J Korean Med Sci.
2014 Apr;29(4):536-543. 10.3346/jkms.2014.29.4.536.
The Association of Socioeconomic Status with Three-Year Clinical Outcomes in Patients with Acute Myocardial Infarction Who Underwent Percutaneous Coronary Intervention
- Affiliations
-
- 1The Heart Center of Chonnam National University Hospital, Gwangju, Korea. myungho@chollian.net
- 2Department of Public Health, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 1774459
- DOI: http://doi.org/10.3346/jkms.2014.29.4.536
Abstract
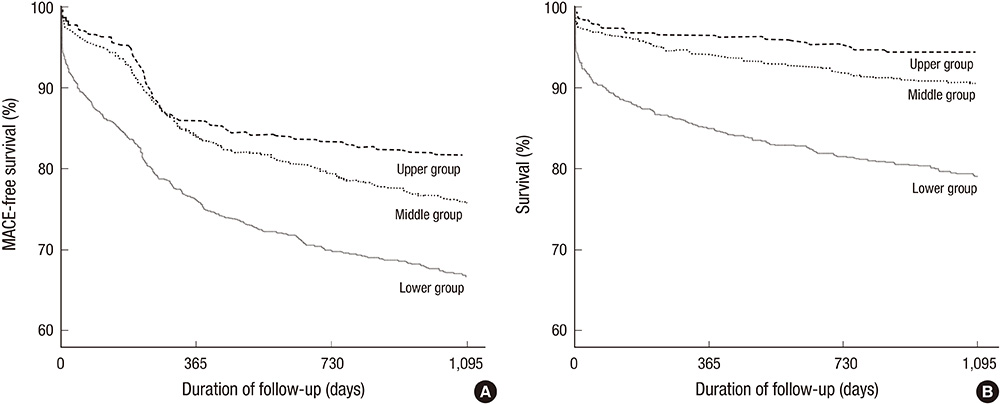
- The aim of this study was to evaluate whether the clinical outcomes were associated with socioeconomic status (SES) in patients with acute myocardial infarction (AMI) who underwent percutaneous coronary intervention (PCI). The author analyzed 2,358 patients (64.9 +/- 12.3 yr old, 71.5% male) hospitalized with AMI between November 2005 and June 2010. SES was measured by the self-reported education (years of schooling), the residential address (social deprivation index), and the national health insurance status (medical aid beneficiaries). Sequential multivariable modeling assessed the relationship of SES factors with 3-yr major adverse cardiovascular events (MACEs) and mortality after the adjustment for demographic and clinical factors. During the 3-yr follow-up, 630 (26.7%) MACEs and 322 (13.7%) all-cause deaths occurred in 2,358 patients. In multivariate Cox proportional hazards regression modeling, the only lower education of SES variables was associated with MACEs (hazard ratio [HR], 1.41; 95% confidence interval [CI], 1.04-1.91) and mortality (HR, 1.93; 95% CI, 1.16-3.20) in the patients with AMI who underwent PCI. The study results indicate that the lower education is a significant associated factor to increased poor clinical outcomes in patients with AMI who underwent PCI.
Keyword
MeSH Terms
-
Acute Disease
Age Factors
Aged
*Angioplasty, Balloon, Coronary
Cohort Studies
Demography
Female
Follow-Up Studies
Humans
Male
Middle Aged
Myocardial Infarction/economics/mortality/*therapy
*Percutaneous Coronary Intervention
Proportional Hazards Models
Retrospective Studies
Risk Factors
Sex Factors
Social Class
Socioeconomic Factors
Treatment Outcome
Figure
Reference
-
1. World Health Organization. The top 10 causes of death. accessed on 3 August 2013. Available at http://www.who.int/mediacentre/factsheets/fs310/en/index.html.2. Gaziano TA, Bitton A, Anand S, Abrahams-Gessel S, Murphy A. Growing epidemic of coronary heart disease in low- and middle-income countries. Curr Probl Cardiol. 2010; 35:72–115.3. Rosengren A, Subramanian SV, Islam S, Chow CK, Avezum A, Kazmi K, Sliwa K, Zubaid M, Rangarajan S, Yusuf S. Education and risk for acute myocardial infarction in 52 high, middle and low-income countries: INTERHEART case-control study. Heart. 2009; 95:2014–2022.4. González-Zobl G, Grau M, Muñoz MA, Martí R, Sanz H, Sala J, Masiá R, Rohlfs I, Ramos R, Marrugat J, et al. Socioeconomic status and risk of acute myocardial infarction: population-based case-control study. Rev Esp Cardiol. 2010; 63:1045–1053.5. Manderbacka K, Elovainio M. The complexity of the association between socioeconomic status and acute myocardial infarction. Rev Esp Cardiol. 2010; 63:1015–1018.6. Salomaa V, Niemelä M, Miettinen H, Ketonen M, Immonen-Räihä P, Koskinen S, Mähönen M, Lehto S, Vuorenmaa T, Palomäki P, et al. Relationship of socioeconomic status to the incidence and prehospital, 28-day, and 1-yr mortality rates of acute coronary events in the FINMONICA myocardial infarction register study. Circulation. 2000; 101:1913–1918.7. Koh DH, Kim HR, Han SS, Jee SH. The relationship between socioeconomic position and the predicted risk of ischemic heart disease with using health risk appraisal. J Prev Med Public Health. 2006; 39:359–364.8. Sundquist J, Malmström M, Johansson SE. Cardiovascular risk factors and the neighbourhood environment: a multilevel analysis. Int J Epidemiol. 1999; 28:841–845.9. Stjärne MK, Fritzell J, De Leon AP, Hallqvist J. Sheep Study Group. Neighborhood socioeconomic context, individual income and myocardial infarction. Epidemiology. 2006; 17:14–23.10. Lawlor DA, Davey Smith G, Patel R, Ebrahim S. Life-course socioeconomic position, area deprivation, and coronary heart disease: findings from the British Women's Heart and Health Study. Am J Public Health. 2005; 95:91–97.11. Kölegård Stjärne M, Diderichsen F, Reuterwall C, Hallqvist J. Sheep Study Group. Socioeconomic context in area of living and risk of myocardial infarction: results from Stockholm Heart Epidemiology Program (SHEEP). J Epidemiol Community Health. 2002; 56:29–35.12. Gerward S, Tydén P, Hansen O, Engström G, Janzon L, Hedblad B. Survival rate 28 days after hospital admission with first myocardial infarction: inverse relationship with socio-economic circumstances. J Intern Med. 2006; 259:164–172.13. Chang WC, Kaul P, Westerhout CM, Graham MM, Armstrong PW. Effects of socioeconomic status on mortality after acute myocardial infarction. Am J Med. 2007; 120:33–39.14. Gerber Y, Goldbourt U, Drory Y. Israel Study Group on First Acute Myocardial Infarction. Interaction between income and education in predicting long-term survival after acute myocardial infarction. Eur J Cardiovasc Prev Rehabil. 2008; 15:526–532.15. Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, Posner S. Socioeconomic status in health research: one size does not fit all. JAMA. 2005; 294:2879–2888.16. Lahelma E, Martikainen P, Laaksonen M, Aittomäki A. Pathways between socioeconomic determinants of health. J Epidemiol Community Health. 2004; 58:327–332.17. French JK, White HD. Clinical implications of the new definition of myocardial infarction. Heart. 2004; 90:99–106.18. Korea Health Promotion Foundation. Health promotion strategies and programmes development for health inequalities alleviation. Management Center for Health Promotion. Management Center for Health Promotion;2009. (Policy research 08-55).19. Korea Centers for Disease Control and Prevention (KCDC). Korea National Health and Nutrition Examination Survey. accessed on 20 December 2006. Available at http://knhanes.cdc.go.kr.20. Kini AS. Coronary angiography, lesion classification and severity assessment. Cardiol Clin. 2006; 24:153–162.21. Manginas A, Gatzov P, Chasikidis C, Voudris V, Pavlides G, Cokkinos DV. Estimation of coronary flow reserve using the Thrombolysis in Myocardial Infarction (TIMI) frame count method. Am J Cardiol. 1999; 83:1562–1565.22. Socio-economic status and risk factors for cardiovascular disease: a multicentre collaborative study in the International Clinical Epidemiology Network (INCLEN): the INCLEN Multicentre Collaborative Group. J Clin Epidemiol. 1994; 47:1401–1409.23. Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 1). J Epidemiol Community Health. 2006; 60:7–12.24. Gerber Y, Benyamini Y, Goldbourt U, Drory Y. Israel Study Group on First Acute Myocardial Infarction. Neighborhood socioeconomic context and long-term survival after myocardial infarction. Circulation. 2010; 121:375–383.25. Diez Roux AV, Kershaw K, Lisabeth L. Neighborhoods and cardiovascular risk: beyond individual-level risk factors. Curr Cardiovasc Risk Rep. 2008; 2:175–180.26. Rao SV, Kaul P, Newby LK, Lincoff AM, Hochman J, Harrington RA, Mark DB, Peterson ED. Poverty, process of care, and outcome in acute coronary syndromes. J Am Coll Cardiol. 2003; 41:1948–1954.27. Davey Smith G, Hart C, Hole D, MacKinnon P, Gillis C, Watt G, Blane D, Hawthorne V. Education and occupational social class: which is the more important indicator of mortality risk? J Epidemiol Community Health. 1998; 52:153–160.28. Liberatos P, Link BG, Kelsey JL. The measurement of social class in epidemiology. Epidemiol Rev. 1988; 10:87–121.29. Steyn K, Sliwa K, Hawken S, Commerford P, Onen C, Damasceno A, Ounpuu S, Yusuf S. INTERHEART Investigators in Africa. Risk factors associated with myocardial infarction in Africa: the INTERHEART Africa study. Circulation. 2005; 112:3554–3561.30. Hwang SY, Jeong MH. Cognitive factors that influence delayed decision to seek treatment among older patients with acute myocardial infarction in Korea. Eur J Cardiovasc Nurs. 2012; 11:154–159.31. Hwang SY, Ahn YG, Jeong MH. Atypical symptom cluster predicts a higher mortality in patients with first-time acute myocardial infarction. Korean Circ J. 2012; 42:16–22.32. Hwang SY, Park EH, Shin ES, Jeong MH. Comparison of factors associated with atypical symptoms in younger and older patients with acute coronary syndromes. J Korean Med Sci. 2009; 24:789–794.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- No-Reflow Phoenomenon by Intracoronary Thrombus in Acute Myocardial Infarction
- The Prognostic Impact of Hypertriglyceridemia and Abdominal Obesity in Acute Myocardial Infarction Patients Underwent Percutaneous Coronary Intervention
- Cardiac arrest due to an unexpected acute myocardial infarction during head and neck surgery: A case report
- Clinical outcome in elderly patients older than 70 years with acute myocardial infarction after use of platelet glycoprotein IIb/IIIa receptor blocker during percutaneous coronary intervention: Comparison with those younger than 70 years
- Current status of acute myocardial infarction in Korea