J Korean Med Sci.
2010 Jan;25(1):148-151. 10.3346/jkms.2010.25.1.148.
A Case of Mexiletine-induced Hypersensitivity Syndrome Presenting as Eosinophilic Pneumonia
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea. hjyoon@hanyang.ac.kr
- KMID: 1713847
- DOI: http://doi.org/10.3346/jkms.2010.25.1.148
Abstract
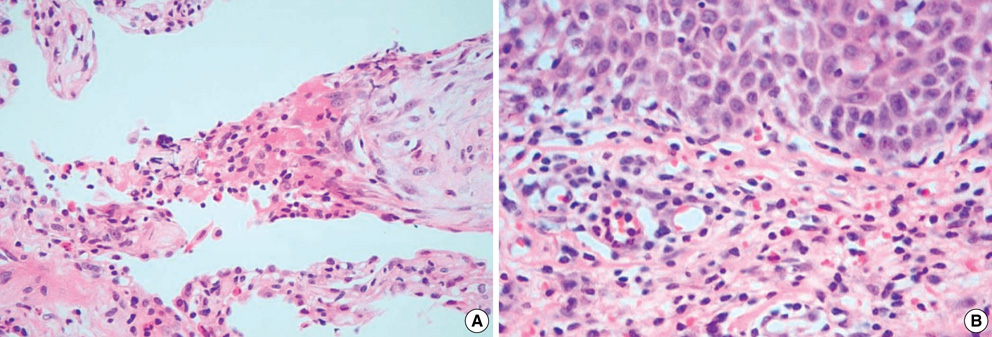
- An 82-yr-old man was presented with fever and cough accompanied by generalized erythematous rash. He had taken mexiletine for 5 months, as he had been diagnosed with dilated cardiomyopathy and ventricular arrhythmia. Laboratory studies showed peripheral blood eosinophilia and elevated liver transaminase levels. Chest radiographs showed multiple nodular consolidations in both lungs. Biopsies of the lung and skin lesions revealed eosinophilic infiltration. After a thorough review of his medication history, mexiletine was suspected as the etiologic agent. After discontinuing the mexiletine and starting oral prednisolone, the patient improved, and the skin and lung lesions disappeared. Subsequently, mexiletine was confirmed as the causative agent based on a positive patch test. Drug-induced hypersensitivity syndrome is a severe adverse reaction to drugs and results from treatment with anticonvulsants, allopurinol, sulfonamides, and many other drugs. Several cases of mexiletine-induced hypersensitivity syndrome have been reported in older Japanese males with manifestation of fever, rash, peripheral blood eosinophilia, liver dysfunction without other organ involvement. Here, we report a case of mexiletine-induced hypersensitivity syndrome which presented as eosinophilic pneumonia in a Korean male.
MeSH Terms
-
Aged, 80 and over
Anti-Arrhythmia Agents/*adverse effects
Arrhythmias, Cardiac/drug therapy
Cardiomyopathy, Dilated/drug therapy
Drug Hypersensitivity/*diagnosis/etiology
Exanthema/pathology
Humans
Lung/pathology/radiography
Male
Mexiletine/*adverse effects
Pulmonary Eosinophilia/*chemically induced/*diagnosis
Syndrome
Tomography, X-Ray Computed
Anti-Arrhythmia Agents
Mexiletine
Figure
Reference
-
1. Shiohara T, Inaoka M, Kano Y. Drug-induced hypersensitivity syndrome (DIHS): a reaction induced by a complex interplay among herpesviruses and antiviral and antidrug immune responses. Allergol Int. 2006. 55:1–8.2. Aihara Y, Ito SI, Kobayashi Y, Yamakawa Y, Aihara M, Yokota S. Carbamazepine-induced hypersensitivity syndrome associated with transient hypogammaglobulinaemia and reactivation of human herpesvirus 6 infection demonstrated by real-time quantitative polymerase chain reaction. Br J Dermatol. 2003. 149:165–169.
Article3. Talbot RG, Nimmo J, Julian DG, Clark RA, Neilson JM, Prescott LF. Treatment of ventricular arrhythmias with mexiletine (Ko 1173). Lancet. 1973. 2:399–404.4. Higa K, Hirata K, Dan K. Mexiletine-induced severe skin eruption, fever, eosinophilia, atypical lymphocytosis, and liver dysfunction. Pain. 1997. 73:97–99.
Article5. Sasaki K, Yamamoto T, Kishi M, Yokozeki H, Nishioka K. Acute exanthematous pustular drug eruption induced by mexiletine. Eur J Dermatol. 2001. 11:469–471.6. Seino Y, Yamauchi M, Hirai C, Okumura A, Kondo K, Yamamoto M, Okazaki Y. A case of fulminant type 1 diabetes associated with mexiletine hypersensitivity syndrome. Diabet Med. 2004. 21:1156–1157.
Article7. Sekiguchi A, Kashiwagi T, Ishida-Yamamoto A, Takahashi H, Hashimoto Y, Kimura H, Tohyama M, Hashimoto K, Iizuka H. Drug-induced hypersensitivity syndrome due to mexiletine associated with human herpes virus 6 and cytomegalovirus reactivation. J Dermatol. 2005. 32:278–281.
Article8. Yagami A, Yoshikawa T, Asano Y, Koie S, Shiohara T, Matsunaga K. Drug-induced hypersensitivity syndrome due to mexiletine hydrochloride associated with reactivation of human herpesvirus 7. Dermatology. 2006. 213:341–344.
Article9. Wilkinson DS, Fregert S, Magnusson B, Bandmann HJ, Calnan CD, Cronin E, Hjorth N, Maibach HJ, Malalten KE, Meneghini CL, Pirila V. Terminology of contact dermatitis. Acta Derm Venereol. 1970. 50:287–292.10. Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (drug rash with eosinophilia and systemic symptoms: Dress). Semin Cutan Med Surg. 1996. 15:250–257.
Article11. Shear NH, Spielberg SP. Anticonvulsant hypersensitivity syndrome. In vitro assessment of risk. J Clin Invest. 1988. 82:1826–1832.
Article12. Chung WH, Hung SI, Hong HS, Hsih MS, Yang LC, Ho HC, Wu JY, Chen YT. Medical genetics: A marker for stevens-johnson syndrome. Nature. 2004. 428:486.13. Lonjou C, Thomas L, Borot N, Ledger N, de Toma C, LeLouet H, Graf E, Schumacher M, Hovnanian A, Mockenhaupt M, Roujeau JC. A marker for stevens-johnson syndrome...: Ethnicity matters. Pharmacogenomics J. 2006. 6:265–268.14. Chung WH, Hung SI, Chen YT. Human leukocyte antigens and drug hypersensitivity. Curr Opin Allergy Clin Immunol. 2007. 7:317–323.
Article15. Sullivan JR, Shear NH. The drug hypersensitivity syndrome: What is the pathogenesis? Arch Dermatol. 2001. 137:357–364.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of carbamazepine-induced anticonvulsant hypersensitivity syndrome expressing eosinophilic pneumonia
- A Case of Anticonvulsant Hypersensitivity Syndrome with Subcarinal Lymph node Enlargement and Eosinophilic Pneumonia Induced by Carbamazepine
- Acute Eosinophilic Pneumonia: A Case Report
- Clinical Study of Antiarrhythmic Effect of Mexiletine
- A Case of Eosinophilic Cholecystitis associated with Eosinophilic Cholangitis and Pancreatitis