Korean J Ophthalmol.
2013 Oct;27(5):376-380. 10.3341/kjo.2013.27.5.376.
Acute Central Retinal Artery Occlusion Associated with Livedoid Vasculopathy: A Variant of Sneddon's Syndrome
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. sejoon1@hanmail.net
- 2Department of Biomedical Sciences, Seoul National University Graduate School, Seoul, Korea.
- 3Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 4Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 5Department of Neurosurgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- KMID: 1707293
- DOI: http://doi.org/10.3341/kjo.2013.27.5.376
Abstract
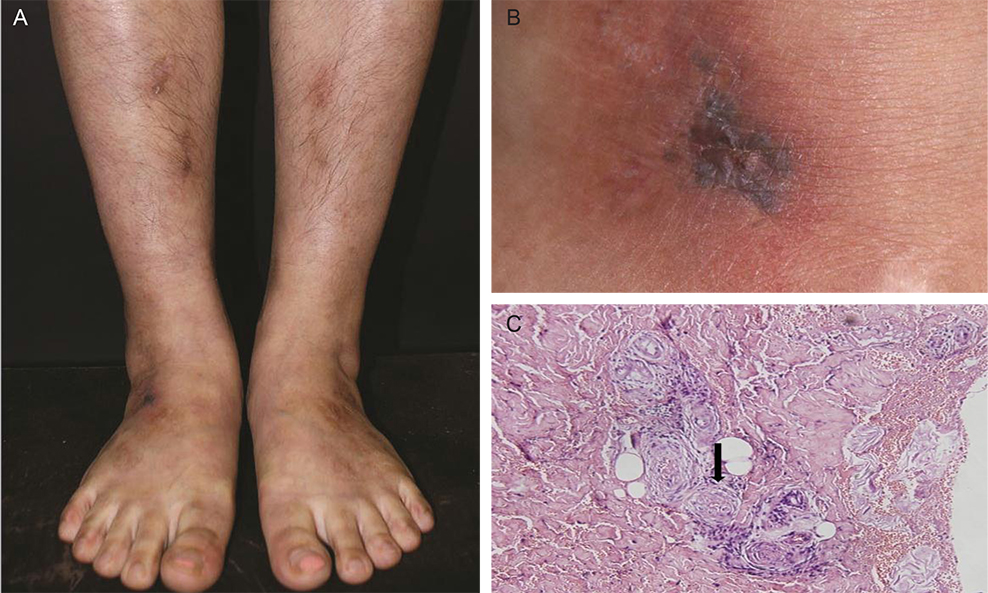
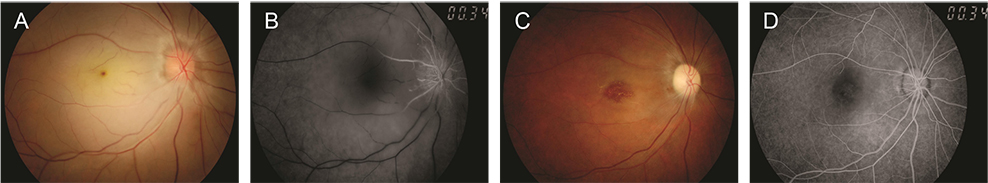
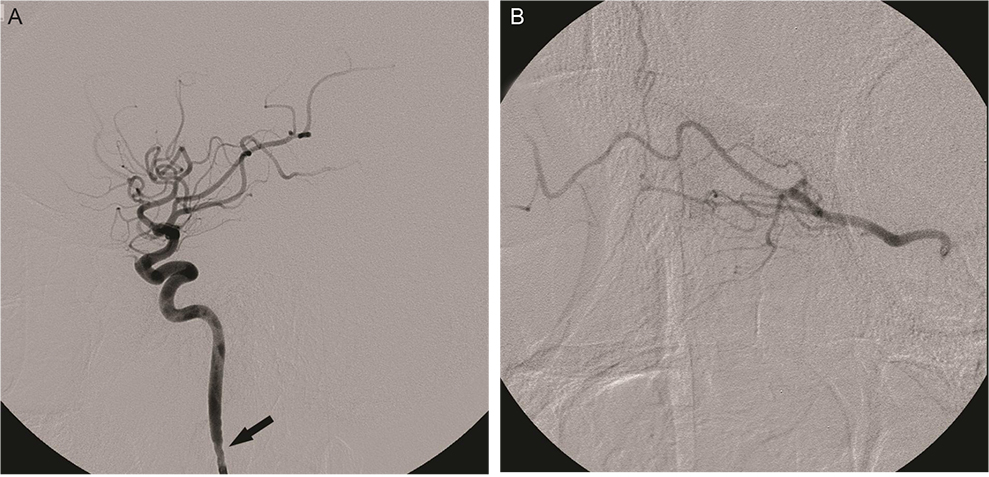
- Livedoid vasculopathy (LV) is characterized by a long history of ulceration of the feet and legs and histopathology indicating a thrombotic process. We report a case of acute central retinal artery occlusion in a 32-year-old woman who had LV. She showed no discernible laboratory abnormalities such as antiphospholipid antibodies and no history of cerebrovascular accidents. Attempted intra-arterial thrombolysis showed no effect in restoring retinal arterial perfusion or vision. The central retinal artery occlusion accompanied by LV in this case could be regarded as a variant form of Sneddon's syndrome, which is characterized by livedo reticularis and cerebrovascular accidents.
Keyword
MeSH Terms
Figure
Reference
-
1. Khenifer S, Thomas L, Balme B, Dalle S. Livedoid vasculopathy: thrombotic or inflammatory disease? Clin Exp Dermatol. 2010; 35:693–698.2. Read RW, Chong LP, Rao NA. Occlusive retinal vasculitis associated with systemic lupus erythematosus. Arch Ophthalmol. 2000; 118:588–589.3. Mirza S, Raghu Ram AR, Bowling BS, Nessim M. Central retinal artery occlusion and bilateral choroidal infarcts in Wegener's granulomatosis. Eye (Lond). 1999; 13(Pt 3a):374–376.4. Warrasak S, Tapaneya-Olarn W, Euswas A, et al. Fibromuscular dysplasia: a rare cause of cilioretinal artery occlusion in childhood. Ophthalmology. 2000; 107:737–741.5. Shimizu K, Numaga J, Takahashi M, Matsunaga T. A case of Sneddon syndrome. Nihon Ganka Gakkai Zasshi. 1995; 99:104–108.6. Jonas J, Kolble K, Volcker HE, Kalden JR. Central retinal artery occlusion in Sneddon's disease associated with antiphospholipid antibodies. Am J Ophthalmol. 1986; 102:37–40.7. Pauranik A, Parwani S, Jain S. Simultaneous bilateral central retinal arterial occlusion in a patient with Sneddon syndrome: case history. Angiology. 1987; 38(2 Pt 1):158–163.8. Alegre VA, Winkelmann RK, Gastineau DA. Cutaneous thrombosis, cerebrovascular thrombosis, and lupus anticoagulant--the Sneddon syndrome: report of 10 cases. Int J Dermatol. 1990; 29:45–49.9. Rehany U, Kassif Y, Rumelt S. Sneddon's syndrome: neuro-ophthalmologic manifestations in a possible autosomal recessive pattern. Neurology. 1998; 51:1185–1187.10. Hayreh SS, Podhajsky PA, Zimmerman MB. Retinal artery occlusion: associated systemic and ophthalmic abnormalities. Ophthalmology. 2009; 116:1928–1936.11. Ivanisević M, Karelovic D. The incidence of central retinal artery occlusion in the district of Split, Croatia. Ophthalmologica. 2001; 215:245–246.12. Kollarits CR, Lubow M, Hissong SL. Retinal strokes. I. Incidence of carotid atheromata. JAMA. 1972; 222:1273–1275.13. Brown GC, Magargal LE, Shields JA, et al. Retinal arterial obstruction in children and young adults. Ophthalmology. 1981; 88:18–25.14. Greven CM, Slusher MM, Weaver RG. Retinal arterial occlusions in young adults. Am J Ophthalmol. 1995; 120:776–783.15. Calamia KT, Balabanova M, Perniciaro C, Walsh JS. Livedo (livedoid) vasculitis and the factor V Leiden mutation: additional evidence for abnormal coagulation. J Am Acad Dermatol. 2002; 46:133–137.16. McCalmont CS, McCalmont TH, Jorizzo JL, et al. Livedo vasculitis: vasculitis or thrombotic vasculopathy? Clin Exp Dermatol. 1992; 17:4–8.17. Klein KL, Pittelkow MR. Tissue plasminogen activator for treatment of livedoid vasculitis. Mayo Clin Proc. 1992; 67:923–933.18. Acland KM, Darvay A, Wakelin SH, Russell-Jones R. Livedoid vasculitis: a manifestation of the antiphospholipid syndrome? Br J Dermatol. 1999; 140:131–135.19. Grob JJ, Bonerandi JJ. Thrombotic skin disease as a marker of the anticardiolipin syndrome: livedo vasculitis and distal gangrene associated with abnormal serum antiphospholipid activity. J Am Acad Dermatol. 1989; 20:1063–1069.20. Biousse V, Calvetti O, Bruce BB, Newman NJ. Thrombolysis for central retinal artery occlusion. J Neuroophthalmol. 2007; 27:215–230.21. Sneddon IB. Cerebro-vascular lesions and livedo reticularis. Br J Dermatol. 1965; 77:180–185.22. Aladdin Y, Hamadeh M, Butcher K. The Sneddon syndrome. Arch Neurol. 2008; 65:834–835.23. Asherson RA, Cervera R, de Groot PG, et al. Catastrophic antiphospholipid syndrome: international consensus statement on classification criteria and treatment guidelines. Lupus. 2003; 12:530–534.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter to the Editor: Sneddon's Syndrome versus Susac Syndrome
- Incomplete Central Retinal Artery Occlusion
- A Case of Secondary Antiphospholipid Syndrome with Systemic Erythematosus Lupus Who Presenting Livedo Reticularis, Livedoid Vasculopathy, Peripheral Gangrene, and Leg Ulcers
- The Successful Treatment of a Case of Central Retinal Artery Occlusion
- Central Retinal Artery Occlusion Masquerading as Branch Retinal Artery Occlusion