Korean J Radiol.
2014 Feb;15(1):114-122. 10.3348/kjr.2014.15.1.114.
MR Findings of the Osteofibrous Dysplasia
- Affiliations
-
- 1Department of Radiology, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea. whjee@catholic.ac.kr
- 2Department of Radiology, Seoul National University College of Medicine, Seoul 110-744, Korea.
- 3Department of Radiology, Seoul National University Bundang Hospital, Seongnam 463-707, Korea.
- 4Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea.
- 5Department of Radiology, Kyung Hee University College of Medicine, Seoul 130-872, Korea.
- 6Department of Radiology, Korea University College of Medicine, Seoul 136-705, Korea.
- 7Department of Pathology, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea.
- 8Department of Orthopedic Surgery, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea.
- KMID: 1711485
- DOI: http://doi.org/10.3348/kjr.2014.15.1.114
Abstract
OBJECTIVE
The aim of this study was to describe MR findings of osteofibrous dysplasia.
MATERIALS AND METHODS
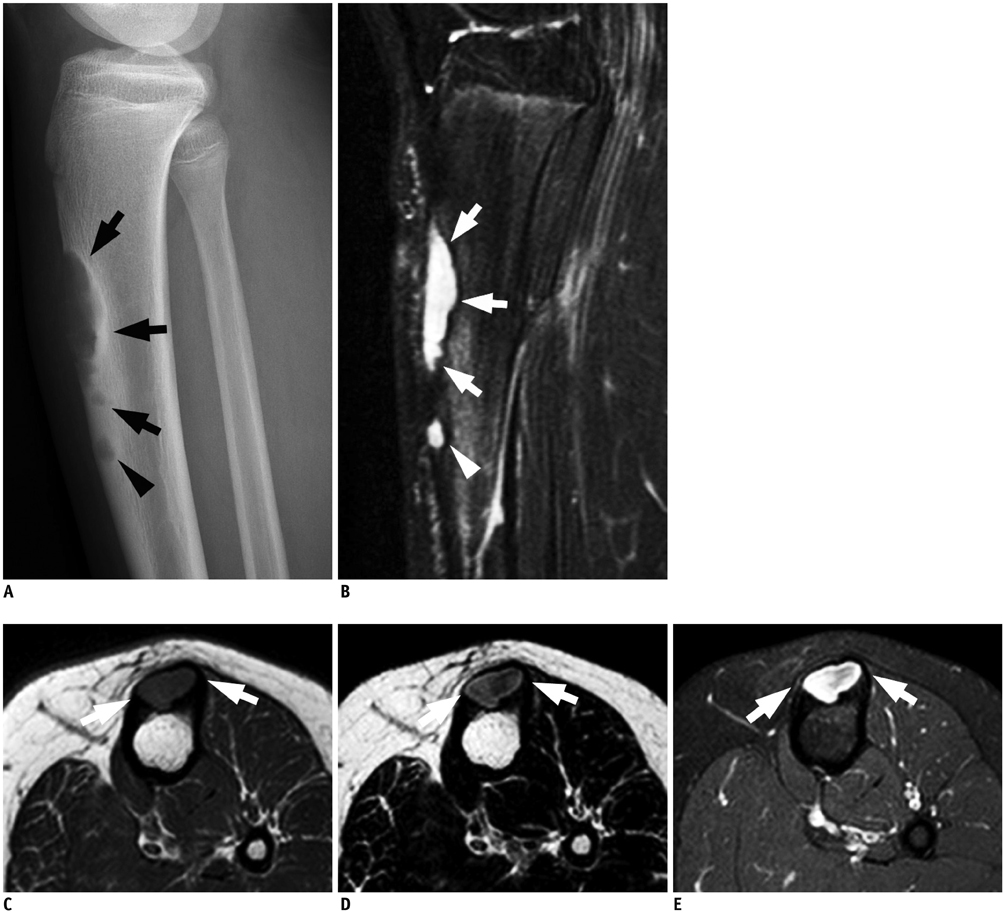
MR images of 24 pathologically proven osteofibrous dysplasia cases were retrospectively analyzed for a signal intensity of the lesion, presence of intralesional fat signal, internal hypointense band, multilocular appearance, cortical expansion, intramedullary extension, cystic area, cortical breakage and extraosseous extension, abnormal signal from the adjacent bone marrow and soft tissue and patterns of contrast enhancement.
RESULTS
All cases of osteofibrous dysplasia exhibited intermediate signal intensity on T1-weighted images. On T2-weighted images, 20 and 4 cases exhibited heterogeneously intermediate and high signal intensity, respectively. Intralesional fat was identified in 12% of the cases. Internal low-signal bands and multilocular appearance were observed in 91%. Cortical expansion was present in 58%. Intramedullary extension was present in all cases, and an entire intramedullary replacement was observed in 33%. Cortical breakage (n = 3) and extraosseous mass formation (n = 1) were observed in cases with pathologic fractures only. A cystic area was observed in one case. Among 21 cases without a pathologic fracture, abnormal signal intensity in the surrounding bone marrow and adjacent soft tissue was observed in 43% and 48%, respectively. All cases exhibited diffuse contrast enhancement.
CONCLUSION
Osteofibrous dysplasia exhibited diverse imaging features ranging from lesions confined to the cortex to more aggressive lesions with complete intramedullary involvement or perilesional marrow edema.
MeSH Terms
Figure
Reference
-
1. Campanacci M, Laus M. Osteofibrous dysplasia of the tibia and fibula. J Bone Joint Surg Am. 1981; 63:367–375.2. Campbell CJ, Hawk T. A variant of fibrous dysplasia (osteofibrous dysplasia). J Bone Joint Surg Am. 1982; 64:231–236.3. Mirra JM, Picci P. Osteofibrous dysplasia (juvenile adamantinoma?). In : Mirra JM, editor. Bone Tumors-Clinical, Radiologic, and Pathologic Correlations. Philadelphia: Lea & Febiger;1989. p. 1217–1231.4. Resnick D, Kyriakos M, Greenway GD. Tumors and tumor-like lesions of bone: Imaging and pathology of specific lesions. In : Resnick D, editor. Diagnosis of Bone and Joint Disorders. 4th ed. Philadelphia: Saunders;2002. p. 3796–3800.5. Goergen TG, Dickman PS, Resnick D, Saltzstein SL, O'Dell CW, Akeson WH. Long bone ossifying fibromas. Cancer. 1977; 39:2067–2072.6. Park YK, Unni KK, McLeod RA, Pritchard DJ. Osteofibrous dysplasia: clinicopathologic study of 80 cases. Hum Pathol. 1993; 24:1339–1347.7. Dominguez R, Saucedo J, Fenstermacher M. MRI findings in osteofibrous dysplasia. Magn Reson Imaging. 1989; 7:567–570.8. Khanna M, Delaney D, Tirabosco R, Saifuddin A. Osteofibrous dysplasia, osteofibrous dysplasia-like adamantinoma and adamantinoma: correlation of radiological imaging features with surgical histology and assessment of the use of radiology in contributing to needle biopsy diagnosis. Skeletal Radiol. 2008; 37:1077–1084.9. Gleason BC, Liegl-Atzwanger B, Kozakewich HP, Connolly S, Gebhardt MC, Fletcher JA, et al. Osteofibrous dysplasia and adamantinoma in children and adolescents: a clinicopathologic reappraisal. Am J Surg Pathol. 2008; 32:363–376.10. Springfield DS, Rosenberg AE, Mankin HJ, Mindell ER. Relationship between osteofibrous dysplasia and adamantinoma. Clin Orthop Relat Res. 1994; (309):234–244.11. Murphey MD, wan Jaovisidha S, Temple HT, Gannon FH, Jelinek JS, Malawer MM. Telangiectatic osteosarcoma: radiologic-pathologic comparison. Radiology. 2003; 229:545–553.12. Goto T, Kojima T, Iijima T, Yokokura S, Kawano H, Yamamoto A, et al. Osteofibrous dysplasia of the ulna. J Orthop Sci. 2001; 6:608–611.13. Nakashima Y, Yamamuro T, Fujiwara Y, Kotoura Y, Mori E, Hamashima Y. Osteofibrous dysplasia (ossifying fibroma of long bones). A study of 12 cases. Cancer. 1983; 52:909–991.14. Williams HK, Mangham C, Speight PM. Juvenile ossifying fibroma. An analysis of eight cases and a comparison with other fibro-osseous lesions. J Oral Pathol Med. 2000; 29:13–18.15. Kahn LB. Adamantinoma, osteofibrous dysplasia and differentiated adamantinoma. Skeletal Radiol. 2003; 32:245–258.16. Teo HE, Peh WC, Akhilesh M, Tan SB, Ishida T. Congenital osteofibrous dysplasia associated with pseudoarthrosis of the tibia and fibula. Skeletal Radiol. 2007; 36:Suppl 1. S7–S14.17. Wang JW, Shih CH, Chen WJ. Osteofibrous dysplasia (ossifying fibroma of long bones). A report of four cases and review of the literature. Clin Orthop Relat Res. 1992; (278):235–243.18. Jee WH, Choe BY, Kang HS, Suh KJ, Suh JS, Ryu KN, et al. Nonossifying fibroma: characteristics at MR imaging with pathologic correlation. Radiology. 1998; 209:197–202.19. Jee WH, Choi KH, Choe BY, Park JM, Shinn KS. Fibrous dysplasia: MR imaging characteristics with radiopathologic correlation. AJR Am J Roentgenol. 1996; 167:1523–1527.20. Utz JA, Kransdorf MJ, Jelinek JS, Moser RP Jr, Berrey BH. MR appearance of fibrous dysplasia. J Comput Assist Tomogr. 1989; 13:845–851.21. Van der Woude HJ, Hazelbag HM, Bloem JL, Taminiau AH, Hogendoorn PC. MRI of adamantinoma of long bones in correlation with histopathology. AJR Am J Roentgenol. 2004; 183:1737–1744.22. Ishida T, Iijima T, Kikuchi F, Kitagawa T, Tanida T, Imamura T, et al. A clinicopathological and immunohistochemical study of osteofibrous dysplasia, differentiated adamantinoma, and adamantinoma of long bones. Skeletal Radiol. 1992; 21:493–502.23. Markel SF. Ossifying fibroma of long bone: its distinction from fibrous dysplasia and its association with adamantinoma of long bone. Am J Clin Pathol. 1978; 69:91–97.24. Mori H, Yamamoto S, Hiramatsu K, Miura T, Moon NF. Adamantinoma of the tibia. Ultrastructural and immunohistochemic study with reference to histogenesis. Clin Orthop Relat Res. 1984; (190):299–310.25. Sweet DE, Vinh TN, Devaney K. Cortical osteofibrous dysplasia of long bone and its relationship to adamantinoma. A clinicopathologic study of 30 cases. Am J Surg Pathol. 1992; 16:282–290.26. Bloem JL, van der Heul RO, Schuttevaer HM, Kuipers D. Fibrous dysplasia vs adamantinoma of the tibia: differentiation based on discriminant analysis of clinical and plain film findings. AJR Am J Roentgenol. 1991; 156:1017–1023.27. Czerniak B, Rojas-Corona RR, Dorfman HD. Morphologic diversity of long bone adamantinoma. The concept of differentiated (regressing) adamantinoma and its relationship to osteofibrous dysplasia. Cancer. 1989; 64:2319–2334.28. Hazelbag HM, Taminiau AH, Fleuren GJ, Hogendoorn PC. Adamantinoma of the long bones. A clinicopathological study of thirty-two patients with emphasis on histological subtype, precursor lesion, and biological behavior. J Bone Joint Surg Am. 1994; 76:1482–1499.29. Kransdorf MJ, Stull MA, Gilkey FW, Moser RP Jr. Osteoid osteoma. Radiographics. 1991; 11:671–696.30. Tehranzadeh J, Wong E, Wang F, Sadighpour M. Imaging of osteomyelitis in the mature skeleton. Radiol Clin North Am. 2001; 39:223–250.31. López-Barea F, Hardisson D, Rodríguez-Peralto JL, Sánchez-Herrera S, Lamas M. Intracortical hemangioma of bone. Report of two cases and review of the literature. J Bone Joint Surg Am. 1998; 80:1673–1678.32. Mahnken AH, Nolte-Ernsting CC, Wildberger JE, Heussen N, Adam G, Wirtz DC, et al. Aneurysmal bone cyst: value of MR imaging and conventional radiography. Eur Radiol. 2003; 13:1118–1124.33. Kroon HM, Schurmans J. Osteoblastoma: clinical and radiologic findings in 98 new cases. Radiology. 1990; 175:783–790.34. Lädermann A, Stern R, Ceroni D, De Coulon G, Taylor S, Kaelin A. Unusual radiologic presentation of monostotic fibrous dysplasia. Orthopedics. 2008; 31:282.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Osteofibrous Dysplasia of The Femoral Shaft
- Congenital Osteofibrous Dysplasia, Involving the Tibia of a Neonate
- Treatment of Osteofibrous Dysplasia and Associated Lesions
- Osteofibrous Dysplasia of the Tibia in Children
- Importance of Extraperiosteal Excision in Surgical Treatment of Osteofibrous Dysplasia