Korean J Radiol.
2013 Aug;14(4):559-567. 10.3348/kjr.2013.14.4.559.
Sonoelastography in Distinguishing Benign from Malignant Complex Breast Mass and Making the Decision to Biopsy
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, Seoul National University Hospital, and Institute of Radiation Medicine, Seoul 110-744, Korea. river7774@gmail.com
- 2Department of Radiology, Konkuk University School of Medicine, Konkuk University Medical Center, Seoul 143-729, Korea.
- 3Department of Radiology, Seoul National University Bundang Hospital, Seongnam 463-707, Korea.
- KMID: 1715759
- DOI: http://doi.org/10.3348/kjr.2013.14.4.559
Abstract
OBJECTIVE
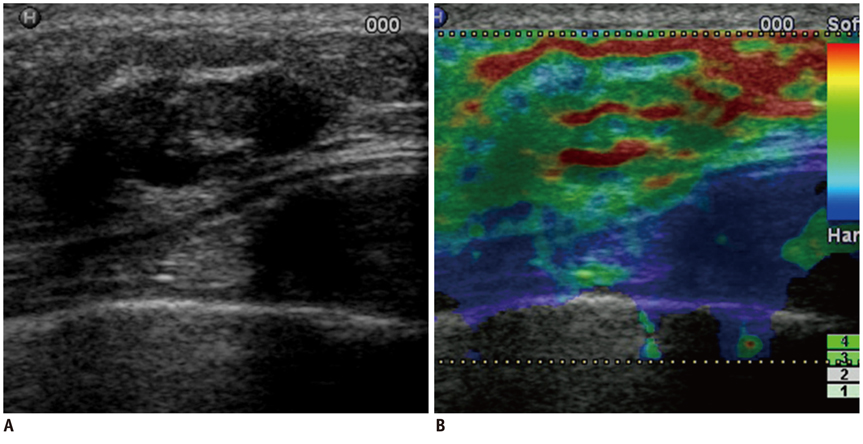
To evaluate the additional effect of sonoelastography on the radiologist's ability for distinguishing benign from malignant complex breast masses and to decide whether to perform biopsy by B-mode US.
MATERIALS AND METHODS
One hundred eighteen complex breast masses (15 malignant lesions, 103 benign lesions) were included. Five blinded readers independently assessed the likelihood of the malignancy score from 1 to 5 for two data sets (B-mode ultrasound alone and B-mode ultrasound with sonoelastography). Elasticity scores were categorized as 0, 1, or 2 based on the degree and distribution of strain of the echogenic component within complex masses. The readers were asked to downgrade the likelihood of the malignancy score when an elasticity score of 0 was assigned and to upgrade the likelihood of the malignancy score when an elasticity score of 2 was assigned. The likelihood of the malignancy score was maintained as it was for the lesions with an elasticity score of 1. The Az values, sensitivities, and specificities were compared.
RESULTS
The Az value of B-mode ultrasound with sonoelastography (mean, 0.863) was greater than that of B-mode ultrasound alone (mean, 0.731; p = 0.001-0.007) for all authors. The specificity of B-mode ultrasound with sonoelastography (mean, 37.1%) was greater than that of B-mode ultrasound alone (mean, 3.8%; p < 0.001) for all readers. The addition of sonoelastography led to changes in decisions. A mean of 33.6% of benign masses were recommended for follow-up instead of biopsy.
CONCLUSION
For complex breast masses, sonoelastography allows increase in both the accuracy in distinguishing benign from malignant lesions and the specificity in deciding whether to perform biopsy.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Annual Trends in Ultrasonography-Guided 14-Gauge Core Needle Biopsy for Breast Lesions
Inha Jung, Kyunghwa Han, Min Jung Kim, Hee Jung Moon, Jung Hyun Yoon, Vivian Youngjean Park, Eun-Kyung Kim
Korean J Radiol. 2020;21(3):259-267. doi: 10.3348/kjr.2019.0695.
Reference
-
1. Gordon PB, Goldenberg SL. Malignant breast masses detected only by ultrasound. A retrospective review. Cancer. 1995; 76:626–630.2. Buchberger W, DeKoekkoek-Doll P, Springer P, Obrist P, Dünser M. Incidental findings on sonography of the breast: clinical significance and diagnostic workup. AJR Am J Roentgenol. 1999; 173:921–927.3. Buchberger W, Niehoff A, Obrist P, DeKoekkoek-Doll P, Dünser M. Clinically and mammographically occult breast lesions: detection and classification with high-resolution sonography. Semin Ultrasound CT MR. 2000; 21:325–336.4. Kaplan SS. Clinical utility of bilateral whole-breast US in the evaluation of women with dense breast tissue. Radiology. 2001; 221:641–649.5. Kolb TM, Lichy J, Newhouse JH. Comparison of the performance of screening mammography, physical examination, and breast US and evaluation of factors that influence them: an analysis of 27,825 patient evaluations. Radiology. 2002; 225:165–175.6. Leconte I, Feger C, Galant C, Berlière M, Berg BV, D'Hoore W, et al. Mammography and subsequent whole-breast sonography of nonpalpable breast cancers: the importance of radiologic breast density. AJR Am J Roentgenol. 2003; 180:1675–1679.7. Crystal P, Strano SD, Shcharynski S, Koretz MJ. Using sonography to screen women with mammographically dense breasts. AJR Am J Roentgenol. 2003; 181:177–182.8. Hooley RJ, Greenberg KL, Stackhouse RM, Geisel JL, Butler RS, Philpotts LE. Screening US in patients with mammographically dense breasts: initial experience with Connecticut Public Act 09-41. Radiology. 2012; 265:59–69.9. Berg WA, Blume JD, Cormack JB, Mendelson EB, Lehrer D, Böhm-Vélez M, et al. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA. 2008; 299:2151–2163.10. Berg WA, Sechtin AG, Marques H, Zhang Z. Cystic breast masses and the ACRIN 6666 experience. Radiol Clin North Am. 2010; 48:931–987.11. American College of Radiology. Breast imaging reporting and data system-ultrasound. American College of Radiology. Breast imaging reporting and data system. 4th ed. Reston, VA: American College of Radiology;2003.12. Omori LM, Hisa N, Ohkuma K, Fujikura Y, Hiramatsu K, Enomoto I, et al. Breast masses with mixed cystic-solid sonographic appearance. J Clin Ultrasound. 1993; 21:489–495.13. Berg WA, Campassi CI, Ioffe OB. Cystic lesions of the breast: sonographic-pathologic correlation. Radiology. 2003; 227:183–191.14. Chang YW, Kwon KH, Goo DE, Choi DL, Lee HK, Yang SB. Sonographic differentiation of benign and malignant cystic lesions of the breast. J Ultrasound Med. 2007; 26:47–53.15. Tea MK, Grimm C, Fink-Retter A, Bikas D, Kroiss R, Kubista E, et al. The validity of complex breast cysts after surgery. Am J Surg. 2009; 197:199–202.16. Krouskop TA, Wheeler TM, Kallel F, Garra BS, Hall T. Elastic moduli of breast and prostate tissues under compression. Ultrason Imaging. 1998; 20:260–274.17. Wellman PS, Dalton EP, Krag D, Kern KA, Howe RD. Tactile imaging of breast masses: first clinical report. Arch Surg. 2001; 136:204–208.18. Itoh A, Ueno E, Tohno E, Kamma H, Takahashi H, Shiina T, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006; 239:341–350.19. Raza S, Odulate A, Ong EM, Chikarmane S, Harston CW. Using real-time tissue elastography for breast lesion evaluation: our initial experience. J Ultrasound Med. 2010; 29:551–563.20. Cho N, Moon WK, Park JS, Cha JH, Jang M, Seong MH. Nonpalpable breast masses: evaluation by US elastography. Korean J Radiol. 2008; 9:111–118.21. Cho N, Jang M, Lyou CY, Park JS, Choi HY, Moon WK. Distinguishing benign from malignant masses at breast US: combined US elastography and color doppler US--influence on radiologist accuracy. Radiology. 2012; 262:80–90.22. Yi A, Cho N, Chang JM, Koo HR, La Yun B, Moon WK. Sonoelastography for 1,786 non-palpable breast masses: diagnostic value in the decision to biopsy. Eur Radiol. 2012; 22:1033–1040.23. Tan SM, Teh HS, Mancer JF, Poh WT. Improving B mode ultrasound evaluation of breast lesions with real-time ultrasound elastography--a clinical approach. Breast. 2008; 17:252–257.24. Thomas A, Fischer T, Frey H, Ohlinger R, Grunwald S, Blohmer JU, et al. Real-time elastography--an advanced method of ultrasound: first results in 108 patients with breast lesions. Ultrasound Obstet Gynecol. 2006; 28:335–340.25. Tardivon A, El Khoury C, Thibault F, Wyler A, Barreau B, Neuenschwander S. [Elastography of the breast: a prospective study of 122 lesions]. J Radiol. 2007; 88(5 Pt 1):657–662.26. Zhi H, Ou B, Luo BM, Feng X, Wen YL, Yang HY. Comparison of ultrasound elastography, mammography, and sonography in the diagnosis of solid breast lesions. J Ultrasound Med. 2007; 26:807–815.27. Booi RC, Carson PL, O'Donnell M, Roubidoux MA, Hall AL, Rubin JM. Characterization of cysts using differential correlation coefficient values from two dimensional breast elastography: preliminary study. Ultrasound Med Biol. 2008; 34:12–21.28. Cho N, Moon WK, Chang JM, Kim SJ, Lyou CY, Choi HY. Aliasing artifact depicted on ultrasound (US)-elastography for breast cystic lesions mimicking solid masses. Acta Radiol. 2011; 52:3–7.29. Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull. 1971; 76:378–382.30. Berg WA, Blume JD, Cormack JB, Mendelson EB. Operator dependence of physician-performed whole-breast US: lesion detection and characterization. Radiology. 2006; 241:355–365.31. Warren RM, Pointon L, Thompson D, Hoff R, Gilbert FJ, Padhani A, et al. Reading protocol for dynamic contrastenhanced MR images of the breast: sensitivity and specificity analysis. Radiology. 2005; 236:779–788.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Breast Imaging Reporting and Data System Category 4 Complex Cystic Masses of the Breast: Do All the Complex Cystic Breast Masses Merit a Biopsy?
- The Usefulness of Scoring System Distinguishing between Benign and Malignant Breast Masses on Ultrasonogram
- Benign core biopsy of probably benign breast lesions 2 cm or larger: correlation with excisional biopsy and long-term follow-up
- Is It Useful for Distinguishing between Benign and Malignant Solid Breast Masses? : Diagnostic Criteria of Japan Society of Ultrasonics in IVledicine(JSUM)
- Benign Neoplasm of the Breast