J Korean Med Sci.
2007 Apr;22(2):248-253. 10.3346/jkms.2007.22.2.248.
Relationship between Twin-to-twin Delivery Interval and Umbilical Artery Acid-base Status in the Second Twin
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, 300 Gumi-dong, Bundang-gu, Seongnam, Korea. pkh0419@snubh.org
- 3Department of Obstetrics and Gynecology, Seoul National University Hospital, Seoul, Korea.
- KMID: 1713179
- DOI: http://doi.org/10.3346/jkms.2007.22.2.248
Abstract
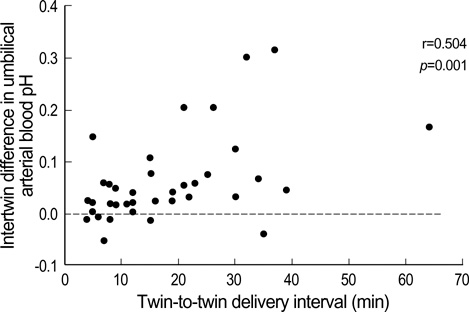
- The purpose of this study was to determine the effect of twin-to-twin delivery interval on umbilical artery acid-base status of the second twin at birth. This was a retrospective cohort study of all live-born twins with measured acid-base status in umbilical arterial blood who were delivered after 34 weeks' gestation from June 2003 to February 2006. Twins with any maternal or fetal complications were excluded. Subjects were divided into two groups based on the mode of delivery of the first twin: normal cephalic vaginal deliveries (n=40) or cesarean deliveries (n=67). The inter-twin differences in umbilical arterial blood pH, PCO2, PO2, and base excess in twin newborns born vaginally were significantly greater than the corresponding differences in those born by cesarean section. A significant positive correlation was found between twin-to-twin delivery interval and inter-twin difference in umbilical arterial blood pH in twin newborns born vaginally. The umbilical arterial blood pH of the second twin was less than 7.0 in 14% (2/14) in cases delivered more than 20 min after the first twin. The umbilical arterial blood gas status of the second twin worsened with increasing twin-to-twin delivery interval, and pathologic fetal acidemia (pH<7.0) might develop in the second twin when the twin-to-twin delivery interval was greater than 20 min.
MeSH Terms
Figure
Reference
-
1. Ho SK, Wu PY. Perinatal factors and neonatal morbidity in twin pregnancy. Am J Obstet Gynecol. 1975. 122:979–987.
Article2. McCarthy BJ, Sachs BP, Layde PM, Burton A, Terry JS, Rochat R. The epidemiology of neonatal death in twins. Am J Obstet Gynecol. 1981. 141:252–256.
Article3. Spellacy WN, Handler A, Ferre CD. A case-control study of 1253 twin pregnancies from a 1982-1987 perinatal data base. Obstet Gynecol. 1990. 75:168–171.4. Gardner MO, Goldenberg RL, Cliver SP, Tucker JM, Nelson KG, Copper RL. The origin and outcome of preterm twin pregnancies. Obstet Gynecol. 1995. 85:553–557.
Article5. Smith GC, Pell JP, Dobbie R. Birth order, gestational age, and risk of delivery related perinatal death in twins: retrospective cohort study. BMJ. 2002. 325:1004–1008.
Article6. Ferguson WF. Perinatal mortality in multiple gestations: a review of Perinatal deaths from 1609 multiple gestations. Obstet Gynecol. 1964. 23:861–870.7. Ware HH. The second twin. Am J Obstet Gynecol. 1971. 110:865–873.
Article8. Spurway JH. The fate and management of the second twin. Am J Obstet Gynecol. 1962. 83:1377–1388.
Article9. Langer H. Perinatal mortality in twins. Zentralbl Gynakol. 1972. 94:1288–1296.10. Farooqui MO, Grossman JH, Shannon RA. A review of twin pregnancy and perinatal mortality. Obstet Gynecol Surv. 1973. 28:144–153.
Article11. Rayburn WF, Lavin JP, Miodovnik M, Varner MW. Multiple gestation: Time interval between delivery of the first and second twins. Obstet Gynecol. 1984. 63:502–506.12. Rydhstrom H, Ingemarsson I. Interval between birth of the first and the second twin and its impact on second twin perinatal mortality. J Perinat Med. 1990. 18:449–453.13. Thompson SA, Lyons TL, Makowski EL. Outcome of twin gestations at the University of Colorado Health Science Center, 1973-1983. J Reprod Med. 1987. 32:328–339.14. Chervenak FA, Johnson RE, Youcha S, Hobbins JC, Berkowitz RL. Intrapartum management of twin gestation. Obstet Gynecol. 1985. 65:119–124.15. Sykes GS, Molloy PM, Johnson P, Gu W, Ashworth F. Do Apgar scores indicate asphyxia? Lancet. 1982. 1:494–496.
Article16. Nelson KB, Ellenberg JH. Apgar scores as predictors of chronic neurologic disability. Pediatrics. 1981. 68:36–44.17. Freeman JM, Nelson KB. Intrapartum asphyxia and cerebral palsy. Pediatrics. 1988. 82:240–249.18. Usta IM, Rechdan JB, Khalil AM, Nassar AH. Mode of delivery for vertex-nonvertex twin gestations. Int J Gynaecol Obstet. 2005. 88:9–14.
Article19. Chauhan SP, Roberts WE, McLaren RA, Roach H, Morrison JC, Martin JN Jr. Delivery of the nonvertex second twin: breech extraction versus external cephalic version. Am J Obstet Gynecol. 1995. 173:1015–1020.20. Hartley RS, Hitti J. Birth order and delivery interval: analysis of twin pair perinatal outcomes. J Matern Fetal Neonatal Med. 2005. 17:375–380.
Article21. Brown HL, Miller JM Jr, Neumann DE, Sarpong DF, Gabert HA. Umbilical cord blood gas assessment of twins. Obstet Gynecol. 1990. 75:826–829.
Article22. Young BK, Suidan J, Antoine C, Silverman F, Lustig I, Wasserman J. Differences in twins: the importance of birth order. Am J Obstet Gynecol. 1985. 151:915–923.
Article23. Nakano R, Takemura H. Birth order in delivery of twins. Gynecol Obstet Invest. 1988. 25:217–222.
Article24. Yancey MK, Harlass FE. Extraneous factors and their influences on fetal acid-base status. Clin Obstet Gynecol. 1993. 36:60–72.
Article25. Yoon BH, Kim SW. The effect of labor on the normal values of umbilical blood acid-base status. Acta Obstet Gynecol Scand. 1994. 73:555–561.
Article26. Maymon R, Herman A, Halperin R, Bukovsky I, Weinraub Z, Ariely S. Changes in uterine artery Doppler flow velocity waveforms during the third stage of labor. Gynecol Obstet Invest. 1995. 40:24–27.
Article27. Cunningham FG, MacDonald PC, Gant NF, Leveno KJ, Gilstrap LC, Hankins GD, Clark SL. Cunningham FG, MacDonald PC, Gant NF, Leveno KJ, Gilstrap LC, Hankins GD, Clark SL, editors. Obstetrical hemorrhage. Williams Obstetrics. 1997. 20th ed. Norwalk (CT): Appleton & Lange;745–782.28. Gupta JK, Hofmeyr GJ. Position for women during second stage of labour. Cochrane Database Syst Rev. 2004. 1:CD002006.
Article29. Leung TY, Tam WH, Leung TN, Lok IH, Lau TK. Effect of twin-to-twin delivery interval on umbilical cord blood gas in the second twins. BJOG. 2002. 109:63–67.
Article30. American college of obstetricians and gynecologists. Committee Opinion, No. 174. Use and abuse of the Apgar score. 1996. July.31. Gilstrap LC 3rd, Leveno KJ, Burris J, Williams ML, Little BB. Diagnosis of birth asphyxia on the basis of fetal pH, Apgar score, and newborn cerebral dysfunction. Am J Obstet Gynecol. 1989. 161:825–830.
Article32. Chauhan SP, Roberts WE. Gall SA, editor. Intrapartum management. Multiple pregnancy and delivery. 1996. St. Louis: Mosby-Year Book;243–280.33. American College of Obstetricians and Gynecologists. Education Bulletin No. 253. Special problems of multiple gestation. 1998. November.34. Laros RK Jr, Dattel BJ. Management of twin pregnancy: the vaginal route is still safe. Am J Obstet Gynecol. 1988. 158:1330–1338.
Article35. Hogle KL, Hutton EK, McBrien KA, Barrett JF, Hannah ME. Cesarean delivery for twins: a systematic review and meta-analysis. Am J Obstet Gynecol. 2003. 188:220–227.
Article36. McGrail CD, Bryant DR. Intertwin time interval: how it affects the immediate neonatal outcome of the second twin. Am J Obstet Gynecol. 2005. 192:1420–1422.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- One Case of Monoamniotic Twin with Entanglement of Umbilical Cord and a Single Fetal Death in Uterus - One Case Report -
- A Successful Delayed-Interval Delivery without Cerclage Operation after One Fetal Delivery in a Case of Twin Pregnancy
- The significance of umbilical artery velocimetry in twin pregnancies
- A Case of Acute Twin-Twin Transfusion Syndrome
- A cass of Twin to Twin Transfusion Syndrome