–909.6. Gertz MA, Comenzo R, Falk RH, et al. Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18-22 April 2004. Am J Hematol. 2005. 79:319–328.7. Moon W, Lee OY, Cho YJ, et al. The endoscopic findings and clinical characteristics of gastrointestinal amyloidosis. Korean J Gastrointest Endosc. 2005. 31:216–220.8. Leem JM, Choi JH, Park NG, et al. A case of gastrointestinal amyloidosis presenting with hematochezia. Korean J Gastrointest Endosc. 2002. 25:38–42.9. Levy DJ, Franklin GO, Rosenthal WS. Gastrointestinal bleeding and amyloidosis. Am J Gastroenterol. 1982. 77:422–426.10. Barth WF, Glenner GG, Waldmann TA, Zelis RF. Primary amyloidosis. Ann Intern Med. 1968. 69:787–805.11. Chitkara NL, Chugh TD, Chhuttani PN, Chugh KS. Secondary amyloidosis. Indian J Pathol Bacteriol. 1965. 8:285–293.12. Patel SA, al-Haddadin D, Schopp J, Cantave I, Duarte B, Watkins JL. Gastrointestinal manifestations of amyloidosis: a case of diverticular perforation. Am J Gastroenterol. 1993. 88:578–582.13. Puchtler H, Sweat F, Levine M. On the binding of congo red by amyloid. J Histochem Cytochem. 1962. 10:355–364.14. Usui M, Matsuda S, Suzuki H, Hirata K, Ogura Y, Shiraishi T. Gastric amyloidosis with massive bleeding requiring emergency surgery. J Gastroenterol. 2000. 35:924–928.15. Kyle RA, Gertz MA, Greipp PR, et al. A trial of three regimens for primary amyloidosis: colchicine alone, melphalan and prednisone, and melphalan, prednisone, and colchicine. N Engl J Med. 1997. 336:1202–1207.16. Takahashi A, Matsumoto J, Nishimura S, et al. Improvement of endoscopic and histologic findings of AA-type gastrointestinal amyloidosis by treatment with dimethyl sulfoxide and prednisolone. Gastroenterol Jpn. 1985. 20:143–147.17. Cohen HJ, Lessin LS, Hallal J, Burkholder P. Resolution of primary amyloidosis during chemotherapy. Studies in a patient with nephrotic syndrome. Ann Intern Med. 1975. 82:466–473.18. Redleaf PD, Davis RB, Kucinski C, Hoilund L, Gans H. Amyloidosis with and unusual bleeding diathesis; observations on the use of epsilon amino caproic acid. Ann Intern Med. 1963. 58:347–354.19. Nakamura T, Higashi S, Tomoda K, Tsukano M, Baba S. Efficacy of etanercept in patients with AA amyloidosis secondary to rheumatoid arthritis. Clin Exp Rheumatol. 2007. 25:518–522.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Intestinal Hemorrhage in Patient with Primary Amyloidosis
- A Case of Amyloidosis with Recurrent Intestinal Bleeding
- A Case of Secondary Amyloidosis Presenting as Massive Gastrointestinal Bleeding
- Primary Systemic Amyloidosis Presenting as Swollen Dense Breast: A Case Report
- Primary localized amyloidosis of the bladder: a case report