Korean J Gastroenterol.
2014 Mar;63(3):171-175. 10.4166/kjg.2014.63.3.171.
Acute Obstructive Cholangitis Complicated by Tumor Migration after Transarterial Chemoembolization: A Case Report and Literature Review
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea. portalvein@naver.com
- KMID: 1730928
- DOI: http://doi.org/10.4166/kjg.2014.63.3.171
Abstract
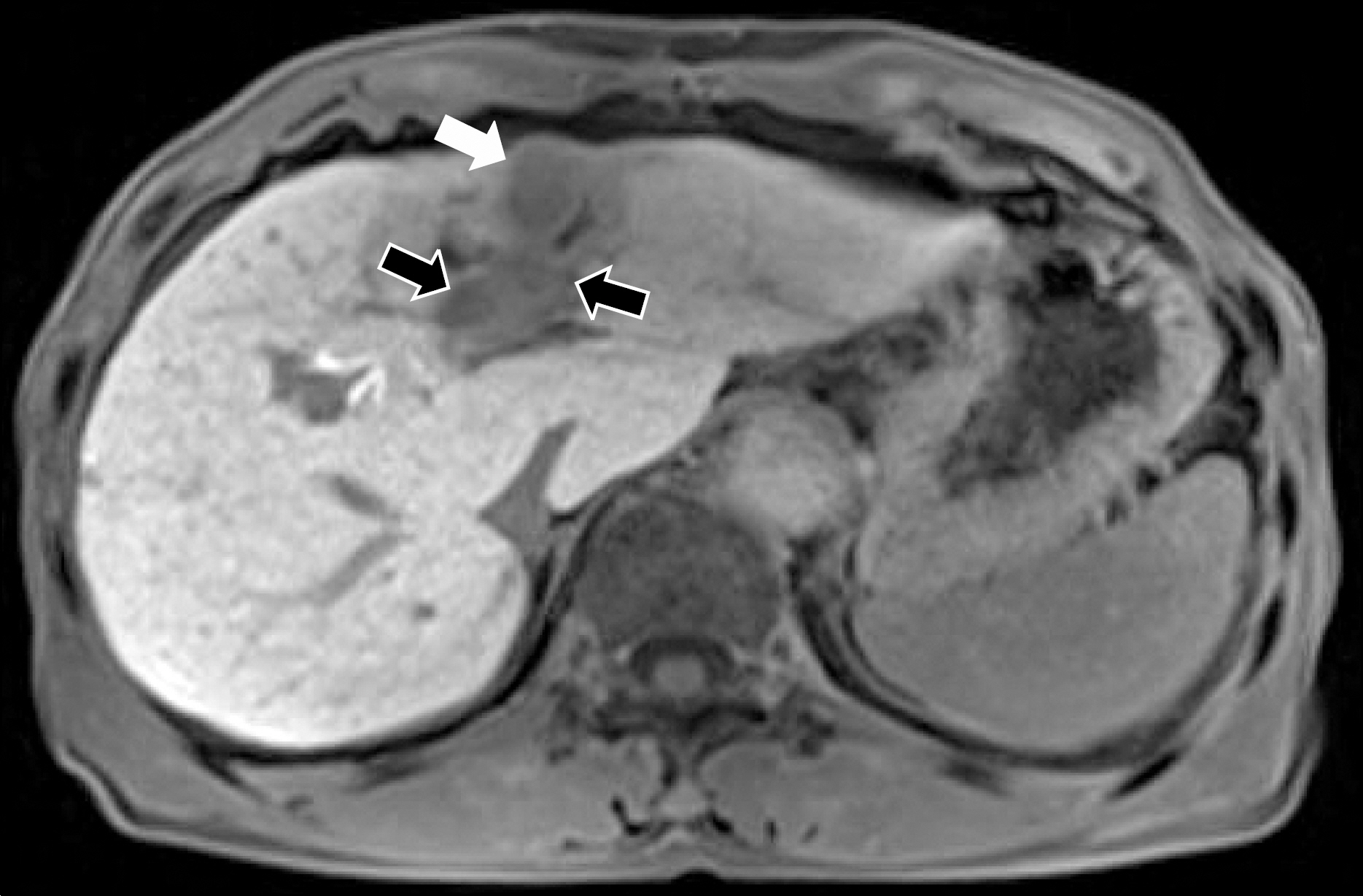
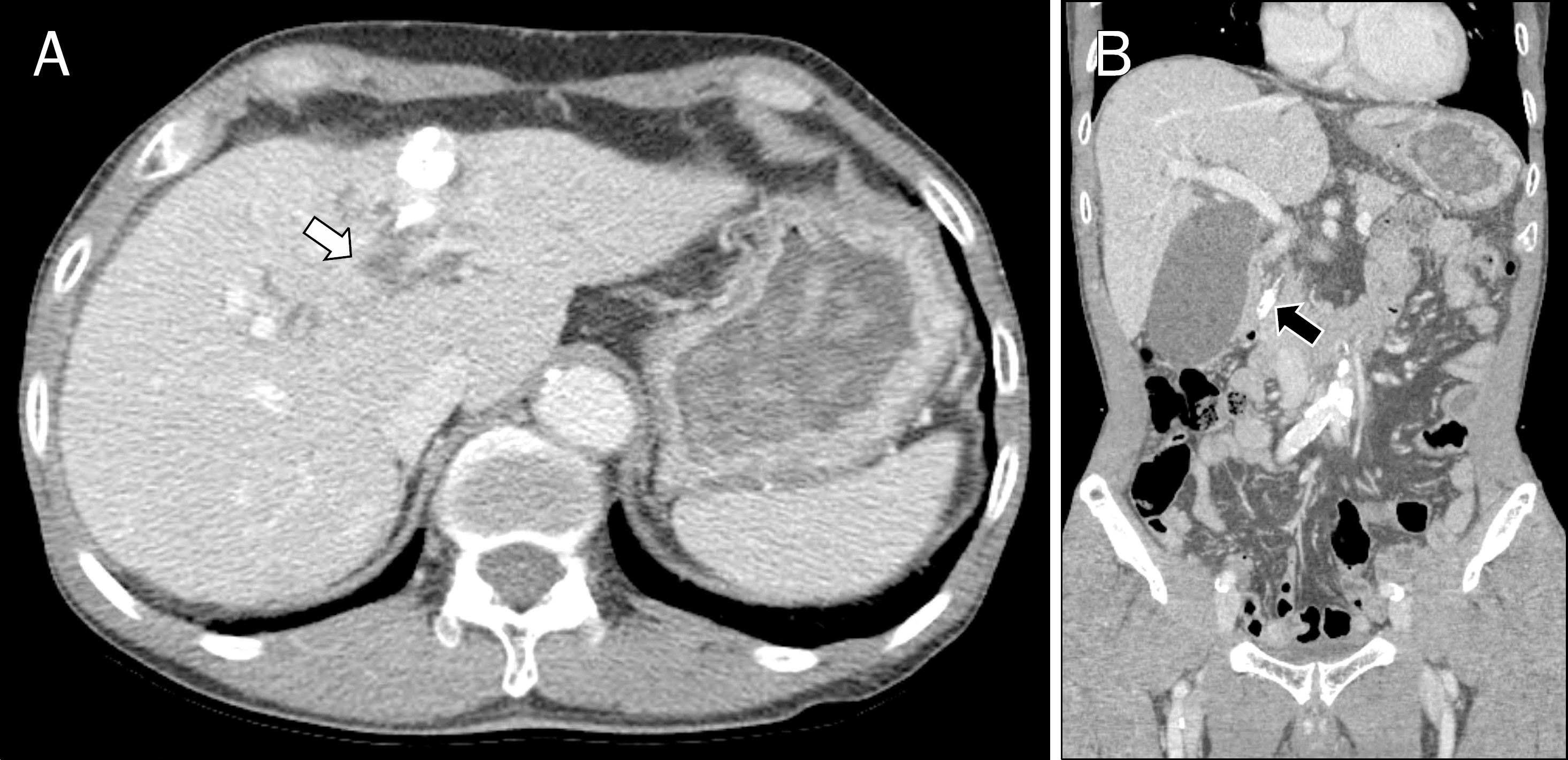
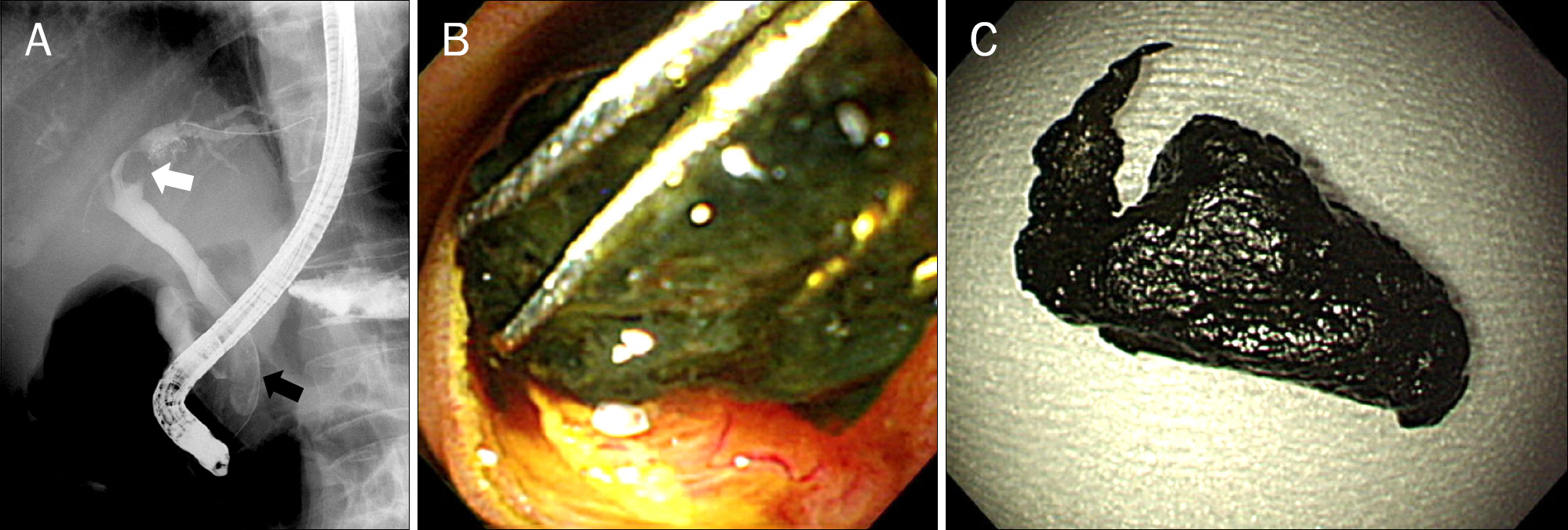
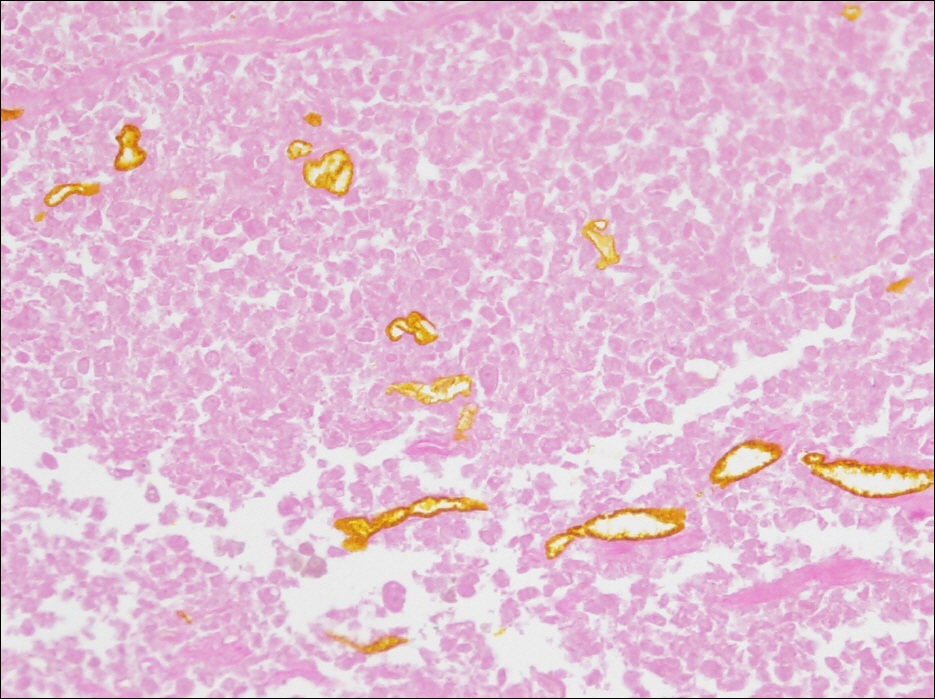
- Intraductal tumor invasion of hepatocellular carcinoma (HCC) is considered rare. Transarterial chemoembolization (TACE) is effective for tumor thrombus of HCC in the bile duct. However, a few cases of obstructive jaundice caused by migration of a tumor fragment after TACE have recently been reported. The aim of this study was to identify factors that affect tumor migration after TACE. At this writing, a review of the medical literature disclosed seven reported cases of biliary obstruction caused by migration of a necrotic tumor cast after TACE. We, herein, report on an additional case of acute obstructive cholangitis complicated by migration of a necrotic tumor cast after TACE for intrabile duct invasion of HCC, in a 71-year-old man. The tumor cast in the common bile duct was removed successfully using a basket during ERCP and was pathologically confirmed to be a completely necrotic fragment of HCC. The patient's symptoms showed dramatic improvement. In summary, physicians should be aware of acute obstructive cholangitis complicated by tumor migration in a patient undergoing TACE. We suggest that an intrabile duct invasion would be a major predisposing factor of tumor migration after TACE and drainage procedures such as ERCP or percutaneous transbiliary drainage could be effective treatment modalities in these patients.
MeSH Terms
-
Acute Disease
Aged
Antineoplastic Agents/administration & dosage
Bile Ducts, Intrahepatic/pathology
Carcinoma, Hepatocellular/*diagnosis/pathology/therapy
Chemoembolization, Therapeutic/adverse effects
Cholangiopancreatography, Endoscopic Retrograde
Cholangitis/*etiology
Humans
Jaundice, Obstructive/etiology
Liver Neoplasms/*diagnosis/pathology/therapy
Male
Necrosis/pathology
Sphincterotomy, Endoscopic
Thrombosis/etiology
Tomography, X-Ray Computed
Antineoplastic Agents
Figure
Reference
-
References
1. Clark TW. Complications of hepatic chemoembolization. Semin Intervent Radiol. 2006; 23:119–125.
Article2. Xia J, Ren Z, Ye S, et al. Study of severe and rare complications of transarterial chemoembolization (TACE) for liver cancer. Eur J Radiol. 2006; 59:407–412.
Article3. Ikeda M, Maeda S, Shibata J, et al. Transcatheter arterial chemotherapy with and without embolization in patients with hepatocellular carcinoma. Oncology. 2004; 66:24–31.
Article4. Jeon SH, Park KS, Kim YH, et al. Incidence and risk factors of acute hepatic failure after transcatheter arterial chemoembolization for hepatocellular carcinoma. Korean J Gastroenterol. 2007; 50:176–182.5. Spahr L, Frossard JL, Felley C, Brundler MA, Majno PE, Hadengue A. Biliary migration of hepatocellular carcinoma fragment after transcatheter arterial chemoembolization therapy. Eur J Gastroenterol Hepatol. 2000; 12:243–244.
Article6. Hiraki T, Sakurai J, Gobara H, et al. Sloughing of intraductal tumor thrombus of hepatocellular carcinoma after transcatheter chemoembolization causing obstructive jaundice and acute pancreatitis. J Vasc Interv Radiol. 2006; 17:583–585.
Article7. Choi KH, Cho YK, An JK, Woo JJ, Kim HS, Choi YS. Acute obstructive cholangitis after transarterial chemoembolization: the effect of percutaneous transhepatic removal of tumor fragment. Korean J Radiol. 2009; 10:197–201.
Article8. Choi H, Kim SB, Shin KC, et al. Common bile duct obstruction caused by tumor thrombus after transarterial chemoembolization in a hepatocellular carcinoma patient. Korean J Gastrointest Endosc. 2009; 38:299–302.9. Okuda M, Miyayama S, Yamashiro M, et al. Sloughing of intraductal tumor thrombus of hepatocellular carcinoma after transcatheter arterial chemoembolization. Cardiovasc Intervent Radiol. 2010; 33:619–623.
Article10. Chen MF, Jan YY, Jeng LB, Hwang TL, Wang CS, Chen SC. Obstructive jaundice secondary to ruptured hepatocellular carcinoma into the common bile duct. Surgical experiences of 20 cases. Cancer. 1994; 73:1335–1340.
Article11. Huang JF, Wang LY, Lin ZY, et al. Incidence and clinical outcome of icteric type hepatocellular carcinoma. J Gastroenterol Hepatol. 2002; 17:190–195.
Article12. Ikenaga N, Chijiiwa K, Otani K, Ohuchida J, Uchiyama S, Kondo K. Clinicopathologic characteristics of hepatocellular carcinoma with bile duct invasion. J Gastrointest Surg. 2009; 13:492–497.
Article13. Kojiro M, Kawabata K, Kawano Y, Shirai F, Takemoto N, Nakashima T. Hepatocellular carcinoma presenting as intrabile duct tumor growth: a clinicopathologic study of 24 cases. Cancer. 1982; 49:2144–2147.
Article14. Lin TY, Chen KM, Chen YR, Lin WS, Wang TH, Sung JL. Icteric type hepatoma. Med Chir Dig. 1975; 4:267–270.15. Qin LX, Tang ZY. Hepatocellular carcinoma with obstructive jaundice: diagnosis, treatment and prognosis. World J Gastroenterol. 2003; 9:385–391.
Article16. Wang HJ, Kim JH, Kim JH, Kim WH, Kim MW. Hepatocellular carcinoma with tumor thrombi in the bile duct. Hepatogastroenterology. 1999; 46:2495–2499.17. Takagi H, Yamada S, Abe T, et al. A case report of transcatheter arterial embolization of cholestatic type of hepatoma. Gastroenterol Jpn. 1989; 24:315–319.
Article18. Martin JA, Slivka A, Rabinovitz M, Carr BI, Wilson J, Silverman WB. ERCP and stent therapy for progressive jaundice in hepatocellular carcinoma: which patients benefit, which patients don't? Dig Dis Sci. 1999; 44:1298–1302.19. Cho HC, Lee JK, Lee KH, et al. Are endoscopic or percutaneous biliary drainage effective for obstructive jaundice caused by hepatocellular carcinoma? Eur J Gastroenterol Hepatol. 2011; 23:224–231.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraductal migration of necrotic hepatocellular carcinoma: A possible cause of obstructive cholangitis after chemoembolization
- Acute Obstructive Cholangitis after Transarterial Chemoembolization: the Effect of Percutaneous Transhepatic Removal of Tumor Fragment
- Complications Related to Transarterial Treatment of Hepatocellular Carcinoma: A Comprehensive Review
- Common Bile Duct Obstruction Caused by Tumor Thrombus after Trans-arterial Chemoembolization in a Hepatocellular Carcinoma Patient
- Rare Case of Pyogenic Brain Abscess after Transarterial Chemoembolization in a Patient with Hepatocellular Carcinoma: Case Report and Literature Review