J Lipid Atheroscler.
2014 Dec;3(2):105-109. 10.12997/jla.2014.3.2.105.
Large Coronary Artery Aneurysm with Thrombotic Coronary Occlusion Resulting in ST-Elevation Myocardial Infarction after Warfarin Interruption
- Affiliations
-
- 1Department of Internal Medicine, Myongji Hospital, Goyang, Korea.
- 2Division of Cardiology, Cardiovascular Center, Myongji Hospital, Goyang, Korea. chodk1234@daum.net
- KMID: 1773889
- DOI: http://doi.org/10.12997/jla.2014.3.2.105
Abstract
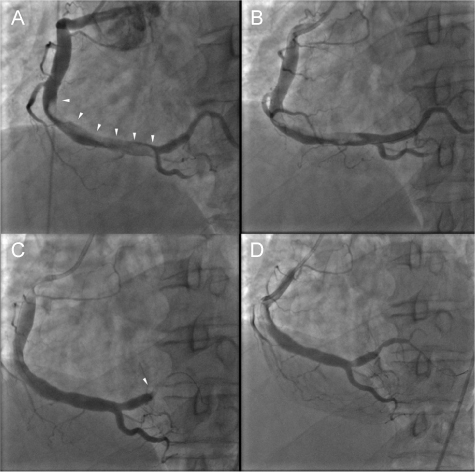
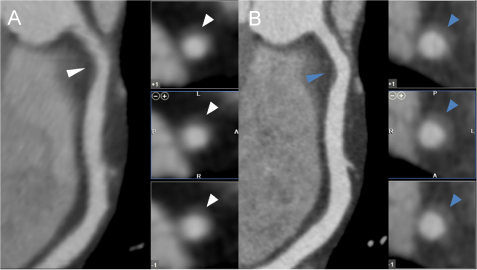
- A 44-year-old man, who had a history of myocardial infarction (MI) due to thrombotic occlusion of right coronary artery (RCA) aneurysm, visited emergency department presenting with ST-segment elevation myocardial infarction (STEMI). The patient had been on oral anticoagulant therapy (warfarin) from the first thrombotic event, but the medication had been recently changed to aspirin 4 months before the second event. Emergent coronary angiography revealed thrombotic total occlusion of RCA with heavy thrombotic burden from middle RCA to the ostium of the posterior descending branch. Combination pharmacotherapy was performed with anticoagulants (heparin), fibrinolytics (urokinase), and Glycoprotein IIb/IIIa antagonists (abciximab), in addition to mechanical thrombosuction. However, on hospital day 2, the patient complained recurrent chest pain and again underwent coronary angiography, which revealed distal embolization of large thrombus to the posterior lateral branch. Coronary flow was recovered after repeated mechanical thrombosuction was performed. This case has shown the importance of aggressive combination drug therapy, accompanied by mechanical thrombosuction in patient with myocardial infarction due to thrombotic occlusion of coronary artery aneurysm and the importance of unceasing life-long anticoagulant therapy in those particular patients.
MeSH Terms
Figure
Reference
-
1. Nichols L, Lagana S, Parwani A. Coronary artery aneurysm: a review and hypothesis regarding etiology. Arch Pathol Lab Med. 2008; 132:823–828.
Article2. Pahlavan PS, Niroomand F. Coronary artery aneurysm: a review. Clin Cardiol. 2006; 29:439–443.
Article3. Iwai-Takano M, Oikawa M, Yamaki T, Yamaguchi O, Nakazato K, Ohsugi T, et al. A case of recurrent myocardial infarction caused by a giant right coronary artery aneurysm. J Am Soc Echocardiogr. 2007; 20:1318.e5–1318.e8.
Article4. Fulton DR, Newburger JW. Long-term cardiac sequelae of Kawasaki disease. Curr Rheumatol Rep. 2000; 2:324–329.
Article5. Everett JE, Burkhart HM. Coronary artery aneurysm: case report. J Cardiothorac Surg. 2008; 3:1.
Article6. Uhm JS, Park CS, Kim TS, Kim SY, Kim HJ, Park YK, et al. A case of acute myocardial infarction caused by coronary thrombus associated with a myocardial bridge and slow coronary flow. Korean Circ J. 2005; 35:639–642.
Article7. Rashdan I, Schechter E. Safety and efficacy of abciximab use in conjunction with intracoronary urokinase in patients requiring angioplasty. Catheter Cardiovasc Interv. 2000; 49:113–116.
Article8. Thiele H, Schindler K, Friedenberger J, Eitel I, Fürnau G, Grebe E, et al. Intracoronary compared with intravenous bolus abciximab application in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention: the randomized Leipzig immediate percutaneous coronary intervention abciximab IV versus IC in ST-elevation myocardial infarction trial. Circulation. 2008; 118:49–57.
Article9. Sezer M, Cimen A, Aslanger E, Elitok A, Umman B, Buğra Z, et al. Effect of intracoronary streptokinase administered immediately after primary percutaneous coronary intervention on long-term left ventricular infarct size, volumes, and function. J Am Coll Cardiol. 2009; 54:1065–1071.
Article10. Cortese B, Micheli A, Picchi A, Limbruno U. Combined, superselective pharmacological management of large coronary thrombus burden. J Invasive Cardiol. 2009; 21:168–171.11. Henriques JP, Zijlstra F, Ottervanger JP, de Boer MJ, van 't Hof AW, Hoorntje JC, et al. Incidence and clinical significance of distal embolization during primary angioplasty for acute myocardial infarction. Eur Heart J. 2002; 23:1112–1117.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Report of a Huge Coronary Artery Aneurysm with Acute Myocardial Infarction
- Acute Myocardial Infarction by Right Coronary Artery Occlusion Presenting as Precordial ST Elevation on Electrocardiography
- Two Cases of Multivessel Coronary Artery Ectasias Resulting in Acute Inferior Myocardial Infarction
- Detection of a Left Main Coronary Aneurysm with a Thrombus Presenting as an Acute Myocardial Infarction by Coronary Computed Tomographic Angiography
- Precordial ST-Segment Elevation in Acute Right Ventricular Myocardial Infarction