Pharmacologic Management of Chronic Pain
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, School of Medicine, The Catholic University of Korea, Seoul, Korea. demoon@catholic.ac.kr
- KMID: 1770541
- DOI: http://doi.org/10.3344/kjp.2010.23.2.99
Abstract
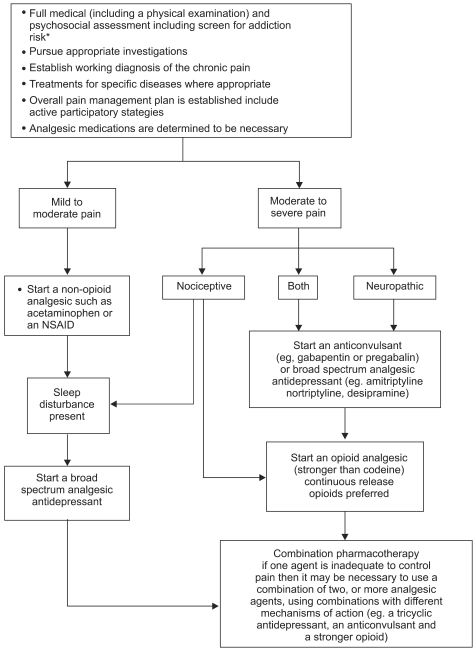
- Chronic pain is a multifactorial condition with both physical and psychological symptoms, and it affects around 20% of the population in the developed world. In spite of outstanding advances in pain management over the past decades, chronic pain remains a significant problem. This article provides a mechanism- and evidence-based approach to improve the outcome for pharmacologic management of chronic pain. The usual approach to treat mild to moderate pain is to start with a nonopioid analgesic. If this is inadequate, and if there is an element of sleep deprivation, then it is reasonable to add an antidepressant with analgesic qualities. If there is a component of neuropathic pain or fibromyalgia, then a trial with one of the gabapentinoids is appropriate. If these steps are inadequate, then an opioid analgesic may be added. For moderate to severe pain, one would initiate an earlier trial of a long term opioid. Skeletal muscle relaxants and topicals may also be appropriate as single agents or in combination. Meanwhile, the steps of pharmacologic treatments for neuropathic pain include (1) certain antidepressants (tricyclic antidepressants, serotonin and norepinephrine reuptake inhibitors), calcium channel alpha2-delta ligands (gabapentin and pregabalin) and topical lidocaine, (2) opioid analgesics and tramadol (for first-line use in selected clinical circumstances) and (3) certain other antidepressant and antiepileptic medications (topical capsaicin, mexiletine, and N-methyl-d-aspartate receptor antagonists). It is essential to have a thorough understanding about the different pain mechanisms of chronic pain and evidence-based multi-mechanistic treatment. It is also essential to increase the individualization of treatment.
Keyword
MeSH Terms
-
Analgesics, Opioid
Antidepressive Agents
Calcium Channels
Capsaicin
Chronic Pain
Fibromyalgia
Lidocaine
Ligands
Mexiletine
N-Methylaspartate
Neuralgia
Neuromuscular Agents
Norepinephrine
Pain Management
Serotonin
Sleep Deprivation
Tramadol
Analgesics, Opioid
Antidepressive Agents
Calcium Channels
Capsaicin
Lidocaine
Ligands
Mexiletine
N-Methylaspartate
Neuromuscular Agents
Norepinephrine
Serotonin
Tramadol
Figure
Cited by 10 articles
-
Current pharmacological management of chronic pain
Joong Chul Park, Youn Seon Choi, Jung Hyun Kim
J Korean Med Assoc. 2010;53(9):815-823. doi: 10.5124/jkma.2010.53.9.815.Analgesic Efficacy and Safety of Prolonged-Release Oxycodone/Naloxone in Korean Patients with Chronic Pain from Spinal Disorders
Chang Ju Hwang, Sung Soo Chung, Kyu-Yeol Lee, Jae Hyup Lee, Seong-Hwan Moon, Jin-Hyok Kim, Kyu-Jung Cho, Jae-Sung Ahn, Dong-Soo Kim, Ye-Soo Park, Hye-Jeong Park
Clin Orthop Surg. 2018;10(1):33-40. doi: 10.4055/cios.2018.10.1.33.Pregnancy in Woman with Spinal Cord Stimulator for Complex Regional Pain Syndrome: A Case Report and Review of the Literature
Hyung Seok Yoo, Francis Sahngun Nahm, Kyoung Hoon Yim, Jee Youn Moon, Yung Suk Kim, Pyung Bok Lee
Korean J Pain. 2010;23(4):266-269. doi: 10.3344/kjp.2010.23.4.266.Chronic Pain and Its Determinants: A Population-based Study in Southern Iran
Safar Zarei, Shiva Bigizadeh, Mohammad Pourahmadi, Mohamed Amin Ghobadifar
Korean J Pain. 2012;25(4):245-253. doi: 10.3344/kjp.2012.25.4.245.Acute Systemic Infusion of Bupropion Decrease Formalin Induced Pain Behavior in Rat
Somayyeh Naderi, Firouz Ghaderi Pakdel, Mostafa Ashrafi Osalou, Ulker Cankurt
Korean J Pain. 2014;27(2):118-124. doi: 10.3344/kjp.2014.27.2.118.Guidelines for prescribing opioids for chronic non-cancer pain in Korea
Eung Don Kim, Jin Young Lee, Ji Seon Son, Gyeong Jo Byeon, Jin Seok Yeo, Do Wan Kim, Sie Hyeon Yoo, Ji Hee Hong, Hue Jung Park,
Korean J Pain. 2017;30(1):18-33. doi: 10.3344/kjp.2017.30.1.18.Low doses of amitriptyline, pregabalin, and gabapentin are preferred for management of neuropathic pain in India: is there a need for revisiting dosing recommendations?
Sanjay Vasant Kamble, Salman Abdulrehman Motlekar, Lyndon Lincoln D'souza, Vinay Nanda Kudrigikar, Sameer Eknath Rao
Korean J Pain. 2017;30(3):183-191. doi: 10.3344/kjp.2017.30.3.183.Therapeutic alternatives in painful diabetic neuropathy: a meta-analysis of randomized controlled trials
Samuel Vilar, Jose Manuel Castillo, Pedro V. Munuera Martínez, María Reina, Manuel Pabón
Korean J Pain. 2018;31(4):253-260. doi: 10.3344/kjp.2018.31.4.253.Double blind randomized control trial to evaluate the efficacy of ketoprofen patch to attenuate pain during venous cannulation
Sanjay Kumar, Omprakash Sanjeev, Anil Agarwal, Chetna Shamshery, Rakhi Gupta
Korean J Pain. 2018;31(1):39-42. doi: 10.3344/kjp.2018.31.1.39.Serotonin syndrome in a patient with chronic pain taking analgesic drugs mistaken for psychogenic nonepileptic seizure: a case report
Mathieu Boudier-Revéret, Min Cheol Chang
Yeungnam Univ J Med. 2021;38(4):371-373. doi: 10.12701/yujm.2021.00948.
Reference
-
1. Kroenke K, Krebs EE, Bair MJ. Pharmacotherapy of chronic pain: a synthesis of recommendations from systematic reviews. Gen Hosp Psychiatry. 2009; 31:206–219. PMID: 19410099.
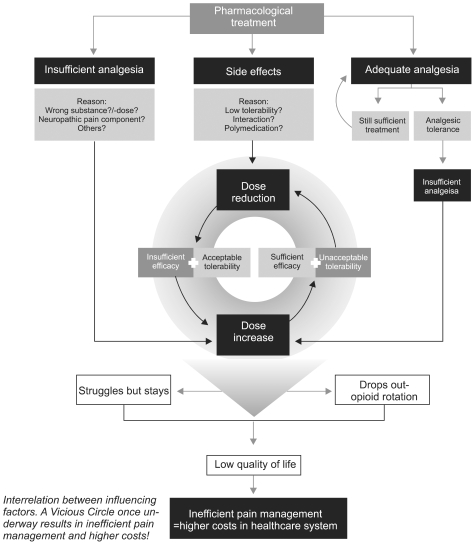
Article2. Varrassi G, Müller-Schwefe G, Pergolizzi J, Orónska A, Morlion B, Mavrocordatos P, et al. Pharmacological treatment of chronic pain - the need for CHANGE. Curr Med Res Opin. 2010; 26:1231–1245. PMID: 20337502.
Article3. Treede RD, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, Griffin JW, et al. Neuropathic pain: redefinition and a grading system for clinical research purposes. Neurology. 2008; 70:1630–1635. PMID: 18003941.
Article4. Torrance N, Smith BH, Watson MC, Bennett MI. Medication and treatment use in primary care patients with chronic pain of predominantly neuropathic origin. Fam Pract. 2007; 24:481–485. PMID: 17670804.
Article5. Smith BH, Torrance N, Bennett MI, Lee AJ. Health and quality of life associated with chronic pain of predominantly neuropathic origin in the community. Clin J Pain. 2007; 23:143–149. PMID: 17237663.
Article6. Roelofs PD, Deyo RA, Koes BW, Scholten RJ, van Tulder MW. Nonsteroidal anti-inflammatory drugs for low back pain: an updated Cochrane review. Spine. 2008; 33:1766–1774. PMID: 18580547.
Article7. Antman EM, Bennett JS, Daugherty A, Furberg C, Roberts H, Taubert KA. Use of nonsteroidal antiinflammatory drugs: an update for clinicians: a scientific statement from the American Heart Association. Circulation. 2007; 115:1634–1642. PMID: 17325246.8. Lee C, Straus WL, Balshaw R, Barlas S, Vogel S, Schnitzer TJ. A comparison of the efficacy and safety of nonsteroidal antiinflammatory agents versus acetaminophen in the treatment of osteoarthritis: a meta-analysis. Arthritis Rheum. 2004; 51:746–754. PMID: 15478167.
Article9. Towheed TE, Maxwell L, Judd MG, Catton M, Hochberg MC, Wells G. Acetaminophen for osteoarthritis. Cochrane Database Syst Rev. 2006; 1:CD004257. PMID: 16437479.
Article10. Wegman A, van der Windt D, van Tulder M, Stalman W, de Vries T. Nonsteroidal antiinflammatory drugs or acetaminophen for osteoarthritis of the hip or knee? A systematic review of evidence and guidelines. J Rheumatol. 2004; 31:344–354. PMID: 14760807.11. Watkins PB, Kaplowitz N, Slattery JT, Colonese CR, Colucci SV, Stewart PW, et al. Aminotransferase elevations in healthy adults receiving 4 grams of acetaminophen daily: a randomized controlled trial. JAMA. 2006; 296:87–93. PMID: 16820551.
Article12. Bonezzi C, Allegri M, Demartini L, Buonocore M. The pharmacological treatment of neuropathic pain. Eur J Pain Suppl. 2009; 3:85–88.
Article13. McDiarmid T, Mackler L, Schneider DM. Clinical inquiries. What is the addiction risk associated with tramadol? J Fam Pract. 2005; 54:72–73. PMID: 15623411.14. Sansone RA, Sansone LA. Tramadol: seizures, serotonin syndrome, and coadministered antidepressants. Psychiatry (Edgmont). 2009; 6:17–21. PMID: 19724727.15. Lynch ME. The pharmacotherapy of chronic pain. Rheum Dis Clin North Am. 2008; 34:369–385. PMID: 18638682.
Article16. Furlan AD, Sandoval JA, Mailis-Gagnon A, Tunks E. Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects. CMAJ. 2006; 174:1589–1594. PMID: 16717269.
Article17. Jovey RD, Ennis J, Gardner-Nix J, Goldman B, Hays H, Lynch M, et al. Use of opioid analgesics for the treatment of chronic noncancer pain--a consensus statement and guidelines from the Canadian Pain Society, 2002. Pain Res Manag. 2003; 8(Suppl A):3A–28A.18. Lynch ME, Watson CP. The pharmacotherapy of chronic pain: a review. Pain Res Manag. 2006; 11:11–38. PMID: 16511612.
Article19. Lynch ME. A review of the use of methadone for the treatment of chronic noncancer pain. Pain Res Manag. 2005; 10:133–144. PMID: 16175249.
Article20. Fine PG, Mahajan G, McPherson ML. Long-acting opioids and short-acting opioids: appropriate use in chronic pain management. Pain Med. 2009; 10(Suppl 2):S79–S88. PMID: 19691687.
Article21. Moore RA, McQuay HJ. Prevalence of opioid adverse events in chronic non-malignant pain: systematic review of randomised trials of oral opioids. Arthritis Res Ther. 2005; 7:R1046–R1051. PMID: 16207320.22. Eisenberg E, McNicol E, Carr DB. Opioids for neuropathic pain. Cochrane Database Syst Rev. 2006; 3:CD006146. PMID: 16856116.
Article23. Ballantyne JC, Mao J. Opioid therapy for chronic pain. N Engl J Med. 2003; 349:1943–1953. PMID: 14614170.
Article24. Daniell HW. Hypogonadism in men consuming sustained-action oral opioids. J Pain. 2002; 3:377–384. PMID: 14622741.
Article25. Daniell HW. Opioid endocrinopathy in women consuming prescribed sustained-action opioids for control of nonmalignant pain. J Pain. 2008; 9:28–36. PMID: 17936076.
Article26. Højsted J, Sjøgren P. An update on the role of opioids in the management of chronic pain of nonmalignant origin. Curr Opin Anaesthesiol. 2007; 20:451–455. PMID: 17873598.
Article27. Fishbain DA, Cutler RB, Rosomoff HL, Rosomoff RS. Are opioid-dependent/tolerant patients impaired in driving-related skills? A structured evidence-based review. J Pain Symptom Manage. 2003; 25:559–577. PMID: 12782437.
Article28. McQuay HJ, Tramér M, Nye BA, Carroll D, Wiffen PJ, Moore RA. A systematic review of antidepressants in neuropathic pain. Pain. 1996; 68:217–227. PMID: 9121808.
Article29. Collins SL, Moore RA, McQuay HJ, Wiffen P. Antidepressants and anticonvulsants for diabetic neuropathy and postherpetic neuralgia: a quantitative systematic review. J Pain Symptom Manage. 2000; 20:449–458. PMID: 11131263.
Article30. Mendell JR, Sahenk Z. Clinical practice. Painful sensory neuropathy. N Engl J Med. 2003; 348:1243–1255. PMID: 12660389.31. Jung AC, Staiger T, Sullivan M. The efficacy of selective serotonin reuptake inhibitors for the management of chronic pain. J Gen Intern Med. 1997; 12:384–389. PMID: 9192257.
Article32. Goldstein DJ, Lu Y, Detke MJ, Lee TC, Iyengar S. Duloxetine vs. placebo in patients with painful diabetic neuropathy. Pain. 2005; 116:109–118. PMID: 15927394.
Article33. Raskin J, Pritchett YL, Wang F, D'Souza DN, Waninger AL, Iyengar S, et al. A double-blind, randomized multicenter trial comparing duloxetine with placebo in the management of diabetic peripheral neuropathic pain. Pain Med. 2005; 6:346–356. PMID: 16266355.
Article34. Wernicke JF, Pritchett YL, D'Souza DN, Waninger A, Tran P, Iyengar S, et al. A randomized controlled trial of duloxetine in diabetic peripheral neuropathic pain. Neurology. 2006; 67:1411–1420. PMID: 17060567.
Article35. Perahia DG, Pritchett YL, Desaiah D, Raskin J. Efficacy of duloxetine in painful symptoms: an analgesic or antidepressant effect? Int Clin Psychopharmacol. 2006; 21:311–317. PMID: 17012978.
Article36. Arnold LM, Lu Y, Crofford LJ, Wohlreich M, Detke MJ, Iyengar S, et al. A double-blind, multicenter trial comparing duloxetine with placebo in the treatment of fibromyalgia patients with or without major depressive disorder. Arthritis Rheum. 2004; 50:2974–2984. PMID: 15457467.
Article37. Arnold LM, Rosen A, Pritchett YL, D'Souza DN, Goldstein DJ, Iyengar S, et al. A randomized, double-blind, placebo-controlled trial of duloxetine in the treatment of women with fibromyalgia with or without major depressive disorder. Pain. 2005; 119:5–15. PMID: 16298061.
Article38. Arnold LM, Pritchett YL, D'Souza DN, Kajdasz DK, Iyengar S, Wernicke JF. Duloxetine for the treatment of fibromyalgia in women: pooled results from two randomized, placebo-controlled clinical trials. J Womens Health (Larchmt). 2007; 16:1145–1156. PMID: 17937567.
Article39. Rowbotham M, Goli V, Kunz NR, Lei D. Venlafaxine extended release in the treatment of painful diabetic neuropathy: a double-blind, placebo-controlled study. Pain. 2004; 110:697–706. PMID: 15288411.
Article40. Grothe DR, Scheckner B, Albano D. Treatment of pain syndromes with venlafaxine. Pharmacotherapy. 2004; 24:621–629. PMID: 15162896.
Article41. Spielmans GI. Duloxetine does not relieve painful physical symptoms in depression: a meta-analysis. Psychother Psychosom. 2008; 77:12–16. PMID: 18087203.
Article42. Krebs EE, Gaynes BN, Gartlehner G, Hansen RA, Thieda P, Morgan LC, et al. Treating the physical symptoms of depression with second-generation antidepressants: a systematic review and metaanalysis. Psychosomatics. 2008; 49:191–198. PMID: 18448772.
Article43. Brecht S, Courtecuisse C, Debieuvre C, Croenlein J, Desaiah D, Raskin J, et al. Efficacy and safety of duloxetine 60 mg once daily in the treatment of pain in patients with major depressive disorder and at least moderate pain of unknown etiology: a randomized controlled trial. J Clin Psychiatry. 2007; 68:1707–1716. PMID: 18052564.
Article44. Carlton SM, Zhou S. Attenuation of formalin-induced nociceptive behaviors following local peripheral injection of gabapentin. Pain. 1998; 76:201–207. PMID: 9696474.
Article45. Field MJ, Holloman EF, McCleary S, Hughes J, Singh L. Evaluation of gabapentin and S-(+)-3-isobutylgaba in a rat model of postoperative pain. J Pharmacol Exp Ther. 1997; 282:1242–1246. PMID: 9316831.46. Chen SR, Xu Z, Pan HL. Stereospecific effect of pregabalin on ectopic afferent discharges and neuropathic pain induced by sciatic nerve ligation in rats. Anesthesiology. 2001; 95:1473–1479. PMID: 11748408.
Article47. McQuay H, Carroll D, Jadad AR, Wiffen P, Moore A. Anticonvulsant drugs for management of pain: a systematic review. BMJ. 1995; 311:1047–1052. PMID: 7580659.
Article48. van Tulder MW, Touray T, Furlan AD, Solway S, Bouter LM. Cochrane Back Review Group. Muscle relaxants for nonspecific low back pain: a systematic review within the framework of the cochrane collaboration. Spine. 2003; 28:1978–1992. PMID: 12973146.
Article49. Chong MS, Hester J. Diabetic painful neuropathy: current and future treatment options. Drugs. 2007; 67:569–585. PMID: 17352515.50. Mason L, Moore RA, Derry S, Edwards JE, McQuay HJ. Systematic review of topical capsaicin for the treatment of chronic pain. BMJ. 2004; 328:991. PMID: 15033881.
Article51. Mason L, Moore RA, Edwards JE, McQuay HJ, Derry S, Wiffen PJ. Systematic review of efficacy of topical rubefacients containing salicylates for the treatment of acute and chronic pain. BMJ. 2004; 328:995. PMID: 15033879.
Article52. Underwood M, Ashby D, Cross P, Hennessy E, Letley L, Martin J, et al. Advice to use topical or oral ibuprofen for chronic knee pain in older people: randomised controlled trial and patient preference study. BMJ. 2008; 336:138–142. PMID: 18056743.
Article53. Nandi R, Beacham D, Middleton J, Koltzenburg M, Howard RF, Fitzgerald M. The functional expression of mu opioid receptors on sensory neurons is developmentally regulated; morphine analgesia is less selective in the neonate. Pain. 2004; 111:38–50. PMID: 15327807.
Article54. Lönnqvist PA, Morton NS. Postoperative analgesia in infants and children. Br J Anaesth. 2005; 95:59–68. PMID: 15668207.
Article55. Bhatt DL, Scheiman J, Abraham NS, Antman EM, Chan FK, Furberg CD, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation. 2008; 118:1894–1909. PMID: 18836135.
Article56. Barkin RL, Barkin SJ, Barkin DS. Pharmacotherapeutic management of pain with a focus directed at the geriatric patient. Rheum Dis Clin North Am. 2007; 33:1–31. PMID: 17367690.
Article57. Barkin RL, Sable KS. Caution recommended for prescribing and administering COX-1/COX-2 and COX-2 specific NSAIDs. P T. 2000; 25:196–202.58. Innes GD, Zed PJ. Basic pharmacology and advances in emergency medicine. Emerg Med Clin North Am. 2005; 23:433–465. PMID: 15829391.
Article59. Murphy EJ. Acute pain management pharmacology for the patient with concurrent renal or hepatic disease. Anaesth Intensive Care. 2005; 33:311–322. PMID: 15973913.
Article60. Davies G, Kingswood C, Street M. Pharmacokinetics of opioids in renal dysfunction. Clin Pharmacokinet. 1996; 31:410–422. PMID: 8968655.
Article61. Stern SS, Ponticello MN. Current concepts in pain management: pharmacologic options for the pediatric, geriatric, hepatic and renal failure patient. Clin Podiatr Med Surg. 2008; 25:381–407. PMID: 18486851.
Article62. O'Connor AB, Dworkin RH. Treatment of neuropathic pain: an overview of recent guidelines. Am J Med. 2009; 122(Suppl 10):S22–S32. PMID: 19801049.