Tuberc Respir Dis.
2010 Mar;68(3):140-145. 10.4046/trd.2010.68.3.140.
Acute Pulmonary Embolism: Clinical Characteristics and Outcomes in a University Teaching Hospital
- Affiliations
-
- 1Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea. wichoi@dsmc.or.kr
- 2Department of Diagnostic Radiology, Keimyung University School of Medicine, Daegu, Korea.
- 3Department of Thoracic Surgery, Keimyung University School of Medicine, Daegu, Korea.
- KMID: 1728958
- DOI: http://doi.org/10.4046/trd.2010.68.3.140
Abstract
- BACKGROUND
Pulmonary embolism (PE) is a common clinical problem in the West that is associated with substantial morbidity and mortality. The diagnostic modality has been changed since 2001. This study retrospectively reviewed the PE mortality with the aim of identifying the risk factors associated with mortality since the multidetector computed tomography (MDCT) was introduced.
METHODS
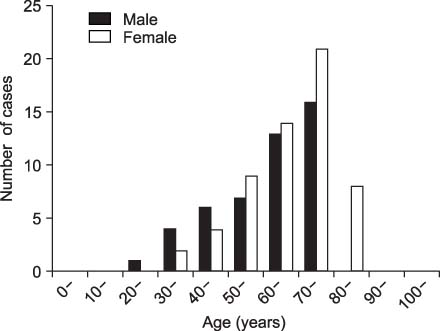
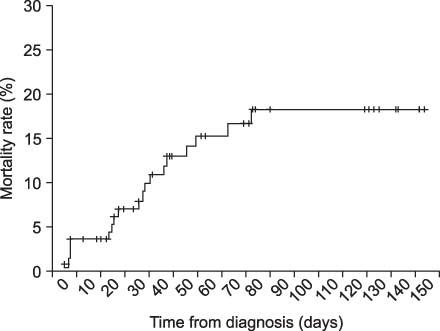
We analyzed 105 patients with acute PE proven by multidetector CT or ventilation perfusion scan. The primary outcome measure was the all-cause mortality at 3 months. The prognostic effect of the baseline factors on survival was assessed by multivariate analysis.
RESULTS
The main risk factors were prolonged immobilization, stroke, cancer and obesity. Forty nine percent of patients had 3 or more risk factors. The overall mortality at 3 months was 18.1%. Multivariate analysis revealed low diastolic blood pressure and the existence of cancer to be independent factors significantly associated with mortality. Forty two PE patients were examined for the coagulation inhibitors. Four of these patients had a protein C deficiency (9.5%), and 11 had a protein S deficiency (26%).
CONCLUSION
PE is an important clinical problem with a high mortality rate. Close monitoring may be necessary in patients with the risk factors.
MeSH Terms
-
Blood Pressure
Hospitals, Teaching
Humans
Immobilization
Multidetector Computed Tomography
Multivariate Analysis
Obesity
Outcome Assessment (Health Care)
Perfusion
Prognosis
Protein C Deficiency
Protein S Deficiency
Pulmonary Embolism
Retrospective Studies
Risk Factors
Stroke
Thrombophilia
Venous Thrombosis
Ventilation
Figure
Reference
-
1. Park YS, Ha JW, Kwon KH, Jang YS, Chung NS, Shim WH, et al. Clinical characteristics and predictors of in-hospital mortality for patients with acute major pulmonary embolism. Korean J Med. 2000. 58:293–300.2. Lee GL, Kim JY, Park JS, Yoo CG, Kim YW, Shim YS, et al. Clinical study of the patients, in whom pulmonary embolism was suspected by lung perfusion scan. Tuberc Respir Dis. 1997. 44:889–898.3. Lee SS, Lim CM, Song KS, Sung KB, Koh YS, Lee SD, et al. The value of spiral computed tomography in the diagnosis of pulmonary embolism. Korean J Med. 1997. 53:787–794.4. Lee S, Jeong H, In K, Yoo S, Kim S, Kim J, et al. Clinical characteristics of acute pulmonary thromboembolism in Korea. Int J Cardiol. 2006. 108:84–88.5. Stein PD, Fowler SE, Goodman LR, Gottschalk A, Hales CA, Hull RD, et al. Multidetector computed tomography for acute pulmonary embolism. N Engl J Med. 2006. 354:2317–2327.6. Anderson DR, Kahn SR, Rodger MA, Kovacs MJ, Morris T, Hirsch A, et al. Computed tomographic pulmonary angiography vs ventilation-perfusion lung scanning in patients with suspected pulmonary embolism: a randomized controlled trial. JAMA. 2007. 298:2743–2753.7. DeMonaco NA, Dang Q, Kapoor WN, Ragni MV. Pulmonary embolism incidence is increasing with use of spiral computed tomography. Am J Med. 2008. 121:611–617.8. British Thoracic Society Standards of Care Committee Pulmonary Embolism Guideline Development Group. British Thoracic Society guidelines for the management of suspected acute pulmonary embolism. Thorax. 2003. 58:470–483.9. Wells PS, Anderson DR, Rodger M, Stiell I, Dreyer JF, Barnes D, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann Intern Med. 2001. 135:98–107.10. Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet. 1999. 353:1386–1389.11. Jang MJ, Choi WI, Bang SM, Lee T, Kim YK, Ageno W, et al. Metabolic syndrome is associated with venous thromboembolism in the Korean population. Arterioscler Thromb Vasc Biol. 2009. 29:311–315.12. Lee JW, Cha SI, Jung CY, Choi WI, Jeon KN, Yoo SS, et al. Clinical course of pulmonary embolism in lung cancer patients. Respiration. 2009. 78:42–48.13. Sorensen HT, Mellemkjaer L, Olsen JH, Baron JA. Prognosis of cancers associated with venous thromboembolism. N Engl J Med. 2000. 343:1846–1850.14. Seligsohn U, Lubetsky A. Genetic susceptibility to venous thrombosis. N Engl J Med. 2001. 344:1222–1231.15. Lee A, Song KS. Screening results of AT III, protein C and S, and APC resistance for diagnosis of inheritied thrombophilia. Korean J Thromb Hemost. 1995. 2:147–153.16. Kim HK, Na JO, Ahn JJ, Park YB, Lim JM, Hong SB, et al. Comparison of clinical features between idiopathic pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Tuberc Respir Dis. 2005. 59:170–178.17. Suehisa E, Nomura T, Kawasaki T, Kanakura Y. Frequency of natural coagulation inhibitor (antithrombin III, protein C and protein S) deficiencies in Japanese patients with spontaneous deep vein thrombosis. Blood Coagul Fibrinolysis. 2001. 12:95–99.18. Tabernero MD, Tomas JF, Alberca I, Orfao A, Lopez Borrasca A, Vicente V. Incidence and clinical characteristics of hereditary disorders associated with venous thrombosis. Am J Hematol. 1991. 36:249–254.19. De Stefano V, Finazzi G, Mannucci PM. Inherited thrombophilia: pathogenesis, clinical syndromes, and management. Blood. 1996. 87:3531–3544.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Impending Paradoxical Embolus in a Patient with Acute Pulmonary Embolism
- Acute Pulmonary Embolism
- Open Embolectomy of an Acute Pulmonary Artery Embolism after Pulmonary Lobectomy
- Acute Massive Pulmonary Thromboembolism Occupying both Whole Pulmonary Arteries
- A Case of Acute Massive Pulmonary Emoblism Complicated by Hypercapnia