Clin Orthop Surg.
2011 Sep;3(3):202-210. 10.4055/cios.2011.3.3.202.
MR-based Parameters as a Supplement to Radiographs in Managing Developmental Hip Dysplasia
- Affiliations
-
- 1Department of Orthopaedic Surgery, Medical Research Institute, Pusan National University Hospital, Busan, Korea. kimht@pusan.ac.kr
- KMID: 1743910
- DOI: http://doi.org/10.4055/cios.2011.3.3.202
Abstract
- BACKGROUND
Some dysplastic hips with favorable radiographic parameters fail to develop normally, suggesting that we should consider cartilaginous or soft tissue structures for further information regarding the condition of the hip. The purpose of this study was to provide a clear definition of concentric reduction in developmental dysplasia of the hip (DDH) based on magnetic resonance imaging (MRI), and to determine how radiographic and MR-based parameters could be used together to treat dysplastic hips.
METHODS
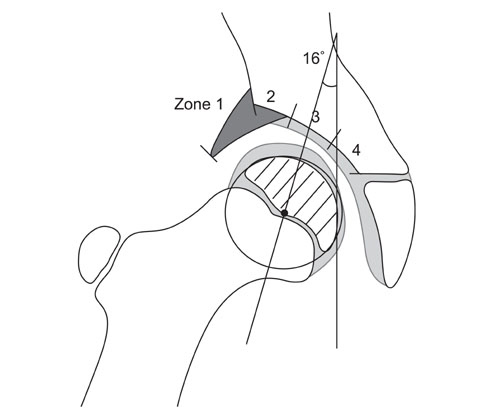
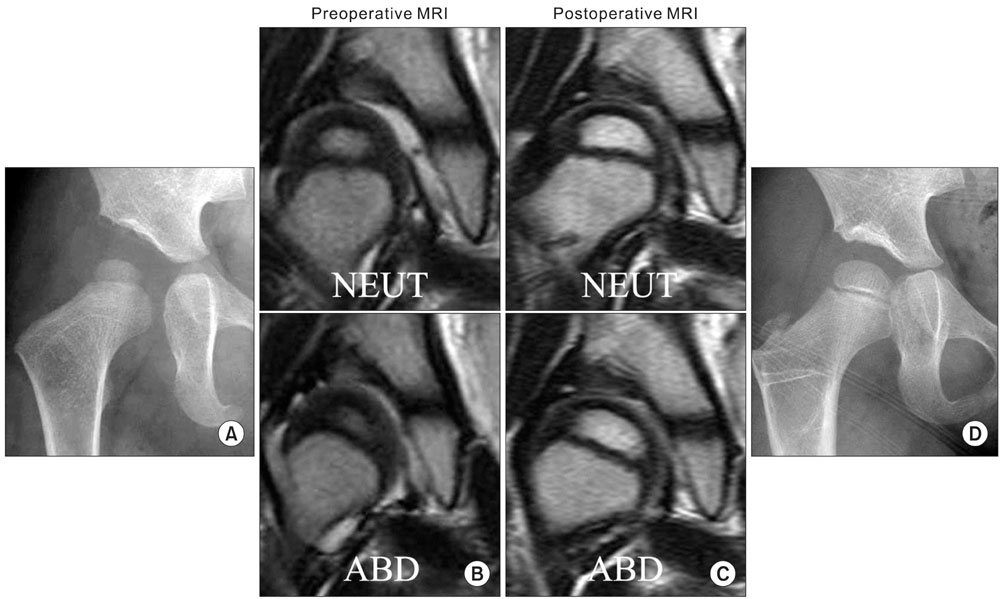
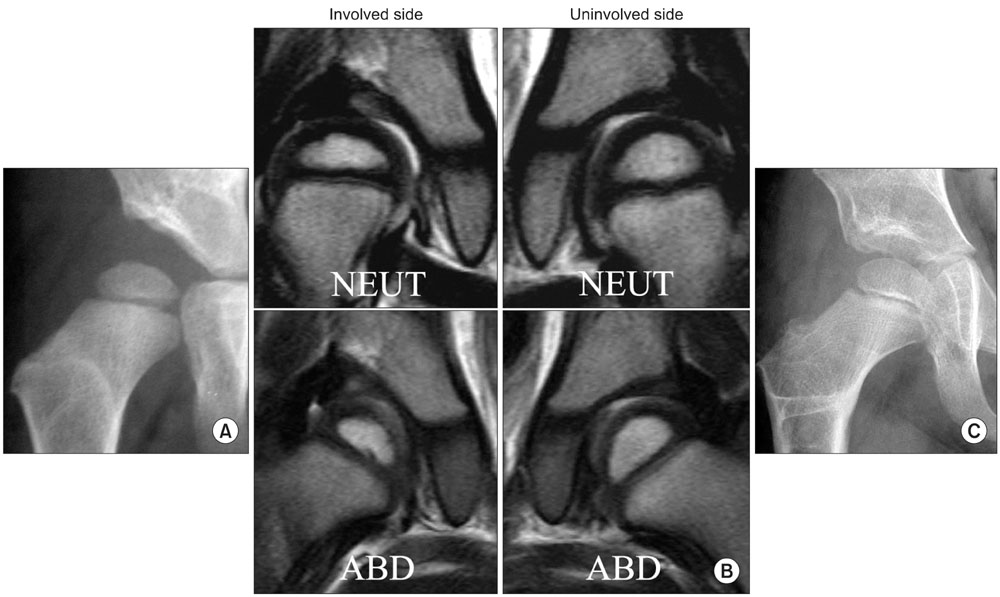
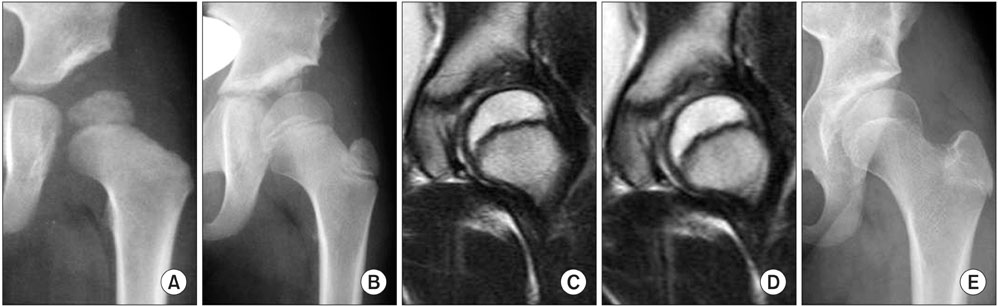
We studied range of motion (ROM)-MRI of 25 patients with unilateral hip dysplasia (mean age at the time of MR imaging, 44.1 months). Each ROM-MRI consisted of a set of bilateral hip scans in the following positions: neutral; abduction; abduction- internal rotation; abduction-internal rotation-flexion; and adduction. Before MR scanning, the 25 patients received the following primary treatments: closed reduction (n = 15; at a mean age of 14.5 months); and open reduction (n = 10; at a mean age of 10.0 months). The following new parameters appear to be useful in treating DDH: 1) the labral angle, the angle the labrum makes with the acetabulum; 2) the uncorrected labral deformity (ULD), the "residual deformity" (deflection of the labrum) when the affected labrum is freed from pressure in abduction; and 3) the zone of compressive force (ZCF), the region of the acetabulum through which the body weight acts on the femoral head.
RESULTS
A concentrically-reduced hip is one in which the labrum points downward in the neutral position, at the same angle as that of the normal side; and in which the ZCF is zone 3, the inner acetabular zone as defined herein. The ULD and the ZCF may be determined precisely as we have done, or the physician may simply observe the changes in the orientation of the labrum and compare the changes qualitatively to the unaffected side, and likewise for the medial joint space.
CONCLUSIONS
Detailed analysis of the labrum as permitted by ROM-MRI, together with acetabular index and other parameters measured from radiographs, provides important information for physicians treating childhood hip dysplasia.
Keyword
MeSH Terms
Figure
Reference
-
1. Mladenov K, Dora C, Wicart P, Seringe R. Natural history of hips with borderline acetabular index and acetabular dysplasia in infants. J Pediatr Orthop. 2002. 22(5):607–612.
Article2. Pirpiris M, Payman KR, Otsuka NY. The assessment of acetabular index: is there still a place for plain radiography? J Pediatr Orthop. 2006. 26(3):310–315.3. Tasnavites A, Murray DW, Benson MK. Improvement in acetabular index after reduction of hips with developmental dysplasia. J Bone Joint Surg Br. 1993. 75(5):755–759.
Article4. Tonnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976. (119):39–47.5. Wiberg G. Studies on dysplastic acetabular and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Parts HV. Acta Chir Scand Suppl. 1939. 83:Suppl 58. 7–38.6. Chen IH, Kuo KN, Lubicky JP. Prognosticating factors in acetabular development following reduction of developmental dysplasia of the hip. J Pediatr Orthop. 1994. 14(1):3–8.
Article7. Smith WS, Badgley CE, Orwig JB, Harper JM. Correlation of postreduction roentgenograms and thirty-one-year follow-up in congenital dislocation of the hip. J Bone Joint Surg Am. 1968. 50(6):1081–1098.
Article8. Wagner H. Weil UH, editor. Transplantation of the greater trochanter. Progress in orthopaedic surgery. Vol 2. Acetabular dyspasia and skeletal dysplasia in childhood. 1978. Heidelberga: Springer;99–102.9. Kim HT, Kim JI, Yoo CI. Acetabular development after closed reduction of developmental dislocation of the hip. J Pediatr Orthop. 2000. 20(6):701–708.
Article10. Ferguson SJ, Bryant JT, Ito K. The material properties of the bovine acetabular labrum. J Orthop Res. 2001. 19(5):887–896.
Article11. Horii M, Kubo T, Inoue S, Kim WC. Coverage of the femoral head by the acetabular labrum in dysplastic hips: quantitative analysis with radial MR imaging. Acta Orthop Scand. 2003. 74(3):287–292.
Article12. Kim YH. Acetabular dysplasia and osteoarthritis developed by an eversion of the acetabular labrum. Clin Orthop Relat Res. 1987. (215):289–295.
Article13. Miozzari HH, Clark JM, Jacob HA, von Rechenberg B, Notzli HP. Effects of removal of the acetabular labrum in a sheep hip model. Osteoarthritis Cartilage. 2004. 12(5):419–430.
Article14. Nishii T, Tanaka H, Sugano N, Miki H, Takao M, Yoshikawa H. Disorders of acetabular labrum and articular cartilage in hip dysplasia: evaluation using isotropic high-resolutional CT arthrography with sequential radial reformation. Osteoarthritis Cartilage. 2007. 15(3):251–257.
Article15. Petersen W, Petersen F, Tillmann B. Structure and vascularization of the acetabular labrum with regard to the pathogenesis and healing of labral lesions. Arch Orthop Trauma Surg. 2003. 123(6):283–288.
Article16. Ponseti IV. Morphology of the acetabulum in congenital dislocation of the hip: gross, histological and roentgenographic studies. J Bone Joint Surg Am. 1978. 60(5):586–599.
Article17. Ueshima K, Takahashi KA, Fujioka M, et al. Relationship between acetabular labrum evaluation by using radial magnetic resonance imaging and progressive joint space narrowing in mild hip dysplasia. Magn Reson Imaging. 2006. 24(5):645–650.
Article18. Pauwels F. Schatzker J, editor. Biomechanical principles of varus/valgus intertrochanteric osteotomy (Pauwels I and II) in the treatment of osteoarthritis of the hip. The intertrochanteric osteotomy. 1984. New York: Springer;3–23.
Article19. Albinana J, Morcuende JA, Weinstein SL. The teardrop in congenital dislocation of the hip diagnosed late: a quantitative study. J Bone Joint Surg Am. 1996. 78(7):1048–1055.
Article20. Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL. Acetabular dysplasia after treatment for developmental dysplasia of the hip: implications for secondary procedures. J Bone Joint Surg Br. 2004. 86(6):876–886.21. Brougham DI, Broughton NS, Cole WG, Menelaus MB. The predictability of acetabular development after closed reduction for congenital dislocation of the hip. J Bone Joint Surg Br. 1988. 70(5):733–736.
Article22. Harris NH, Lloyd-Roberts GC, Gallien R. Acetabular development in congenital dislocation of the hip: with special reference to the indications for acetabuloplasty and pelvic or femoral realignment osteotomy. J Bone Joint Surg Br. 1975. 57(1):46–52.23. Harris NH. Acetabular growth potential in congenital dislocation of the hip and some factors upon which it may depend. Clin Orthop Relat Res. 1976. (119):99–106.
Article24. Lindstrom JR, Ponseti IV, Wenger DR. Acetabular development after reduction in congenital dislocation of the hip. J Bone Joint Surg Am. 1979. 61(1):112–118.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric Hip Disease (I): Diagnosis and Treatment of Developmental Dysplasia of the Hip
- Pediatric Hip Disease (II): Developmental Dysplasia of the Hip – Treatment of Residual Dysplasia
- Dynamic ultrasonography in developmental dysplasia of the hip treated with Pavlik harness
- Radiographic parameters of acetabulum for dysplasia in Korean adults
- Correlations between ultrasonographic and subsequent radiographic findings of developmental dysplasia of the hips