J Korean Med Sci.
2010 Aug;25(8):1251-1252. 10.3346/jkms.2010.25.8.1251.
Corneal Perforation with Preseptal Cellulitis in a Patient with Acute Lymphocytic Leukemia
- Affiliations
-
- 1Department of Ophthalmology and Research Institute of Medical Sciences, Chonnam National University Medical School and Hospital, Gwangju, Korea. kcyoon@jnu.ac.kr
- KMID: 1714055
- DOI: http://doi.org/10.3346/jkms.2010.25.8.1251
Abstract
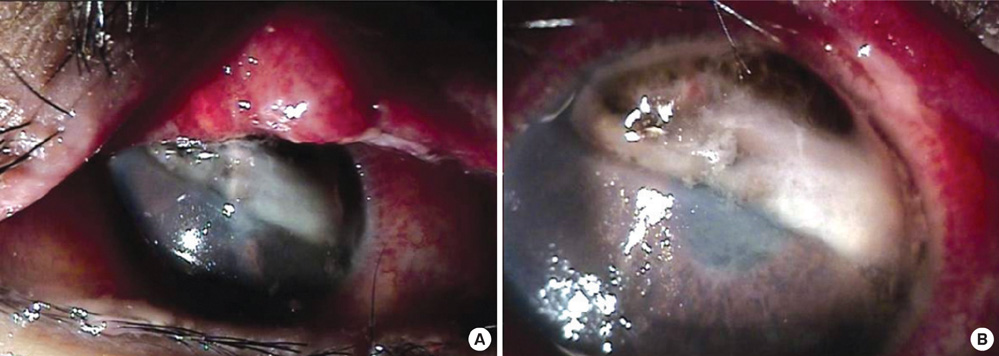
- We report a case of corneal perforation with preseptal cellulitis in a patient with acute lymphocytic leukemia (ALL). A 17-yr-old female patient who was undergoing combination chemotherapy for ALL was referred due to upper lid swelling and pain in the right eye for 2 days. Visual acuity in the right eye was 20/20. Initial examination showed no abnormal findings, other than swelling of the right upper eyelid. Computed tomography showed a finding of preseptal cellulitis. Microbiologic study of bloody and purulent discharge revealed Serratia marcescens. Corneal melting and perforation with iris prolapse were detected in the right eye on the 16th day. Emergent tectonic keratoplasty was performed. Seven months after surgery, visual acuity in the right eye was 20/300, and the corneal graft was stable.
Keyword
MeSH Terms
-
Adolescent
Anti-Bacterial Agents/therapeutic use
Cellulitis/*diagnosis/drug therapy/etiology/microbiology
Corneal Perforation/*diagnosis/etiology/therapy
Corneal Transplantation
Drug Therapy, Combination
Female
Humans
Precursor Cell Lymphoblastic Leukemia-Lymphoma/complications/*drug therapy
Serratia marcescens/isolation & purification
Tomography, X-Ray Computed
Visual Acuity
Figure
Reference
-
1. Al-Tweigeri T, Nabholtz JM, Mackey JR. Ocular toxicity and cancer chemotherapy. A review. Cancer. 1996. 78:1359–1373.
Article2. Schmid KE, Kornek GV, Scheithauer W, Binder S. Update on ocular complications of systemic cancer chemotherapy. Surv Ophthalmol. 2006. 51:19–40.
Article3. Cavallaro N, Cavallaro F, Di Pietro M, Biondi S, Lentini F. An unusual case of orbital cellulitis and perforating scleromalacia. J Fr Ophthalmol. 1999. 22:753–754.4. Lochhead J, Salmon JF, Bron AJ. Cytarabine-induced corneal toxicity. Eye (Lond). 2003. 17:677–678.
Article5. Gorin MB, Day R, Costantino JP, Fisher B, Redmond CK, Wickerham L, Gomolin JE, Margolese RG, Mathen MK, Bowman DM, Kaufman DI, Dimitrov NV, Singerman LJ, Bornstein R, Wolmark N. Long-term tamoxifen citrate use and potential ocular toxicity. Am J Ophthalmol. 1998. 125:493–501.
Article6. Equi RA, Green WR. Endogenous Serratia marcescens endophthalmitis with dark hypopyon: a case report and review. Surv Ophthalmol. 2001. 46:259–268.7. Lyerly D, Gray L, Kreger A. Characterization of rabbit corneal damage produced by Serratia keratitis and by a serratia protease. Infect Immun. 1981. 33:927–932.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cellulitis Caused by Serratia marcescens in a Patient with Acute Lymphocytic Leukemia
- A Case of Acute Lymphocytic Leukemia with Both Renal Enlargement
- Clinical Manifestations and Prognostic Factors of Ocular Infection Associated with Orbital or Preseptal Cellulitis
- Leukemia Cutis in a Patient with Acute Lymphocytic Leukemia
- Orbital Cellulitis after Strabismus Surgery