Korean J Gastroenterol.
2013 Apr;61(4):219-224. 10.4166/kjg.2013.61.4.219.
Septic Pylephlebitis as a Rare Complication of Crohn's Disease
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Kyung Hee University School of Medicine, Seoul, Korea. cklee92@paran.com
- KMID: 1775762
- DOI: http://doi.org/10.4166/kjg.2013.61.4.219
Abstract
- Thrombophlebitis of the portal venous system (PVS) with superimposed bacterial infection (septic pylephlebitis) is an extremely rare complication of Crohn's disease (CD), and therefore diagnosis of septic pylephlebitis is difficult without high clinical suspicion. A 16-year old male patient who was diagnosed with CD 3 months earlier was admitted with recurrent fever and abdominal pain. CD activity had been well controlled with conventional medical treatment during a follow-up period. Abdominal contrast-enhanced computed tomography showed massive thrombosis in the PVS without evidence of intra-abdominal infection, and blood cultures were positive for Streptococcus viridians. There was no evidence of deep vein thrombosis or pulmonary thromboembolism, and all laboratory tests for thrombophilia were normal. Based on these findings, the patient was diagnosed with septic pylephlebitis complicated with CD, and was successfully treated with intravenous antibiotic therapy combined with anticoagulation. This case suggests that early comprehensive evaluation is crucial for immediate diagnosis and proper treatment of septic pylephlebitis in patients with CD who present with fever and abdominal pain of unknown origin, even with stable disease activity and absence of other intra-abdominal infections.
MeSH Terms
-
Adolescent
Anti-Bacterial Agents/therapeutic use
Anticoagulants/therapeutic use
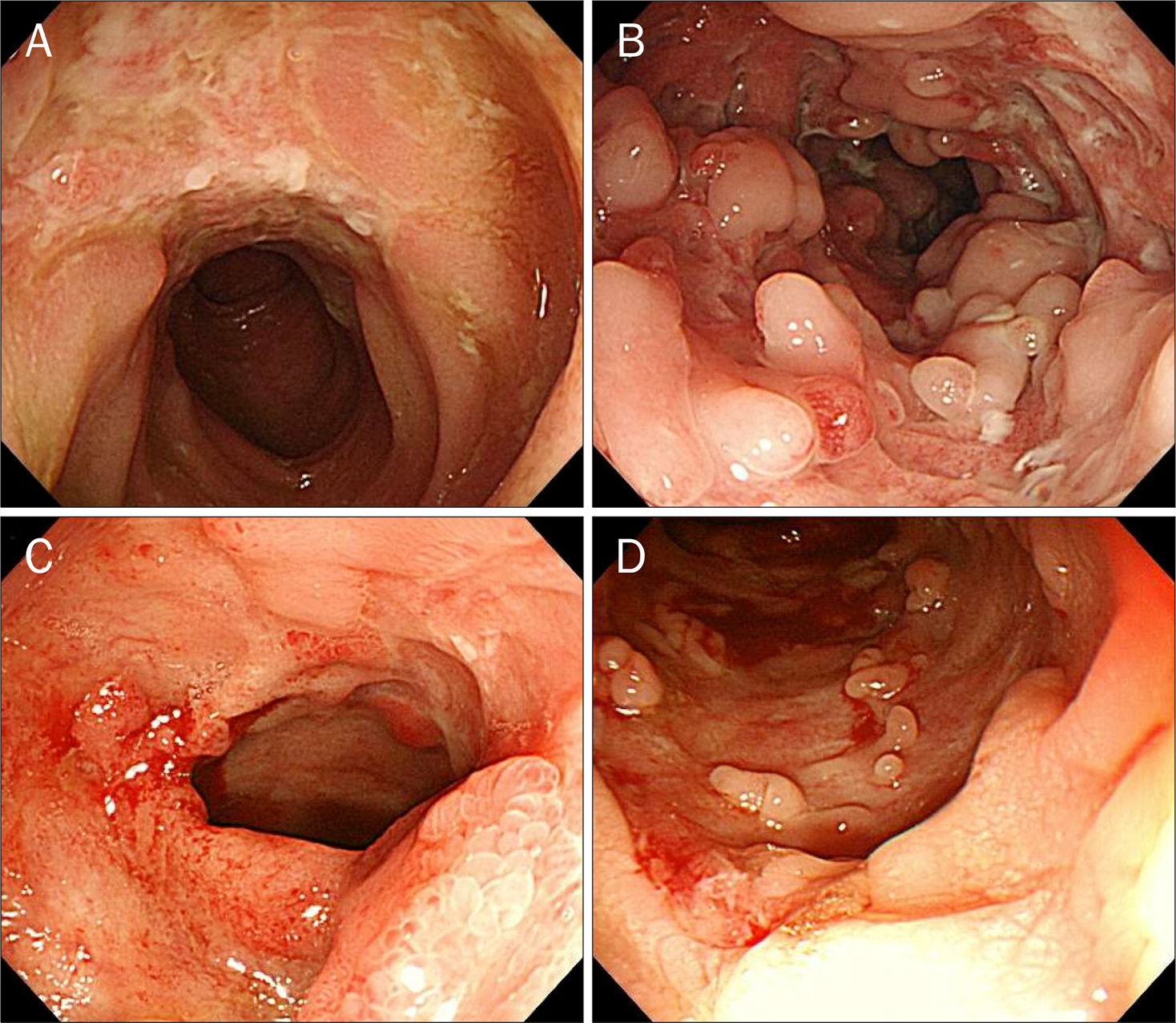
Colonoscopy
Crohn Disease/complications/*diagnosis
Humans
Male
Phlebitis/complications/*diagnosis
Portal Vein/radiography
Sepsis/*diagnosis/microbiology
Streptococcal Infections/diagnosis/drug therapy
Thrombosis/drug therapy/radiography
Tomography, X-Ray Computed
Viridans Streptococci/isolation & purification
Anti-Bacterial Agents
Anticoagulants
Figure
Cited by 1 articles
-
A Case of Pylephlebitis with Pseudomonas aeruginosa Sepsis and Liver Abscess Secondary to Diverticulitis
Yoon Gwon Mun, Seong Wan Son, Minah Kim, Insoo Kim, Yong Hee Kim, Il Soon Jung, Byeong Seong Ko
Korean J Gastroenterol. 2016;67(6):327-331. doi: 10.4166/kjg.2016.67.6.327.
Reference
-
References
1. Miehsler W, Reinisch W, Valic E, et al. Is inflammatory bowel disease an independent and disease specific risk factor for throm-boembolism? Gut. 2004; 53:542–548.
Article2. Aguas M, Bastida G, Nos P, Beltrán B, Grueso JL, Grueso J. Septic thrombophlebitis of the superior mesenteric vein and multiple liver abscesses in a patient with Crohn's disease at onset. BMC Gastroenterol. 2007; 7:22.
Article3. Sherigar R, Amir KA, Bobba RK, Arsura EL, Srinivas N. Abdominal pain secondary to pylephlebitis: an uncommon disease of the portal venous system, treated with local thrombolytic therapy. Dig Dis Sci. 2005; 50:983–987.
Article4. Taylor FW. Regional enteritis complicated by pylephlebitis and multiple liver abscesses. Am J Med. 1949; 7:838–840.
Article5. Saxena R, Adolph M, Ziegler JR, Murphy W, Rutecki GW. Pylephlebitis: a case report and review of outcome in the antibiotic era. Am J Gastroenterol. 1996; 91:1251–1253.6. El-Matary W, Jaffray B, Scott J, Hodges S. Portal pyaemia as a presenting feature of paediatric crohn disease. J Pediatr Gastroenterol Nutr. 2006; 43:260–262.
Article7. Ng SS, Yiu RY, Lee JF, Li JC, Leung KL. Portal venous gas and thrombosis in a Chinese patient with fulminant Crohn's colitis: a case report with literature review. World J Gastroenterol. 2006; 12:5582–5586.
Article8. Baddley JW, Singh D, Correa P, Persich NJ. Crohn's disease presenting as septic thrombophlebitis of the portal vein (pylephlebitis): case report and review of the literature. Am J Gastroenterol. 1999; 94:847–849.
Article9. Tung JY, Johnson JL, Liacouras CA. Portal-mesenteric pylephlebitis with hepatic abscesses in a patient with Crohn's disease treated successfully with anticoagulation and antibiotics. J Pediatr Gastroenterol Nutr. 1996; 23:474–478.
Article10. Ajzen SA, Gibney RG, Cooperberg PL, Scudamore CH, Miller RR. Enterovenous fistula: unusual complication of Crohn disease. Radiology. 1988; 166:745–746.
Article11. Drabick JJ, Landry FJ. Suppurative pylephlebitis. South Med J. 1991; 84:1396–1398.
Article12. Sanghavi P, Paramesh A, Dwivedi A, Markova T, Phan T. Mesenteric arterial thrombosis as a complication of Crohn's disease. Dig Dis Sci. 2001; 46:2344–2346.13. Freeman HJ. Venous thromboembolism with inflammatory bowel disease. World J Gastroenterol. 2008; 14:991–993.14. Murthy SK, Nguyen GC. Venous thromboembolism in inflammatory bowel disease: an epidemiological review. Am J Gastroenterol. 2011; 106:713–718.
Article15. Grainge MJ, West J, Card TR. Venous thromboembolism during active disease and remission in inflammatory bowel disease: a cohort study. Lancet. 2010; 375:657–663.
Article16. Di Fabio F, Obrand D, Satin R, Gordon PH. Intra-abdominal venous and arterial thromboembolism in inflammatory bowel disease. Dis Colon Rectum. 2009; 52:336–342.
Article17. Carter MJ, Lobo AJ, Travis SP. IBD Section, British Society of Gastroenterology. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004; 53(Suppl 5):V1–V16.
Article18. Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest. 2008; 133(6 Suppl):381S–453S.19. Novacek G, Weltermann A, Sobala A, et al. Inflammatory bowel disease is a risk factor for recurrent venous thromboembolism. Gastroenterology. 2010; 139:779–787.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pylephlebitis as a Complication of Acute Appendicitis
- A case of pylephlebitis with Streptococcus viridans and Bacteroides fragilis bacteremia secondary to diverticulitis
- Pylephlebitis and Multiple Liver Abscesses Caused by Band Erosion Following Laparoscopic Adjustable Gastric Banding
- A Case of Pylephlebitis of the Inferior Mesenteric Vein and Portal Vein
- Pylephlebitis: Report of a Case Secondary to Appendicitis and Review of Cases Reported in Korea