Korean J Ophthalmol.
2013 Aug;27(4):249-255. 10.3341/kjo.2013.27.4.249.
The Recovery of Optical Quality after Laser Vision Correction
- Affiliations
-
- 1HanGil Eye Hospital, Incheon, Korea. limthnet@naver.com
- KMID: 1705420
- DOI: http://doi.org/10.3341/kjo.2013.27.4.249
Abstract
- PURPOSE
To evaluate the optical quality after laser in situ keratomileusis (LASIK) or serial photorefractive keratectomy (PRK) using a double-pass system and to follow the recovery of optical quality after laser vision correction.
METHODS
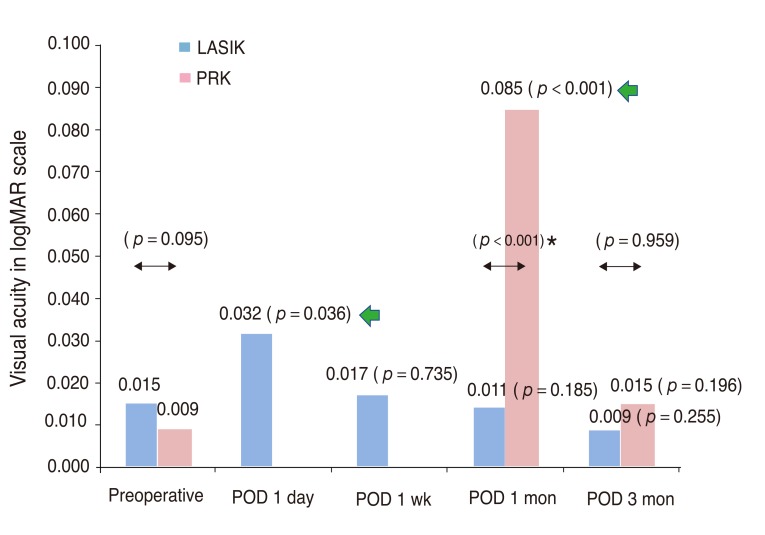
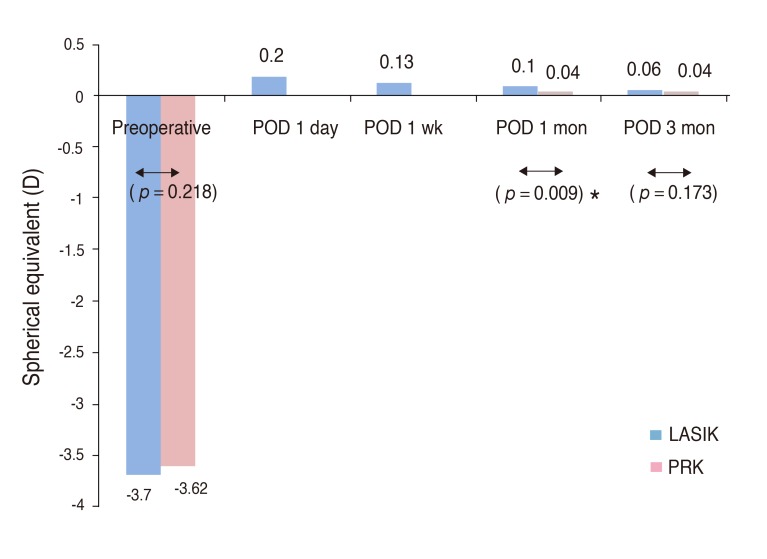
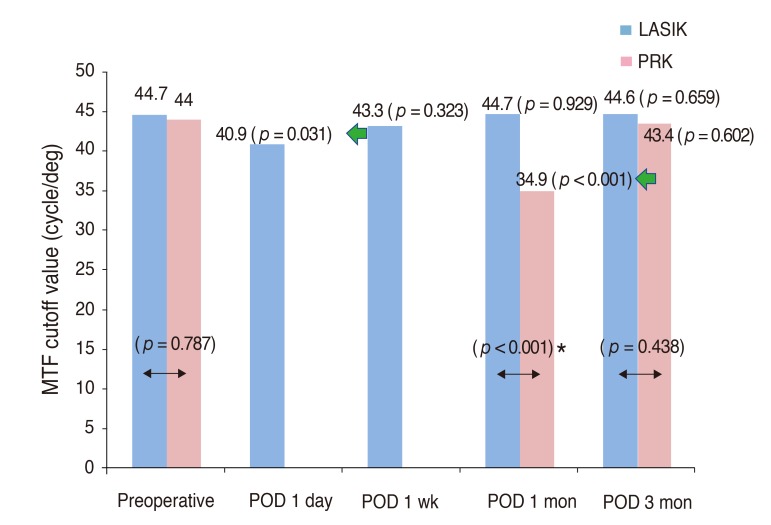
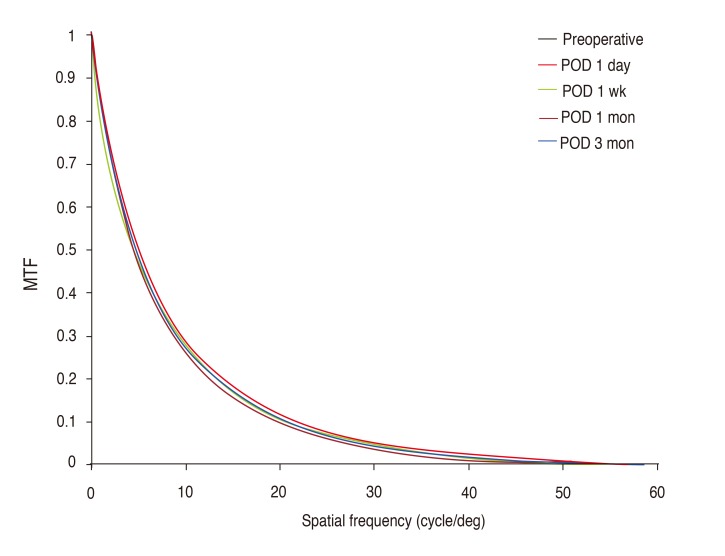
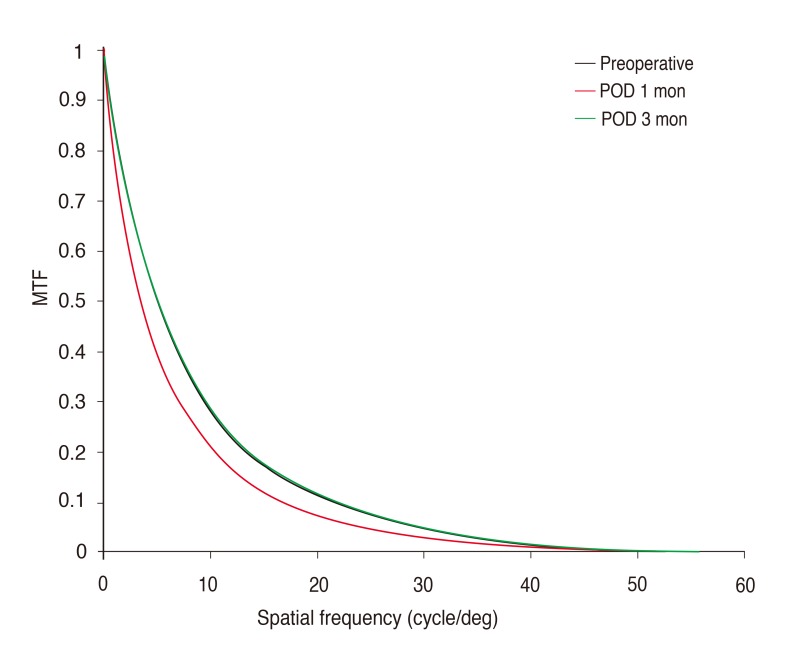
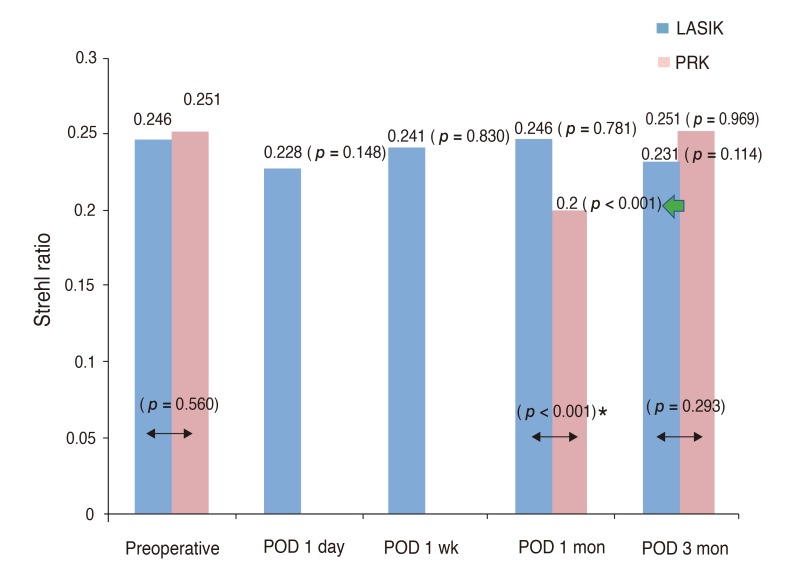
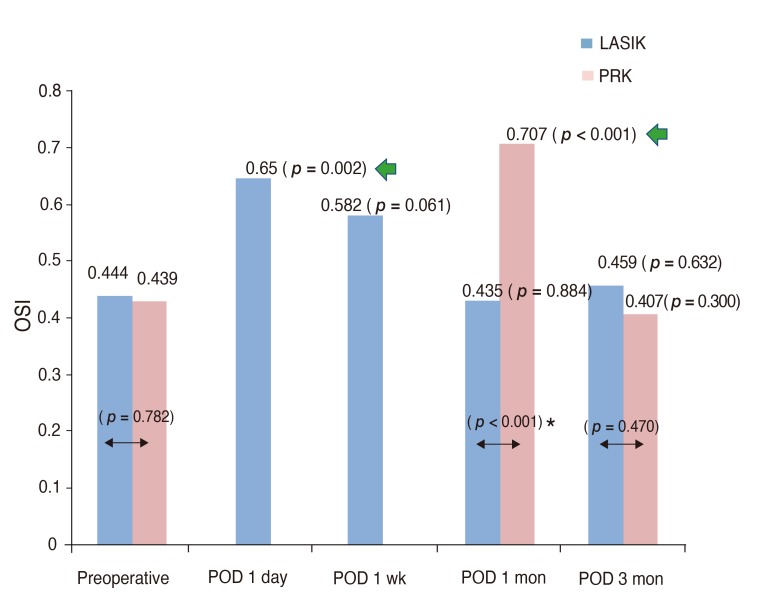
This study measured the visual acuity, manifest refraction and optical quality before and one day, one week, one month, and three months after laser vision correction. Optical quality parameters including the modulation transfer function, Strehl ratio and intraocular scattering were evaluated with a double-pass system.
RESULTS
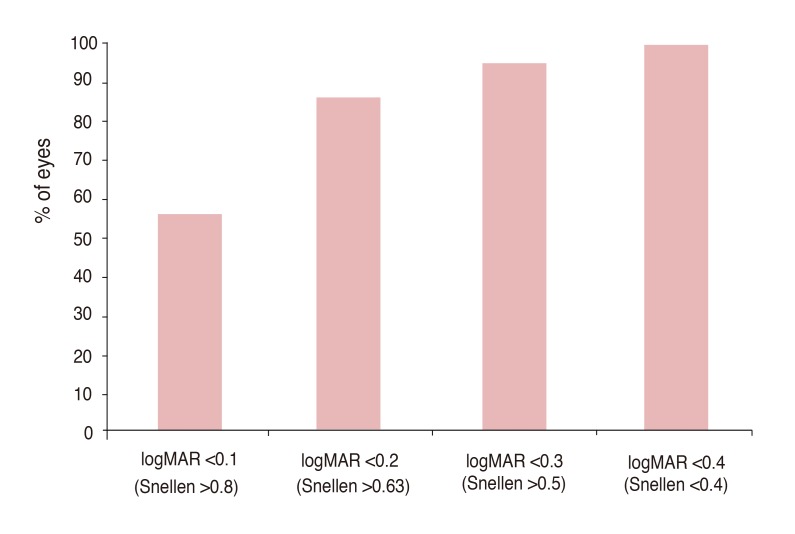
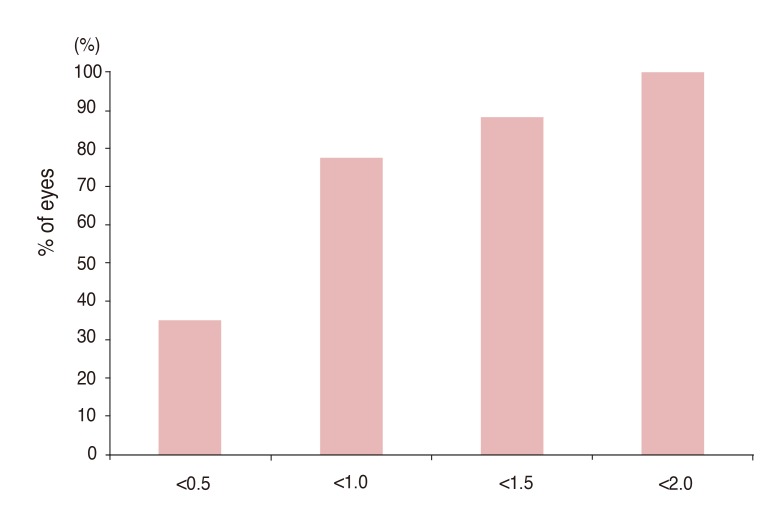
This study included 51 eyes that underwent LASIK and 57 that underwent PRK. The optical quality three months post-surgery did not differ significantly between these laser vision correction techniques. Furthermore, the preoperative and postoperative optical quality did not differ significantly in either group. Optical quality recovered within one week after LASIK but took between one and three months to recover after PRK. The optical quality of patients in the PRK group seemed to recover slightly more slowly than their uncorrected distance visual acuity.
CONCLUSIONS
Optical quality recovers to the preoperative level after laser vision correction, so laser vision correction is efficacious for correcting myopia. The double-pass system is a useful tool for clinical assessment of optical quality.
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Outcome of Small Incision Lenticule Extraction including Visual Quality Analysis
Gi Sung Son, Su Chan Lee, Tae Hyung Lim
J Korean Ophthalmol Soc. 2016;57(4):562-567. doi: 10.3341/jkos.2016.57.4.562.
Reference
-
1. Sugar A, Rapuano CJ, Culbertson WW, et al. Laser in situ keratomileusis for myopia and astigmatism: safety and efficacy: a report by the American Academy of Ophthalmology. Ophthalmology. 2002; 109:175–187. PMID: 11772601.2. Van Gelder RN, Steger-May K, Yang SH, et al. Comparison of photorefractive keratectomy, astigmatic PRK, laser in situ keratomileusis, and astigmatic LASIK in the treatment of myopia. J Cataract Refract Surg. 2002; 28:462–476. PMID: 11973093.
Article3. El Danasoury MA, el Maghraby A, Klyce SD, Mehrez K. Comparison of photorefractive keratectomy with excimer laser in situ keratomileusis in correcting low myopia (from -2.00 to -5.50 diopters): a randomized study. Ophthalmology. 1999; 106:411–420. PMID: 9951500.4. Lee JE, Choi HY, Oum BS, Lee JS. A comparative study for mesopic contrast sensitivity between photorefractive keratectomy and laser in situ keratomileusis. Ophthalmic Surg Lasers Imaging. 2006; 37:298–303. PMID: 16898390.
Article5. Bababeygy SR, Zoumalan CI, Manche EE. Visual outcomes of wavefront-guided laser in situ keratomileusis in eyes with moderate or high myopia and compound myopic astigmatism. J Cataract Refract Surg. 2008; 34:21–27. PMID: 18165076.
Article6. Liang J, Grimm B, Goelz S, Bille JF. Objective measurement of wave aberrations of the human eye with the use of a Hartmann-Shack wave-front sensor. J Opt Soc Am A Opt Image Sci Vis. 1994; 11:1949–1957. PMID: 8071736.
Article7. Prieto PM, Vargas-Martin F, Goelz S, Artal P. Analysis of the performance of the Hartmann-Shack sensor in the human eye. J Opt Soc Am A Opt Image Sci Vis. 2000; 17:1388–1398. PMID: 10935866.
Article8. Schallhorn SC, Farjo AA, Huang D, et al. Wavefront-guided LASIK for the correction of primary myopia and astigmatism a report by the American Academy of Ophthalmology. Ophthalmology. 2008; 115:1249–1261. PMID: 18598819.9. Diaz-Douton F, Benito A, Pujol J, et al. Comparison of the retinal image quality with a Hartmann-Shack wavefront sensor and a double-pass instrument. Invest Ophthalmol Vis Sci. 2006; 47:1710–1716. PMID: 16565413.10. Chen L, Artal P, Gutierrez D, Williams DR. Neural compensation for the best aberration correction. J Vis. 2007; 7:91–9. PMID: 17997678.
Article11. Guirao A, Gonzalez C, Redondo M, et al. Average optical performance of the human eye as a function of age in a normal population. Invest Ophthalmol Vis Sci. 1999; 40:203–213. PMID: 9888445.12. Thibos LN, Hong X, Bradley A, Applegate RA. Accuracy and precision of objective refraction from wavefront aberrations. J Vis. 2004; 4:329–351. PMID: 15134480.
Article13. Guell JL, Pujol J, Arjona M, et al. Optical Quality Analysis System: instrument for objective clinical evaluation of ocular optical quality. J Cataract Refract Surg. 2004; 30:1598–1599. PMID: 15210251.14. Logean E, Dalimier E, Dainty C. Measured double-pass intensity point-spread function after adaptive optics correction of ocular aberrations. Opt Express. 2008; 16:17348–17357. PMID: 18958018.
Article15. Martinez-Roda JA, Vilaseca M, Ondategui JC, et al. Optical quality and intraocular scattering in a healthy young population. Clin Exp Optom. 2011; 94:223–229. PMID: 21083759.16. Saad A, Saab M, Gatinel D. Repeatability of measurements with a double-pass system. J Cataract Refract Surg. 2010; 36:28–33. PMID: 20117702.
Article17. Vilaseca M, Peris E, Pujol J, et al. Intra- and intersession repeatability of a double-pass instrument. Optom Vis Sci. 2010; 87:675–681. PMID: 20581726.
Article18. Ondategui JC, Vilaseca M, Arjona M, et al. Optical quality after myopic photorefractive keratectomy and laser in situ keratomileusis: comparison using a double-pass system. J Cataract Refract Surg. 2012; 38:16–27. PMID: 22153091.
Article19. Ghadhfan F, Al-Rajhi A, Wagoner MD. Laser in situ keratomileusis versus surface ablation: visual outcomes and complications. J Cataract Refract Surg. 2007; 33:2041–2048. PMID: 18053901.
Article20. Miyai T, Miyata K, Nejima R, et al. Comparison of laser in situ keratomileusis and photorefractive keratectomy results: long-term follow-up. J Cataract Refract Surg. 2008; 34:1527–1531. PMID: 18721714.
Article21. Navarro R, Artal P, Williams DR. Modulation transfer of the human eye as a function of retinal eccentricity. J Opt Soc Am A. 1993; 10:201–212. PMID: 8478746.
Article22. Fujikado T, Kuroda T, Maeda N, et al. Light scattering and optical aberrations as objective parameters to predict visual deterioration in eyes with cataracts. J Cataract Refract Surg. 2004; 30:1198–1208. PMID: 15177593.
Article23. Vilaseca M, Padilla A, Ondategui JC, et al. Effect of laser in situ keratomileusis on vision analyzed using preoperative optical quality. J Cataract Refract Surg. 2010; 36:1945–1953. PMID: 21029904.
Article24. Kamiya K, Umeda K, Kobashi H, et al. Effect of aging on optical quality and intraocular scattering using the double-pass instrument. Curr Eye Res. 2012; 37:884–888. PMID: 22587340.
Article25. Pujol J, Gispets J, Arjona M. Optical performance in eyes wearing two multifocal contact lens designs. Ophthalmic Physiol Opt. 2003; 23:347–360. PMID: 12828625.
Article26. Gispets J, Arjona M, Pujol J. Image quality in wearers of a centre distance concentric design bifocal contact lens. Ophthalmic Physiol Opt. 2002; 22:221–233. PMID: 12090637.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Considering Spherical Aberration in Choosing the Wavefront Map for Laser Vision Correction
- Clinical Experience on the Visual Rehabilitation of Low Vision Patients
- Clinical Analysis of 100 Low Vision Patients
- Excimer Laser Refractive Keratectomy: A preliminary Report
- Management of Three Cases of Decentration after Laser In Situ Keratomileusis