Korean J Gastroenterol.
2013 Feb;61(2):93-96. 10.4166/kjg.2013.61.2.93.
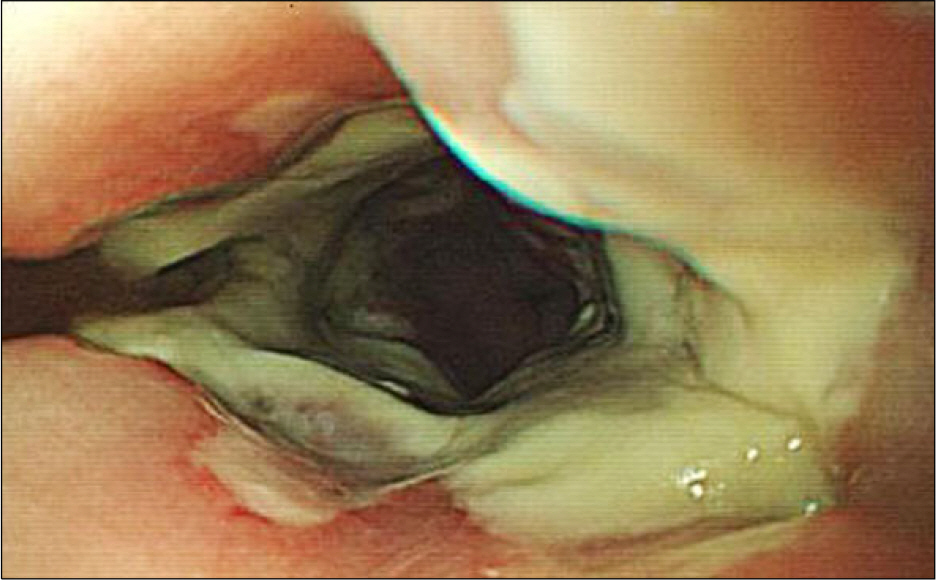
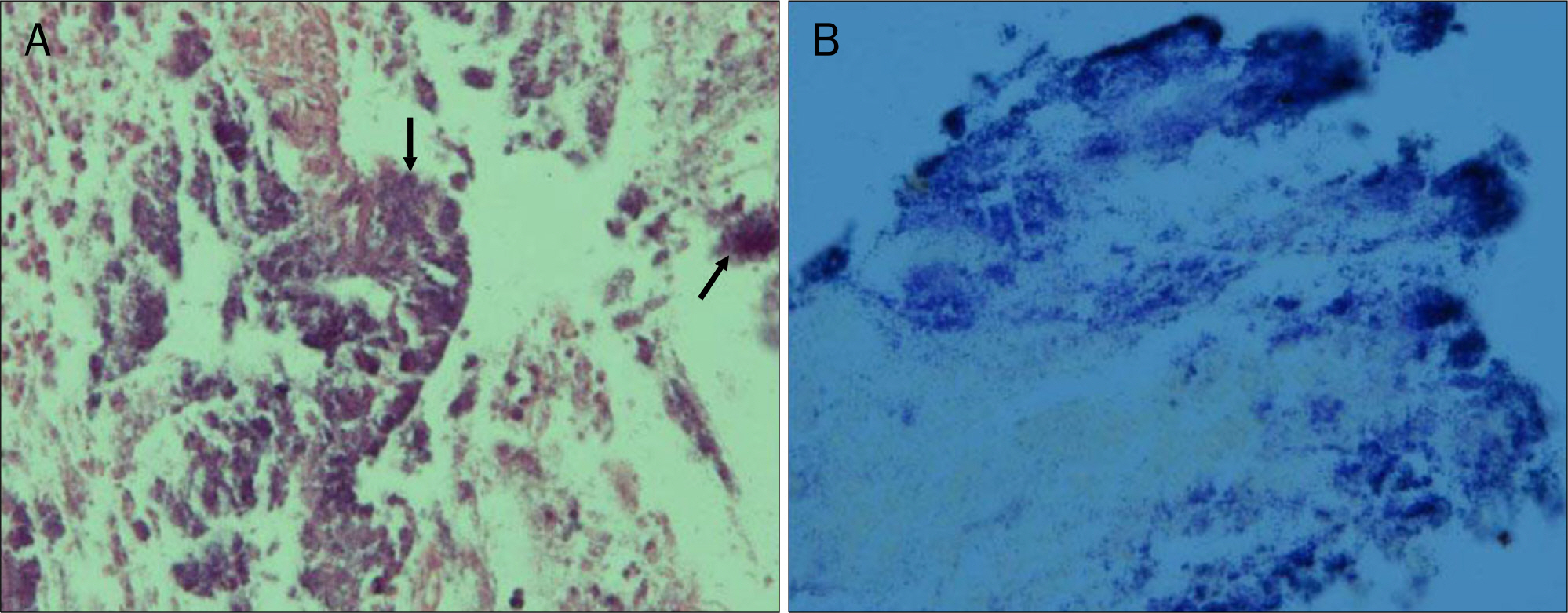
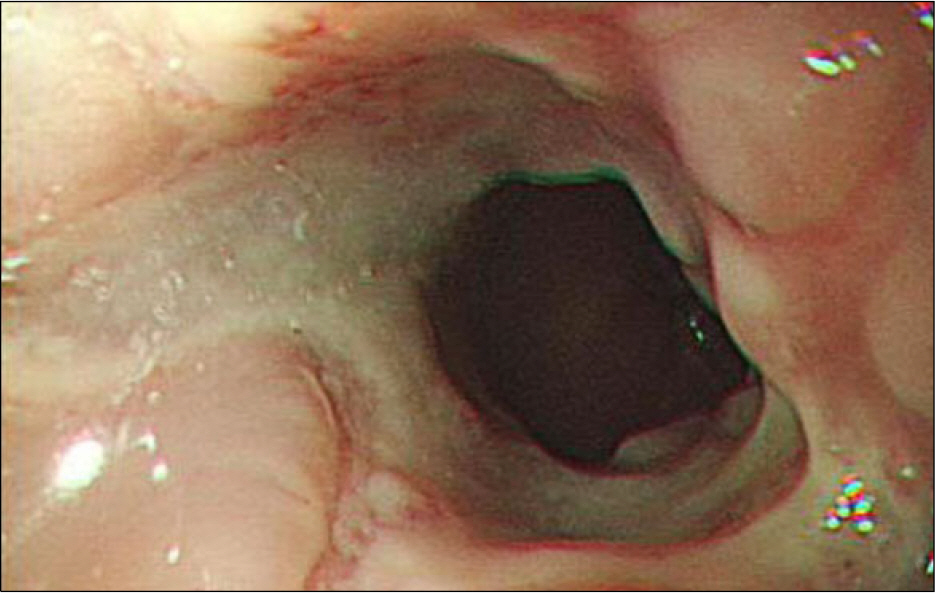
A Case of Esophageal Actinomycosis in a Patient with Normal Immunity
- Affiliations
-
- 1Department of Internal Medicine, DongKang Medical Center, Ulsan, Korea. oon76@naver.com
- 2Department of Pathology, DongKang Medical Center, Ulsan, Korea.
- KMID: 1775773
- DOI: http://doi.org/10.4166/kjg.2013.61.2.93
Abstract
- Actinomycosis is a chronic suppurative disease and caused by Actinomycosis species, principally Actinomyces israelii, which are part of the normal inhabitant on the mucous membrane of the oropharynx, gastrointestinal tract, and urogenital tract. It usually affects cervicofacial, thoracic and abdominal tissue. Cervicofacial type has the highest percentage of occurrence with 50%. Actinomycosis frequently occurs following dental extraction, jaw surgery, chronic infection or poor oral hygiene. It may also be considered as an opportunistic infection in immunocompromised patients such as malignancy, human immunodeficiency virus infection, diabetes mellitus, steroid usage or alcoholism. But, actinomycosis rarely occurs in adults with normal immunity and rare in the esophagus. We report an unusual case of esophageal actinomycosis which was developed in a patient with normal immunity and improved by therapy with intravenous penicillin G followed oral amoxicillin, and we also reviewed the associated literature.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Smego RA Jr, Foglia G. Actinomycosis. Clin Infect Dis. 1998; 26:1255–1261.
Article2. Garner JP, Macdonald M, Kumar PK. Abdominal actinomycosis. Int J Surg. 2007; 5:441–448.
Article3. Wong VK, Turmezei TD, Weston VC. Actinomycosis. BMJ. 2011; 343:d6099.
Article4. Yagi T, Fujino H, Hirai M, et al. Esophageal actinomycosis after allogeneic peripheral blood stem cell transplantation for extranodal natural killer/T cell lymphoma, nasal type. Bone Marrow Transplant. 2003; 32:451–453.
Article5. Jee SB, Jang KS, Kim SH, Kim CJ. Actinomycosis of the appendix: a case report. J Korean Soc Coloproctol. 2010; 26:233–237.
Article6. Weese WC, Smith IM. A study of 57 cases of actinomycosis over a 36-year period. A diagnostic ‘failure’ with good prognosis after treatment. Arch Intern Med. 1975; 135:1562–1568.
Article7. Murchan EM, Redelman-Sidi G, Patel M, Dimaio C, Seo SK. Esophageal actinomycosis in a fifty-three-year-old man with HIV: case report and review of the literature. AIDS Patient Care STDS. 2010; 24:73–78.
Article8. Brenner RW, Gehring SW 2nd. Pelvic actinomycosis in the presence of an endocervical contraceptive device. Report of a case. Obstet Gynecol. 1967; 29:71–73.9. Chou FT, Cheng KS, Chiang IP. Esophageal actinomycosis. Adv Ther. 2006; 23:623–626.
Article10. Kosseifi SG, Dittus K, Nassour DN, Shaikh MA, Young MF. Actinomycosis esophagitis in a patient with persistent dysphagia. South Med J. 2005; 98:662–664.
Article11. Arora AK, Nord J, Olofinlade O, Javors B. Esophageal actinomycosis: a case report and review of the literature. Dysphagia. 2003; 18:27–31.
Article12. Cash JW, McConville C, O'Rourke D, Harding T. Oesophageal ulceration: more than meets the naked eye? Gut. 2005; 54:127–133.
Article13. Fernández Moreno N, Ubiña Aznar E, Rivera Irigoín R, et al. Esophagus actinomycosis causing upper gastrointestinal bleeding. Rev Esp Enferm Dig. 2005; 97:533–534.14. Rachman I. Mpilo hospital round. Actinomycosis of the oesophagus. Cent Afr J Med. 1970; 16:216–218.15. Sudhakar SS, Ross JJ. Short-term treatment of actinomycosis: two cases and a review. Clin Infect Dis. 2004; 38:444–447.
Article16. Kahn JE, Boccara O, Girszyn N, Bernier M, Blétry O, Fain O. A terri-ble diagnosis and hard to swallow!…. Rev Med Interne. 2005; 26(Suppl 2):S230–S233.17. Cintron JR, Del Pino A, Duarte B, Wood D. Abdominal actinomycosis. Dis Colon Rectum. 1996; 39:105–108.
Article18. Simsek A, Perek A, Cakcak IE, Durgun AV. Pelvic actinomycosis presenting as a malignant pelvic mass: a case report. J Med Case Rep. 2011; 5:40.
Article19. Smith AJ, Hall V, Thakker B, Gemmell CG. Antimicrobial susceptibility testing of Actinomyces species with 12 antimicrobial agents. J Antimicrob Chemother. 2005; 56:407–409.
Article20. Macfarlane DJ, Tucker LG, Kemp RJ. Treatment of recalcitrant actinomycosis with ciprofloxacin. J Infect. 1993; 27:177–180.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Esophageal Actinomycosis after Insertion of Esophageal Stent: A Case of Surgical Experience
- A Case of Esophageal Actinomycosis without Treatment in an Immunocompetent Patient
- Case of Esophageal Actinomycosis Occurred after Endoscopic Mucosal Resection for Subepithelial Tumor
- A Case of Actinomycosis of the Maxillary Sinus Accompanied with Fungal Ball
- Hepatic Actinomycosis Mimicking a Malignant Tumor: Three Case Reports