Korean J Gastroenterol.
2012 Nov;60(5):320-324. 10.4166/kjg.2012.60.5.320.
A Case of Acute Lymphoblastic Leukemia Presenting with Protein-Losing Enteropathy
- Affiliations
-
- 1Department of Internal Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea. kwonjg@cu.ac.kr
- KMID: 1775798
- DOI: http://doi.org/10.4166/kjg.2012.60.5.320
Abstract
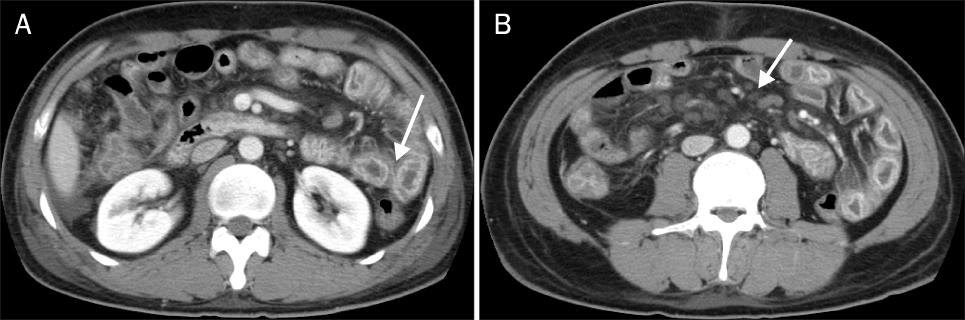
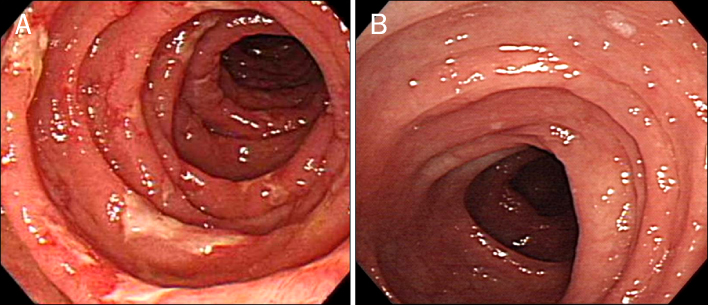
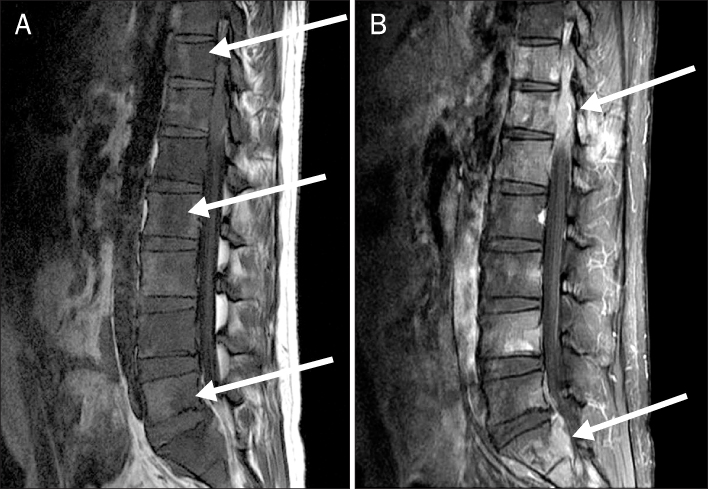
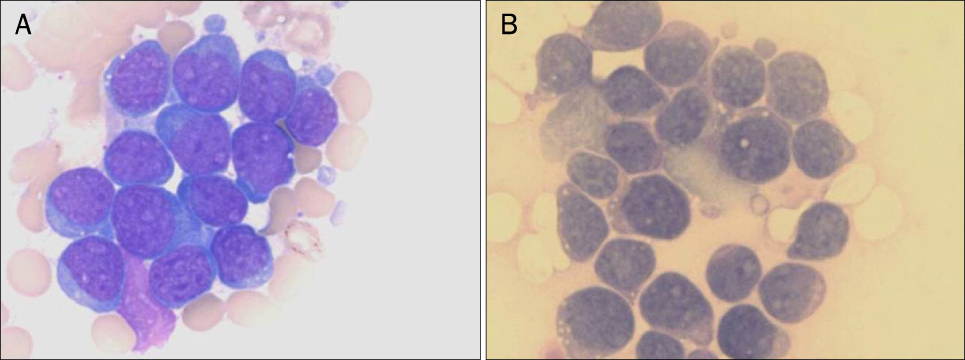
- Protein-losing enteropathy (PLE) is a syndrome characterized by excessive gastrointestinal protein loss, resulting in hypoproteinemia and edema. A variety of benign and malignant conditions can be associated with PLE and acute leukemia is a very rare cause of PLE. We report a case of PLE associated with acute lymphoblastic leukemia. A 27-year-old man was admitted due to watery diarrhea, epigastric pain and bilateral leg edema. Laboratory findings showed hypoproteinemia and polycythemia. The diagnosis of PLE and acute lymphoblastic leukemia were confirmed on the measurement of fecal alpha1-antitrypsin clearance and bone marrow examination. After systemic chemotherapy and autologous stem cell transplantation, his clinical symptoms and abnormal laboratory findings were gradually improved.
Keyword
MeSH Terms
-
Adult
Bone Marrow Cells/pathology
Endoscopy, Gastrointestinal
Humans
Magnetic Resonance Imaging
Male
Precursor Cell Lymphoblastic Leukemia-Lymphoma/complications/*diagnosis/genetics
Protein-Losing Enteropathies/complications/*diagnosis
Thoracic Vertebrae/radiography
Tomography, X-Ray Computed
Translocation, Genetic
alpha 1-Antitrypsin/analysis
alpha 1-Antitrypsin
Figure
Reference
-
1. Waldmann TA. Protein-losing enteropathy. Gastroenterology. 1966. 50:422–423.2. Umar SB, DiBaise JK. Protein-losing enteropathy: case illustrations and clinical review. Am J Gastroenterol. 2010. 105:43–49.3. Hunter TB, Bjelland JC. Gastrointestinal complications of leukemia and its treatment. AJR Am J Roentgenol. 1984. 142:513–518.4. Schmidt PN, Blirup-Jensen S, Svendsen PJ, Wandall JH. Characterization and quantification of plasma proteins excreted in faeces from healthy humans. Scand J Clin Lab Invest. 1995. 55:35–45.5. Takeda H, Ishihama K, Fukui T, et al. Significance of rapid turnover proteins in protein-losing gastroenteropathy. Hepatogastroenterology. 2003. 50:1963–1965.6. Goldberg RI, Calleja GA. Haubrich WS, Schaffner F, Berk JE. Protein-losing gastroenteropathy. Bockus Gastroenterology. 1995. 5th ed. Philadelphia: W.B. Saunders Co.;1072–1086.7. Kaneko H, Yamashita M, Ohshiro M, et al. Protein-losing enteropathy in a case of nodal follicular lymphoma without a gastrointestinal mucosal lesion. Intern Med. 2008. 47:2171–2173.8. Nishiuchi M, Iida M, Saika Y, et al. Malignant lymphoma originating in the jejunum of a long-term follow-up case of protein-losing enteropathy. Intern Med. 1997. 36:556–560.9. Chieng JH, Garrett J, Ding SL, Sullivan M. Clinical presentation and endoscopic features of primary gastric Burkitt lymphoma in childhood, presenting as a protein-losing enteropathy: a case report. J Med Case Rep. 2009. 3:7256.10. Waldmann TA, Wochner RD, Strober W. The role of the gastrointestinal tract in plasma protein metabolism. Studies with 51Cr-albumin. Am J Med. 1969. 46:275–285.11. Chau TN, Mok MY, Chan EY, et al. Evaluation of performance of measurement of faecal α(1)-antitrypsin clearance and technetium-99m human serum albumin scintigraphy in protein-losing enteropathy. Digestion. 2011. 84:199–206.12. Bernier JJ, Florent C, Desmazures C, Aymes C, L'Hirondel C. Diagnosis of protein-losing enteropathy by gastrointestinal clearance of alpha1-antitrypsin. Lancet. 1978. 2:763–764.13. Ferrante M, Penninckx F, De Hertogh G, et al. Protein-losing enteropathy in Crohn's disease. Acta Gastroenterol Belg. 2006. 69:384–389.14. Strygler B, Nicar MJ, Santangelo WC, Porter JL, Fordtran JS. Alpha 1-antitrypsin excretion in stool in normal subjects and in patients with gastrointestinal disorders. Gastroenterology. 1990. 99:1380–1387.15. Uzuner O, Ziessman HA. Protein-losing enteropathy detected by Tc-99m-MDP abdominal scintigraphy. Pediatr Radiol. 2008. 38:1122–1124.16. Hallevy C, Sperber AD, Almog Y. Group G streptococcal empyema complicating primary intestinal lymphangiectasia. J Clin Gastroenterol. 2003. 37:270.17. Ducassou S, Ferlay C, Bergeron C, et al. Clinical presentation, evolution, and prognosis of precursor B-cell lymphoblastic lymphoma in trials LMT96, EORTC 58881, and EORTC 58951. Br J Haematol. 2011. 152:441–451.18. Landzberg BR, Pochapin MB. Protein-losing enteropathy and gastropathy. Curr Treat Options Gastroenterol. 2001. 4:39–49.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of systemic lupus erythematosus with chylothorax, chronic interstitial cystitis and protein-losing enteropathy
- A Case of Eosinophilic Gastroenteritis Associsted with Protein - losing Enteropathy
- A case of constrictive pericarditis presenting with protein-losing enteropathy
- A Case of Primary Sjogren's Syndrome with Protein-losing Enteropathy
- Primary protein-losing enteropathy : report of a case (idiopathic intestinal lymphangiectasia)