J Lipid Atheroscler.
2014 Dec;3(2):89-96. 10.12997/jla.2014.3.2.89.
Prevalence and Gender-Related Characteristics of Metabolic Syndrome in Korean Community
- Affiliations
-
- 1Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea. shkimmd@snu.ac.kr
- 2Hallym University Sacred Heart Hospital, Anyang, Korea.
- 3Bucheon St. Mary's Hospital, Catholic University College of Medicine, Bucheon, Korea.
- 4Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea.
- 5Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Cheil Hospital and Women's Health Care Center, Catholic Kwandong University College of Medicine, Seoul, Korea.
- KMID: 1773887
- DOI: http://doi.org/10.12997/jla.2014.3.2.89
Abstract
OBJECTIVE
There are still a limited number of studies assessing the prevalence of metabolic syndrome in the community. The aim of this study is to investigate the prevalence and gender-related characteristics of metabolic syndrome in Korean community.
METHODS
A total of 417 community subjects (mean age was 60.7+/-13.6 years, 35.3% were men) who attended the routine check-up were analyzed. National Cholesterol Education Program-Adult Treatment Panel (NCEP-ATP) III clinical guideline was used to define metabolic syndrome.
RESULTS
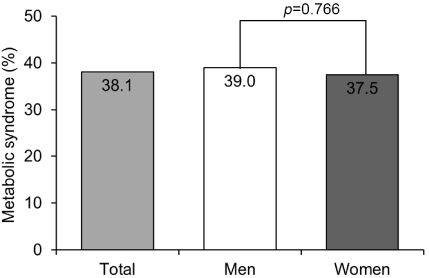
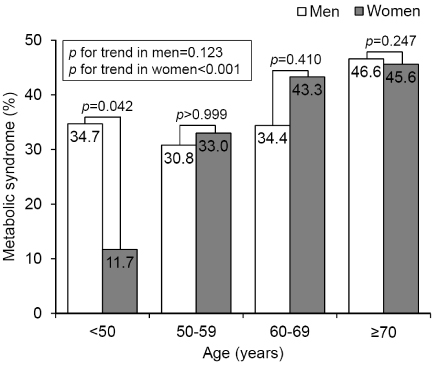
Metabolic syndrome was diagnosed in 38.1% of study subjects. The prevalence of metabolic syndrome was not different between men and women (men 39.0% vs. women 37.5%, p=0.766). The positive association between age and the prevalence of metabolic syndrome was more pronounced in women (chi2=17.52, p for trend<0.001) than men (chi2=2.38, p for trend=0.123). In young age group (<50 years), the prevalence of metabolic syndrome was higher in men than in women (34.7% vs. 11.7%, p=0.042). This gender difference was not observed in older group (> or =50 years). The most prevalent factor of metabolic syndrome was hypertriglyceridemia (49.9%) and hypertension (47.6%) in both genders. Among metabolic syndrome components, central obesity (40.5% vs. 25.2%, p=0.002) and hypertriglyceridemia (54.5% vs. 41.8%, p=0.015) were more prevalent in women than in men, and the prevalence of other components were similar between genders.
CONCLUSIONS
In the community, metabolic syndrome was highly prevalent in middle-aged and elderly Korean adult. Age related change in the prevalence of metabolic syndrome was gender specific. Age and gender effects should be considered for the effective control of metabolic syndrome in the community.
Keyword
MeSH Terms
Figure
Reference
-
1. Statistics Korea. Statistics of cause of death and birth 2013 [Internet]. Daejeon: Statistics Korea;2014. cited 2014 Nov 16. Available from: http://www.kostat.go.kr.2. Seo S. Economic burden of cardio-cerebrovascular diseases, 2008. Public Health Wkly Rep [Internet]. 2011. 03. 18. 4:1–5. updated 2012 Aug 25. cited 2014 Nov 16. Available from: http://www.cdc.go.kr/CDC/cms/content/95/12595_view.html.3. DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. 1991; 14:173–194.
Article4. Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005; 365:1415–1428.
Article5. Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988; 37:1595–1607.
Article6. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998; 15:539–553.
Article7. Alberti KG, Zimmet P, Shaw J. Metabolic syndrome--a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006; 23:469–480.
Article8. Isomaa B, Almgren P, Tuomi T, Forsén B, Lahti K, Nissén M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001; 24:683–689.
Article9. Cull CA, Jensen CC, Retnakaran R, Holman RR. Impact of the metabolic syndrome on macrovascular and microvascular outcomes in type 2 diabetes mellitus: United Kingdom Prospective Diabetes Study 78. Circulation. 2007; 116:2119–2126.
Article10. Kim MH, Kim MK, Choi BY, Shin YJ. Prevalence of the metabolic syndrome and its association with cardiovascular diseases in Korea. J Korean Med Sci. 2004; 19:195–201.
Article11. Suh S, Lee MK. Metabolic syndrome and cardiovascular diseases in Korea. J Atheroscler Thromb. 2014; 21:Suppl 1. S31–S35.
Article12. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002; 106:3143–3421.13. Tan CE, Ma S, Wai D, Chew SK, Tai ES. Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care. 2004; 27:1182–1186.
Article14. Hildrum B, Mykletun A, Hole T, Midthjell K, Dahl AA. Age-specific prevalence of the metabolic syndrome defined by the International Diabetes Federation and the National Cholesterol Education Program: the Norwegian HUNT 2 study. BMC Public Health. 2007; 7:220.
Article15. Lawlor DA, Smith GD, Ebrahim S. Does the new International Diabetes Federation definition of the metabolic syndrome predict CHD any more strongly than older definitions? Findings from the British Women's Heart and Health Study. Diabetologia. 2006; 49:41–48.
Article16. Vishram JK, Borglykke A, Andreasen AH, Jeppesen J, Ibsen H, Jørgensen T, et al. Impact of age and gender on the prevalence and prognostic importance of the metabolic syndrome and its components in Europeans. The MORGAM Prospective Cohort Project. PLoS One. 2014; 9:e107294.
Article17. Park HS, Kim SM, Lee JS, Lee J, Han JH, Yoon DK, et al. Prevalence and trends of metabolic syndrome in Korea: Korean National Health and Nutrition Survey 1998-2001. Diabetes Obes Metab. 2007; 9:50–58.
Article18. Lee K, Koh SB, Shin M, Ahn M, Kim JY, Yoo BS, et al. Prevalence and sex-related characteristics of metabolic syndrome in a Korean rural cohort. J Korean Soc Lipidol Atheroscler. 2008; 18:226–239.19. Lim J, Kim S, Ke S, Cho B. The prevalence of obesity, abdominal obesity and metabolic syndrome among elderly in general population. Korean J Fam Med. 2011; 32:128–134.
Article20. Lim S, Shin H, Song JH, Kwak SH, Kang SM, Won Yoon J, et al. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998-2007. Diabetes Care. 2011; 34:1323–1328.21. Ishii S, Tanaka T, Akishita M, Ouchi Y, Tuji T, Iijima K, et al. Metabolic syndrome, sarcopenia and role of sex and age: cross-sectional analysis of kashiwa cohort study. PLoS One. 2014; 9:e112718.
Article22. Liu J, Shi WQ, Cao Y, He LP, Guan K, Ling WH, et al. Higher serum carotenoid concentrations associated with a lower prevalence of the metabolic syndrome in middle-aged and elderly Chinese adults. Br J Nutr. 2014; 112:2041–2048.
Article23. Salas R, Bibiloni MD, Ramos E, Villarreal J, Pons A, Tur JA, et al. Metabolic syndrome prevalence among northern Mexican adult population. PLoS ONE. 2014; 9:e105581.
Article24. Heiss G, Snyder ML, Teng Y, Schneiderman N, Llabre MM, Cowie C, et al. Prevalence of metabolic syndrome among Hispanics/Latinos of diverse background: the Hispanic Community Health Study/Study of Latinos. Diabetes Care. 2014; 37:2391–2399.
Article25. Roh E, Ko SH, Kwon HS, Kim NH, Kim JH, Kim CS, et al. Prevalence and management of dyslipidemia in Korea: Korea National Health and Nutrition Examination Survey during 1998 to 2010. Diabetes Metab J. 2013; 37:433–449.
Article26. Kim MA. Triglyceride and cardiovascular disease. J Lipid Atheroscler. 2013; 2:1–8.
Article27. Hokanson JE, Austin MA. Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studies. J Cardiovasc Risk. 1996; 3:213–219.
Article28. Sarwar N, Danesh J, Eiriksdottir G, Sigurdsson G, Wareham N, Bingham S, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation. 2007; 115:450–458.
Article29. Haim M, Benderly M, Brunner D, Behar S, Graff E, Reicher-Reiss H, et al. Elevated serum triglyceride levels and long-term mortality in patients with coronary heart disease: the Bezafibrate Infarction Prevention (BIP) Registry. Circulation. 1999; 100:475–482.
Article30. Liu S, Manson JE. Dietary carbohydrates, physical inactivity, obesity, and the metabolic syndrome as predictors of coronary heart disease. Curr Opin Lipidol. 2001; 12:395–404.
Article31. Goff DC Jr, Gerstein HC, Ginsberg HN, Cushman WC, Margolis KL, Byington RP, et al. Prevention of cardiovascular disease in persons with type 2 diabetes mellitus: current knowledge and rationale for the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Am J Cardiol. 2007; 99:4i–20i.
Article32. Carr MC. The emergence of the metabolic syndrome with menopause. J Clin Endocrinol Metab. 2003; 88:2404–2411.
Article33. Tchernof A, Calles-Escandon J, Sites CK, Poehlman ET. Menopause, central body fatness, and insulin resistance: effects of hormone-replacement therapy. Coron Artery Dis. 1998; 9:503–511.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Prevalence and the Related Factors of Metabolic Syndrome in Urban and Rural Community
- Gender Differences in the Association of Socioeconomic Status with Metabolic Syndrome in Middle-Aged Koreans
- Gender Difference in Association with Socioeconomic Status and Incidence of Metabolic Syndrome in Korean Adults
- Association of Family Composition and Metabolic Syndrome in Korean Adults Aged over 45 Years Old
- Gender Differences between Metabolic Syndrome and Mental Health Problems in Adults Using Community Health Services