Yonsei Med J.
2005 Jun;46(3):425-430. 10.3349/ymj.2005.46.3.425.
An Unusual Case of Spontaneous Remission of Hodgkin's Disease after a Single Cycle of COPP-ABV Chemotherapy Followed by Infectious Complications
- Affiliations
-
- 1Division of Hemato-oncology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. medi@yumc.yonsei.ac.kr
- 2Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1734079
- DOI: http://doi.org/10.3349/ymj.2005.46.3.425
Abstract
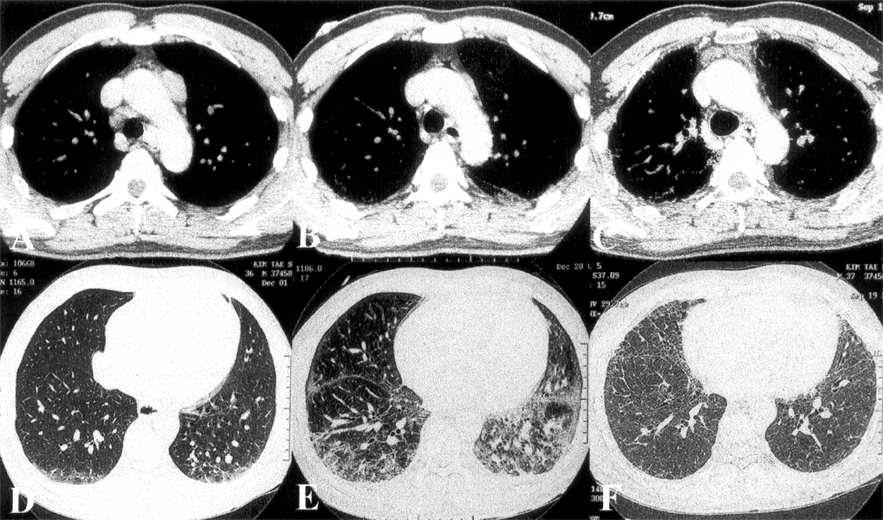
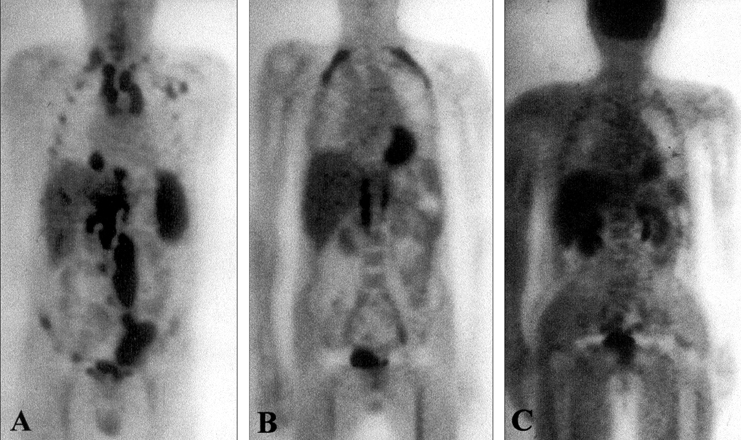
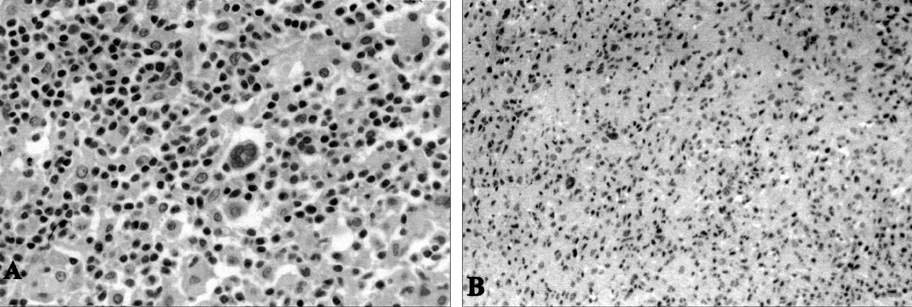
- Advanced Hodgkin's disease is usually treated with six or more cycles of combination chemotherapy. Spontaneous regression of the cancer is very rarely reported in patients with Hodgkin's disease. We present an unusual case of a patient with Hodgkin's disease who experienced complete remission with a single cycle of chemotherapy, followed by pneumonia. The case was a 36-year-old man diagnosed with stage IVB mixed cellularity Hodgkin's disease in November 2000. After treatment with one cycle of COPP-ABV (cyclophosphamide, vincristine, procarbazine, prednisone, doxorubicin, bleomycin, and vinblastine) chemotherapy without bleomycin, the patient developed interstitial pneumonia and was cared in the intensive care unit (ICU) for two months. Follow-up chest computerized tomography (CT), performed during the course of ICU care, revealed markedly improved mediastinal lymphomatous lesions. Furthermore, follow-up whole body CT and 18-fluorodeoxyglucose positron emission tomography showed complete disappearance of the lymphomatous lesions. Four years later, the patient is well and without relapse. This report is followed by a short review of the literature on spontaneous regression of Hodgkin's disease. To the best of our knowledge, this is the first case report of spontaneous remission of Hodgkin's disease in Korea.
MeSH Terms
-
Adult
Antineoplastic Combined Chemotherapy Protocols/*administration & dosage
Bleomycin/*administration & dosage
Cyclophosphamide/*administration & dosage
Doxorubicin/*administration & dosage
Hodgkin Disease/*complications/*drug therapy
Humans
Male
Pneumonia/*complications
Prednisone/*administration & dosage
Procarbazine/*administration & dosage
Remission, Spontaneous
Vinblastine/*administration & dosage
Vincristine/*administration & dosage
Figure
Reference
-
1. MacMahon B. Epidemiology of Hodgkin's disease. Cancer Res. 1966. 26:1189–1200.2. Papac RJ. Spontaneous regression of cancer. Cancer Treat Rev. 1996. 22:395–423.3. Challis GB, Stam HJ. The spontaneous regression of cancer. A review of cases from 1900 to 1987. Acta Oncol. 1990. 5:545–549.4. Gattiker HH, Wiltshaw E, Galton DA. Spontaneous regression in non-Hodgkin's lymphoma. Cancer. 1980. 45:2627–2632.5. Horning SJ, Rosenberg SA. The natural history of initially untreated low-grade non-Hodgkin's lymphomas. N Engl J Med. 1984. 311:1471–1475.6. Krikorian JG, Portlock CS, Cooney P, Rosenberg SA. Spontaneous regression of non-Hodgkin's lymphoma: a report of nine cases. Cancer. 1980. 46:2093–2099.7. Poppema S, Postma L, Brinker M, de Jong B. Spontaneous regression of a small non-cleaved cell malignant lymphoma (non-Burkitt's lymphoblastic lymphoma). Morphologic, immunohistological, and immunoglobulin gene analysis. Cancer. 1988. 62:791–794.8. Kumamoto M, Nakamine H, Hara T, Yokoya Y, Kawai J, Ito H, et al. Spontaneous complete regression of high grade non-Hodgkin's lymphoma. Morphologic, immunohistochemical, and gene amplification analyses. Cancer. 1994. 74:3023–3028.9. Heibel H, Knodgen R, Bredenfeld H, Wickenhauser C, Scheer M, Zoller JE. Complete spontaneous remission of an aggressive non-Hodgkin's lymphoma with primary manifestation in the oral cavity. Leuk Lymphoma. 2004. 45:171–174.10. Weinshel EL, Peterson BA. Hodgkin's disease. CA Cancer J Clin. 1993. 43:327–346.11. Mangel J, Barth D, Berinstein NL, Imrie KR. Spontaneous regression of Hodgkin's disease: two case reports and a review of the literature. Hematology. 2003. 8:191–196.12. Williams MV. Spontaneous regression of cutaneous Hodgkin's disease. Br Med J. 1980. 280:903.13. Szur L, Harrison CV, Levene GM, Samman PD. Primary cutaneous Hodgkin's disease. Lancet. 1970. 1:1016–1020.14. Taqi AM, Abdurrahman MB, Yakubu AM, Fleming AF. Regression of Hodgkin's disease after measles. Lancet. 1981. 1:1112.15. Zygiert Z. Hodgkin's disease: remissions after measles. Lancet. 1971. 1:593.16. Parekh S, Koduri PR. Spontaneous regression of HIV-associated Hodgkin's disease. Am J Hematol. 2003. 72:153–154.17. Drobyski WR, Qazi R. Spontaneous regression in non-Hodgkin's lymphoma: clinical and pathogenetic considerations. Am J Hematol. 1989. 31:138–141.18. Ono K, Kikuchi M, Funai N, Matsuzaki M, Shimamoto Y. Natural killing activity in patients with spontaneous regression of malignant lymphoma. J Clin Immunol. 1996. 16:334–339.19. Loren AW, Porter DL, Stadtmauer EA, Tsai DE. Post-transplant lymphoproliferative disorder: a review. Bone Marrow Transplant. 2003. 31:145–155.20. Ryu HJ, Hahn JS, Kim YS, Park K, Yang WI, Lee JD. Complete resolution of posttransplant lymphoproliferative disorder (diffuse large B-cell lymphoma) with reduction of immunosuppressive therapy. Yonsei Med J. 2004. 45:527–532.21. Nauts H. The treatment of malignant tumors by bacterial toxins, as developed by the late William B. and Coley M.D. reviewed in the light of modern research. Cancer Res. 1946. 6:205–216.22. Balkwill FR, Naylor MS, Malik S. Tumour necrosis factor as an anticancer agent. Eur J Cancer. 1990. 26:641–644.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- COPP/ABV Hybrid Chemotherapy in Pateints with Hodgkin's Disease
- A Case of Malignant Histiocytosis : Complete Remission with COPP Combination Chemotherapy
- Combination Chemotherapy to Hodgkin's Disease in a Pregnant Patient
- Simultaneous Occurrence of Hodgkin's Disease and Multiple Myeloma
- Evidence that Amphotericin B Mediates Reactivation of Latent Epstein-Barr Virus in Hodgkin's Lymphoma Allowing Cytotoxicity by Acyclovir