Korean J Pediatr Infect Dis.
2014 Apr;21(1):22-28.
Risk Factors Associated with Respiratory Virus Detection in Infants Younger than 90 Days of Age
- Affiliations
-
- 1Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea. ljhped@catholic.ac.kr
Abstract
- PURPOSE
This study aimed at determining the detection rate of respiratory viruses and at investigating the risk factors associated with respiratory virus detection in young infants.
METHODS
From September 2011 to August 2012, nasopharyngeal swabs were obtained from 227 infants aged < or =90 days with suspected infectious diseases, including sepsis. We performed a retrospective analysis of their clinical characteristics. The prevalence of respiratory viruses in their nasopharyngeal swabs was assayed by real-time polymerase chain reaction (real-time PCR).
RESULTS
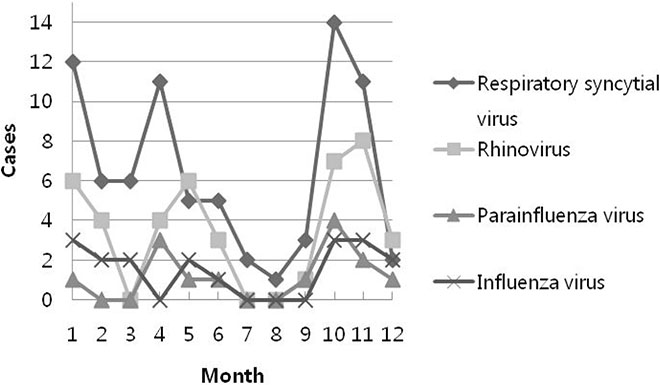
In total, 157 (69.2%) infants had more than one of the following respiratory viruses: respiratory syncytial virus (n=75), rhinovirus (n=42), influenza virus (n=18), parainfluenza virus (n=15), human metapneumovirus (n=9), coronavirus (n=9), adenovirus (n=4), and bocavirus (n=3). During the same period, bacterial infections were confirmed in 24 infants (10.6%). The detection of respiratory viruses was significantly associated with the presence of cough, a family history of respiratory illness, and a seasonal preference (fall/winter). Using logistic regression analysis, these 3 variables were also identified as significant risk factors. During fall and winter, detection of respiratory viruses was significantly higher in infants who did not have a bacterial infection.
CONCLUSION
Respiratory virus is an important pathogen in young infants admitted to a hospital, who are suspected with infectious diseases. Detection of respiratory viruses in young infants was associated with seasonality (fall/winter), presence of respiratory symptoms and a family history of respiratory illness.
Keyword
MeSH Terms
-
Adenoviridae
Bacterial Infections
Bocavirus
Communicable Diseases
Coronavirus
Cough
Humans
Infant*
Logistic Models
Metapneumovirus
Nasopharynx
Orthomyxoviridae
Paramyxoviridae Infections
Prevalence
Real-Time Polymerase Chain Reaction
Respiratory Syncytial Viruses
Respiratory Tract Infections
Retrospective Studies
Rhinovirus
Risk Factors*
Seasons
Sepsis
Virus Diseases
Figure
Reference
-
1. Hall CB, Weinberg GA, Iwane MK, Blumkin AK, Edwards KM, Staat MA, et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med. 2009; 360:588–598.
Article2. Freymuth F, Vabret A, Cuvillon-Nimal D, Simon S, Dina J, Legrand L, et al. Comparison of multiplex PCR assays and conventional techniques for the diagnostic of respiratory virus infections in children admitted to hospital with an acute respiratory illness. J Med Virol. 2006; 78:1498–1504.
Article3. van de Pol AC, Wolfs TF, Jansen NJ, van Loon AM, Rossen JW. Diagnostic value of real-time polymerase chain reaction to detect viruses in young children admitted to the paediatric intensive care unit with lower respiratory tract infection. Crit Care. 2006; 10:R61.4. Ehlken B, Ihorst G, Lippert B, Rohwedder A, Petersen G, Schumacher M, et al. Economic impact of community-acquired and nosocomial lower respiratory tract infections in young children in Germany. Eur J Pediatr. 2005; 164:607–615.
Article5. Brozanski BS, Jones JG, Krohn MJ, Jordan JA. Use of polymerase chain reaction as a diagnostic tool for neonatal sepsis can result in a decrease in use of antibiotics and total neonatal intensive care unit length of stay. J Perinatol. 2006; 26:688–692.
Article6. Wishaupt JO, Russcher A, Smeets LC, Versteegh FG, Hartwig NG. Clinical impact of RT-PCR for pediatric acute respiratory infections: a controlled clinical trial. Pediatrics. 2011; 128:e1113–e1120.
Article7. Monto AS, Ullman BM. Acute respiratory illness in an American community: the Tecumseh study. JAMA. 1974; 227:164–169.
Article8. Tregoning JS, Schwarze J. Respiratory viral infections in infants: causes, clinical symptoms, virology, and immunology. Clin Microbiol Rev. 2010; 23:74–98.
Article9. Aberle JH, Aberle SW, Pracher E, Hutter HP, Kundi M, Popow-Kraupp T. Single versus dual respiratory virus infections in hospitalized infants: impact on clinical course of disease and Interferon-γ response. Pediatr Infect Dis J. 2005; 24:605–610.
Article10. van Piggelen RO, van Loon AM, Krediet TG, Verboon-Maciolek MA. Human rhinovirus causes severe infection in preterm infants. Pediatr Infect Dis J. 2010; 29:364–365.
Article11. Simoes EA. Environmental and demographic risk factors for respiratory syncytial virus lower respiratory tract disease. J Pediatr. 2003; 143:S118–S126.
Article12. Jansen RR, Wieringa J, Koekkoek SM, Visser CE, Pajkrt D, Molenkamp R, et al. Frequent detection of respiratory viruses without symptoms: toward defining clinically relevant cutoff values. J Clin Microbiol. 2011; 49:2631–2636.
Article13. Smit PM, Pronk SM, Kaandorp JC, Weijer O, Lauw FN, Smits PH, et al. RT-PCR detection of respiratory pathogens in newborn children admitted to a neonatal medium care unit. Pediatr Res. 2013; 73:355–361.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors associated with obesity of acute bronchiolitis in infants: association of obesity with disease severity
- Associated Factors with Respiratory Virus Detection in Newborn with Suspected Infection
- Clinical considerations of febrile infants with respiratory symptoms according to the respiratory viral detection
- Association of Respiratory Viral Infection and Atopy with Severity of Acute Bronchiolitis in Infants
- Incidence and Risk Factors of Rehospitalization with Respiratory Syncytial Virus Infection in Premature Infants