Korean J Ophthalmol.
2010 Dec;24(6):331-335. 10.3341/kjo.2010.24.6.331.
Clinical Features, Predisposing Factors, and Treatment Outcomes of Scleritis in the Korean Population
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. wrwee@snu.ac.kr
- 2Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea.
- KMID: 1769085
- DOI: http://doi.org/10.3341/kjo.2010.24.6.331
Abstract
- PURPOSE
To evaluate the clinical features, associated factors, and treatment outcomes of scleritis in the Korean population.
METHODS
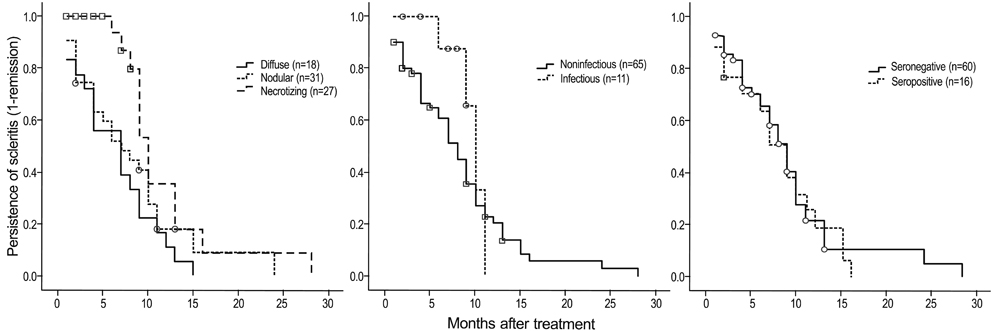
Medical records were retrospectively reviewed for 94 eyes of 76 patients with scleritis. Clinical features of scleritis, including systemic disease, presence of microorganisms, serologic markers, history of previous ocular surgery, and use of immunosuppressants were investigated and compared amongst the subtypes of scleritis. Treatment outcomes were evaluated using best corrected visual acuity (BCVA) and time to scleritis remission.
RESULTS
Nodular scleritis was the most common form observed, followed by necrotizing scleritis with inflammation, diffuse scleritis, and necrotizing scleritis without inflammation, respectively. A total of 16 of 76 patients (21.1%) had connective tissue diseases. Eleven cases (14.5%) had infectious scleritis, of which bacteria (54.5%) and fungi (45.5%) were the causative microorganisms. Thirty-three patients (43.4%) had previous ocular surgery, mostly pterygium excision. Notably, a history of pterygium excision was significantly associated with development of necrotizing and infectious scleritis (odds ratio [OR], 399 and 10.1; p < 0.001 and 0.002, respectively). In addition, patients with necrotizing scleritis were more likely to have infectious scleritis (OR, 11.7; p = 0.001). BCVA after treatment and time to remission also showed significant differences among the different scleritis subtypes. Systemic immunosuppression was required in addition to steroids for treating diffuse and necrotizing scleritis.
CONCLUSIONS
Careful taking of patient history including previous pterygium excision should be performed, especially in patients with necrotizing and infectious scleritis. In addition, evaluation of microbiological infection can be crucial for patients with necrotizing scleritis and history of pterygium excision.
MeSH Terms
-
Adolescent
Adult
Aged
Aged, 80 and over
*Asian Continental Ancestry Group
Bacterial Infections
Child
Eyeglasses
Female
Humans
Male
Medical Records
Middle Aged
Mycoses
Postoperative Period
Pterygium/surgery
Retrospective Studies
Scleritis/classification/ethnology/*etiology/*surgery
Treatment Outcome
Visual Acuity
Young Adult
Figure
Cited by 1 articles
-
Anterior segment eye diseases associated with rheumatic diseases
Joon Young Hyon
J Korean Med Assoc. 2016;59(1):45-51. doi: 10.5124/jkma.2016.59.1.45.
Reference
-
1. Akpek EK, Thorne JE, Qazi FA, et al. Evaluation of patients with scleritis for systemic disease. Ophthalmology. 2004. 111:501–506.2. Sainz de la Maza M, Jabbur NS, Foster CS. Severity of scleritis and episcleritis. Ophthalmology. 1994. 101:389–396.3. Tuft SJ, Watson PG. Progression of scleral disease. Ophthalmology. 1991. 98:467–471.4. Watson PG, Hayreh SS, Awdry PN. Episcleritis and scleritis. I. Br J Ophthalmol. 1968. 52:278–279.5. Sainz de la Maza M, Foster CS, Jabbur NS. Scleritis associated with rheumatoid arthritis and with other systemic immune-mediated diseases. Ophthalmology. 1994. 101:1281–1286.6. Erkanli L, Akova YA, Guney-Tefekli E, Tugal-Tutkun I. Clinical features, prognosis, and treatment results of patients with scleritis from 2 tertiary eye care centers in Turkey. Cornea. 2010. 29:26–33.7. Lee JE, Oum BS, Choi HY, Lee JS. Methicillin-resistant Staphylococcus aureus sclerokeratitis after pterygium excision. Cornea. 2007. 26:744–746.8. O'Donoghue E, Lightman S, Tuft S, Watson P. Surgically induced necrotising sclerokeratitis (SINS): precipitating factors and response to treatment. Br J Ophthalmol. 1992. 76:17–21.9. Su CY, Tsai JJ, Chang YC, Lin CP. Immunologic and clinical manifestations of infectious scleritis after pterygium excision. Cornea. 2006. 25:663–666.10. Huang FC, Huang SP, Tseng SH. Management of infectious scleritis after pterygium excision. Cornea. 2000. 19:34–39.11. Jabs DA, Mudun A, Dunn JP, Marsh MJ. Episcleritis and scleritis: clinical features and treatment results. Am J Ophthalmol. 2000. 130:469–476.12. Singh RP, McCluskey P. Scedosporium prolificans sclerokeratitis 10 years after pterygium excision with adjunctive mitomycin C. Clin Experiment Ophthalmol. 2005. 33:433–434.13. Jain V, Garg P, Sharma S. Microbial scleritis-experience from a developing country. Eye (Lond). 2009. 23:255–261.14. Hsiao CH, Chen JJ, Huang SC, et al. Intrascleral dissemination of infectious scleritis following pterygium excision. Br J Ophthalmol. 1998. 82:29–34.15. Lincoff HA, McLean JM, Nano H. Scleral abscess. I. A complication of retinal detachment. Buckling procedures. Arch Ophthalmol. 1965. 74:641–648.16. Margo CE, Polack FM, Hood CI. Aspergillus panophthalmitis complicating treatment of pterygium. Cornea. 1988. 7:285–289.17. Milauskas AT, Duke JR. Mycotic scleral abscess. Report of a case following a scleral buckling operation for retinal detachment. Am J Ophthalmol. 1967. 63:951–954.18. Lin CP, Shih MH, Tsai MC. Clinical experiences of infectious scleral ulceration: a complication of pterygium operation. Br J Ophthalmol. 1997. 81:980–983.19. Hoang LT, Lim LL, Vaillant B, et al. Antineutrophil cytoplasmic antibody-associated active scleritis. Arch Ophthalmol. 2008. 126:651–655.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Features and Treatment Outcomes in Patients with Infectious Scleritis
- Clinical Features of the Episcleritis and the Scleritis
- Effect of Intravitreal Dexamethasone Implant Injection in a Patient with Recurrent Nodular Anterior Scleritis
- Retinal Pigment Epithelial Detachment in Posterior Scleritis
- Two Cases of Necrotizing Scleritis After Pars Plana Vitrectomy