Lab Med Online.
2014 Jul;4(3):168-171. 10.3343/lmo.2014.4.3.168.
The Use of High-dose Rh Immunoglobulin for the Prevention of D Sensitization in RhD-incompatible Liver Transplantation
- Affiliations
-
- 1Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea. hyunok1019@yuhs.ac
- 2Department of Laboratory Medicine, Konyang University College of Medicine, Nonsan, Korea.
- 3Department of Surgery, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1706855
- DOI: http://doi.org/10.3343/lmo.2014.4.3.168
Abstract
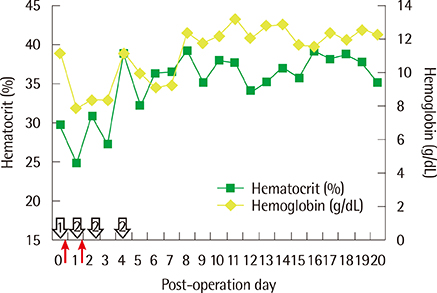
- Approximately 80-85% of D-negative (D-) persons produce anti-D antibodies after exposure to D-positive (D+) red blood cells (RBCs). Previously, anti-D was the most commonly detected Rh antibody, but its incidence has greatly decreased due to the prophylactic use of Rh immunoglobulin (RhIG). Anti-D antibody formation may occur following RhD-incompatible organ transplantation when D- recipients are exposed to D+ RBCs that originate from a donor organ. As a large volume of donor blood may be contained within the transplanted organ, the use of a large amount of RhIG is required in RhD-incompatible liver transplantation. Here, we describe the use of a large amount of RhIG to treat a patient following RhD-incompatible liver transplantation. This patient was a 71-yr-old woman with hepatitis C virus-related liver cirrhosis, who had an A/D- blood type. The donor was her grandson, whose blood type was O/D+. The recipient's preoperative anti-D antibody test was negative. One unit of O/D- irradiated leukoreduced RBCs and three units of A/D- fresh frozen plasma were transfused during liver transplantation. An equal amount (12,000 IU) of RhIG was infused intravenously, immediately after liver transplantation and a second time on post-operation day 1. The anti-D titer was 1:64 on the first post-operation day, and had increased to 1:128 by the following day. By 1 month after the surgery, the titer had decreased to 1:4. In this case of liver transplantation, RhIG was actively used to prevent RhD sensitization and the subsequent occurrence of adverse events associated with RhD-incompatible liver transplantation.
MeSH Terms
Figure
Reference
-
1. Hillyer CD, Silberstein LE, editors. Blood banking and transfusion medicine: Basic principles and practice. 2nd ed. Philadelphia: Churchill Livingstone;2007. p. 86.2. Roback JD, Brenda JG, editors. Technical manual. 17th ed. Bethesda: American Association of Blood Banks;2011. p. 636–638.3. Sebring ES, Polesky HF. Fetomaternal hemorrhage: incidence, risk factors, time of occurrence, and clinical effects. Transfusion. 1990; 30:344–357.
Article4. Ayache S, Herman JH. Prevention of D sensitization after mismatched transfusion of blood components: toward optimal use of RhIG. Transfusion. 2008; 48:1990–1999.
Article5. Lee SH, Chu CW, Yang KH, Ryu JH, Moon KM, Kim HH. A first experience of Rh(D) incompatible living related liver transplantation in Korea. Korean J Blood Transfus. 2012; 23:267–271.6. Cangene corporation. WinRho SDF Prescribing information. Updated on December 2010. http://www.winrho.com/pi.pdf.7. Hwang S, Lee SG, Kim KH, Park KM, Ahn CS, Moon DB, et al. Correlation of blood-free graft weight and volumetric graft volume by an analysis of blood content in living donor liver grafts. Transplant Proc. 2002; 34:3293–3294.
Article8. Gaines AR. Acute onset hemoglobinemia and/or hemoglobinuria and sequelae following Rho(D) immune globulin intravenous administration in immune thrombocytopenic purpura patients. Blood. 2000; 95:2523–2529.
Article9. Han KS, Park MH, Cho HI. Transfusion medicine. 3rd ed. Seoul: Korea Medical Book Publisher;2006. p. 214–219.10. Osman Y, El-Husseini A, Sheashaa H, Amani M, Bakr MA, El-Din AB. Impact of Rh(D) blood group system on graft function and survival in live-donor kidney transplantation: a single-institution experience. Transplantation. 2004; 78:1693–1696.
Article11. Casanueva M, Valdes MD, Ribera MC. Lack of alloimmunization to D antigen in D-negative immunosuppressed liver transplant recipients. Transfusion. 1994; 34:570–572.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Heart Transplantation Despite Rhesus Blood Type Mismatch: A Case Report
- Overcoming high pre-transplant isoagglutinin titers using high-dose intravenous immunoglobulin, salvage plasmapheresis, and booster rituximab without splenectomy in ABO-incompatible living donor liver transplantation: a case report
- A First Experience of Rh(D) Incompatible Living Related Liver Transplantation in Korea
- Anesthetic experience of a combined ABO- and Rh-incompatible living donor liver transplantation between an O Rh- recipient and a B Rh+ donor
- ABO-incompatible living donor liver transplantation with a simplified desensitization and immunosuppression protocol: a single center retrospective study