Korean J Radiol.
2008 Jun;9(3):258-267. 10.3348/kjr.2008.9.3.258.
Peripheral Arteriovenous Malformations with a Dominant Outflow Vein: Results of Ethanol Embolization
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Sungkyunkwan University School of Medicine, Seoul, Korea. ysdo@skku.edu
- 2Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1758460
- DOI: http://doi.org/10.3348/kjr.2008.9.3.258
Abstract
OBJECTIVE
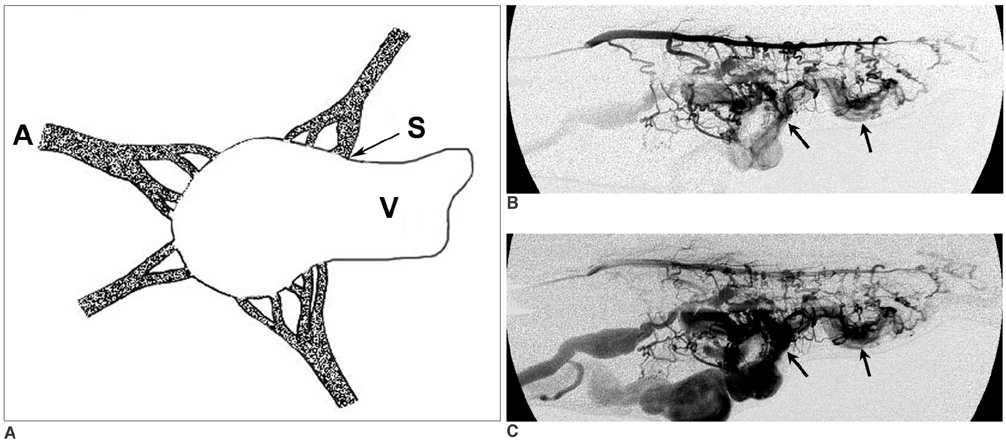
To assess retrospectively the treatment results of ethanol embolization of peripheral arteriovenous malformations (AVMs) with a dominant outflow vein (DOV). MATERIALS AND METHODS: Nineteen patients who had peripheral AVMs with a DOV were enrolled in this study (mean age, 29.7 years; range, 15-42 years). Fifty-one ethanol embolizations (mean, 2.7; range, 1-8) were performed by direct puncture (n = 29), the transarterial approach (n = 13), the transvenous approach (n = 5), or a combination of methods (n = 4) under general anesthesia. Coil and/or core-removed guide wire embolization of the DOV or another flow occlusion technique (i.e., use of an external pneumatic pressure cuff) to achieve vascular stasis were required in all patients during ethanol embolization. Clinical follow-up (mean, 22.2 months; range, 1-53 months) was performed for all patients, and imaging follow-up (mean, 22.1 months; range, 2-53 months) from the last treatment session was performed for 14 patients. The therapeutic outcome (cure, improvement, no change, or aggravation) was assessed according to the clinical response and the degree of devascularization at angiography. RESULTS: Ethanol embolization was considered as an effective procedure in all patients. Thirteen (68%) of 19 patients were cured and six displayed improvement. Three of six patients with improvement needed further treatment sessions for residual AVMs. Four patients (21%) experienced a total of eight complications. Five complications (three events of a distal embolism and one event each of a urinary bladder necrosis and a brain infarct related to the accidental cannulation of the common carotid artery during insertion of the Swan-Ganz catheter) were major and three complications (skin necrosis) were minor. CONCLUSION: Peripheral AVMs with a DOV can be effectively treated with a high cure rate by the use of ethanol embolization alone or in conjunction with the use of coil and/or core-removed guide wire embolization.
Keyword
MeSH Terms
Figure
Reference
-
1. Nakano J, Deschryver C. Effects of arteriovenous fistula on systemic and pulmonary circulations. Am J Physiol. 1964. 207:1319–1324.2. Pritchard DA, Maloney JD, Bernatz PE, Symmonds RE, Stanson AW. Surgical treatment of congenital pelvic arteriovenous malformation. Mayo Clin Proc. 1978. 53:607–611.3. Yakes WF, Rossi P, Odink H. How I do it. Arteriovenous malformation management. Cardiovasc Intervent Radiol. 1996. 19:65–67.4. Kaufman SL, Kumar AA, Roland JM, Harrington DP, Barth KH, Haller JA Jr, et al. Transcatheter embolization in the management of congenital arteriovenous malformations. Radiology. 1980. 137:21–29.5. Widlus DM, Murray RR, White RI Jr, Osterman FA Jr, Schreiber ER, Satre RW, et al. Congenital arteriovenous malformations: tailored embolotherapy. Radiology. 1988. 169:511–516.6. Yakes WF, Luethke JM, Merland JJ, Rak KM, Slater DD, Hollis HW, et al. Ethanol embolization of arteriovenous fistulas: a primary mode of therapy. J Vasc Interv Radiol. 1990. 1:89–96.7. Yakes WF, Pevsner P, Reed M, Donohue HJ, Ghaed N. Serial embolizations of an extremity arteriovenous malformation with alcohol via direct percutaneous puncture. AJR Am J Roentgenol. 1986. 146:1038–1040.8. Gomes AS. Embolization therapy of congenital arteriovenous malformations: use of alternate approaches. Radiology. 1994. 190:191–198.9. Jackson JE, Mansfield AO, Allison DJ. Treatment of high-flow vascular malformations by venous embolization aided by flow occlusion techniques. Cardiovasc Intervent Radiol. 1996. 19:323–328.10. Do YS, Yakes WF, Shin SW, Lee BB, Kim DI, Liu WC, et al. Ethanol embolization of arteriovenous malformations: interim results. Radiology. 2005. 235:674–682.11. Tan KT, Simons ME, Rajan DK, Terbrugge K. Peripheral highflow arteriovenous vascular malformations: a single-center experience. J Vasc Interv Radiol. 2004. 15:1071–1080.12. Cho SK, Do YS, Shin SW, Kim DI, Kim YW, Park KB, et al. Arteriovenous malformations of the body and extremities: analysis of therapeutic outcomes and approaches according to a modified angiographic classification. J Endovasc Ther. 2006. 13:527–538.13. In : Yee DC, Yakes WF, editors. Dominant outflow vein occlusion of high-flow malformations [abstract]. 2003. the 28th Annual Meeting of the Society of Interventional Radiology; March 2003; Salt Lake City, Utah, USA.14. Houdart E, Gobin YP, Casasco A, Aymard A, Herbreteau D, Merland JJ. A proposed angiographic classification of intracranial arteriovenous fistulae and malformations. Neuroradiology. 1993. 35:381–385.15. Shin BS, Do YS, Lee BB, Kim DI, Chung IS, Cho HS, et al. Multistage ethanol sclerotherapy of soft-tissue arteriovenous malformations: effect on pulmonary arterial pressure. Radiology. 2005. 235:1072–1077.16. White RI Jr, Pollak J, Persing J, Henderson KJ, Thomson JG, Burdge CM. Long-term outcome of embolotherapy and surgery for high-flow extremity arteriovenous malformations. J Vasc Interv Radiol. 2000. 11:1285–1295.17. Osuga K, Hori S, Kitayoshi H, Khankan AA, Okada A, Sugiura T, et al. Embolization of high flow arteriovenous malformations: experience with use of superabsorbent polymer microspheres. J Vasc Interv Radiol. 2002. 13:1125–1133.18. Palmaz JC, Newton TH, Reuter SR, Bookstein JJ. Particulate intraarterial embolization in pelvic arteriovenous malformations. AJR Am J Roentgenol. 1981. 137:117–122.19. Schweitzer JS, Chang BS, Madsen P, Vinuela F, Martin NA, Marroquin CE, et al. The pathology of arteriovenous malformations of the brain treated by embolotherapy. II. Results of embolization with multiple agents. Neuroradiology. 1993. 35:468–474.20. Rao VR, Mandalam KR, Gupta AK, Kumar S, Joseph S. Dissolution of isobutyl 2-cyanoacrylate on long-term follow-up. AJNR Am J Neuroradiol. 1989. 10:135–141.21. Germano IM, Davis RL, Wilson CB, Hieshima GB. Histopathological follow-up study of 66 cerebral arteriovenous malformations after therapeutic embolization with polyvinyl alcohol. J Neurosurg. 1992. 76:607–614.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nonsurgical Treatment of Congenital Vascular Malformations of the Trunk and Limb by Transcatheter Embolization
- Adequate time of initiation of continuous infusion of nitroglycerin for controlling pulmonary arterial pressure during ethanol embolotherapy of congenital arteriovenous malformation of the extremities
- Arteriovenous Fistula at Scalp: Rapid Progression After Embolization of Contralateral Facial Arteriovenous Malformation
- A Case of Multiple Pulmonary Arteriovenous Malformation Treated with Coil Embolization
- Ethanol Embolization of Arteriovenous Malformations: Results and Complications of 33 Cases