Cancer Res Treat.
2005 Apr;37(2):109-113.
Outcome and Prognostic Factors of Childhood Diffuse Brainstem Glioma
- Affiliations
-
- 1Department of Radiation Oncology, Konkuk University College of Medicine, Korea.
- 2Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea. ihkim@snu.ac.kr
- 3Institute of Radiation Medicine, Medical Research Center, Seoul National University College of Medicine, Seoul, Korea.
- 4Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea.
Abstract
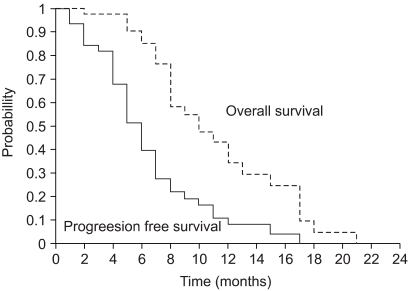
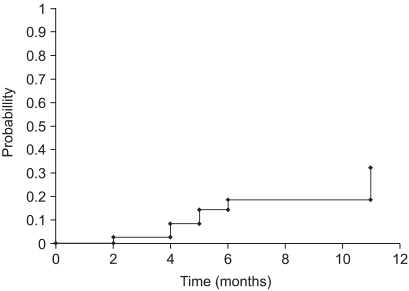
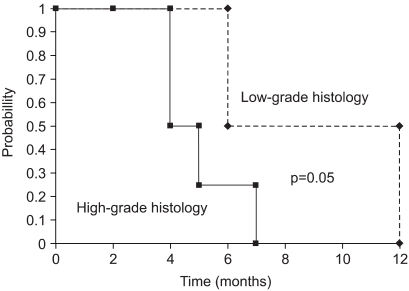
- PURPOSE
The outcome and prognostic factors of brainstem glioma were evaluated following radiotherapy methods. MATERIALS AND METHODS: Between 1986 and 2001, 45 childhood patients with diffuse brainstem glioma were treated. There were 26 boys and 19 girls, with a median age of 7 years (range 3~18). The histopathological diagnoses were confirmed in 13 patients, which revealed a low-grade glioma in four patients, and high-grade glioma in the other nine. Before 1993, radiation therapy using a regime of 1.8 to 2.0 Gy once a day was performed in 16 cases; thereafter, a regimes of 1.1 or 1.5 Gy twice a day was given in 15 and 14 cases, respectively. Nine patients were treated with adjuvant chemotherapy. The response to the treatment was evaluated by the MRI findings 4 weeks after radiotherapy. RESULTS: After radiotherapy, the neurological deficit improved in 42 of the 45 patients (93%). The MRI responses were as follows; partial response 22/39 (56%), minimal to no response in 16/39 (41%) and tumor progression in 1/39 (3%). The median time to disease progression was 7 months, and the median survival was 12 months; the overall survival rate at 1 year was 41%. There was no significant prognostic factor for overall survival. The progression-free survival was influenced by the tumor histology (low grade vs. high grade, p=0.05) in those patients whose pathology was confirmed. CONCLUSION: The radiation therapy fractionation schedule did not influence the survival. Low grade histology was a possible favorable prognostic factor of progression-free survival in pediatric brainstem glioma patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Reigel DH, Scarff TB, Woodford JE. Biopsy of pediatric brainstem tumors. Childs Brain. 1979; 5:329–340. PMID: 456107.2. Zimmerman RA. Neuroimaging of pediatric brain stem diseases other than brain stem glioma. Pediatr Neurosurg. 1996; 25:83–92. PMID: 9075252.
Article3. Freeman CR, Krischer JP, Sanford RA, Cohen ME, Burger PC, del Carpio R, et al. Final results of a study of escalating doses of hyperfractionated radiotherapy in brain-stem tumors in children: a Pediatric Oncology Group study. Int J Radiat Oncol Biol Phys. 1993; 27:197–206. PMID: 8407392.4. Kaplan AM, Albright AL, Zimmerman RA, Rorke LB, Li H, Boyett JM, et al. Brainstem gliomas in children. A Children's Cancer Croup review of 119 cases. Pediatr Neurosurg. 1996; 24:185–192. PMID: 8873160.5. Mandell LR, Kadota R, Freeman C, Douglass EC, Fontanesi J, Cohen ME, et al. There is no role for hyperfractionated radiotherapy in the management of children with newly diagnosed diffuse intrinsic brainstem tumors: results of a Pediatric Oncology Group phase III trial comparing conventional vs. hyperfractionated radiotherapy. Int J Radiat Oncol Biol Phys. 1999; 43:959–964. PMID: 10192340.
Article6. Chuba PJ, Zamarano L, Hamre M, Bhambhani K, Canady A, Guys MB, et al. Permanent I-125 brain stem implants in children. Childs Nerv Syst. 1998; 14:570–577. PMID: 9840381.
Article7. Kretschmar CS, Tarbell NJ, Barnes PD, Krischer JP, Burger PC, Kun L. Pre-irradiation chemotherapy and hyperfractionated radiation therapy 66 Gy for children with brain stem tumors. A phase II study of the Pediatric Oncology Group, Protocol 8833. Cancer. 1993; 72:1404–1413. PMID: 8339231.
Article8. Kedar A, Maria BL, Graham-Pole J, Ringdahl DM, Quisling RG, Mickle JP, et al. High-dose chemotherapy with marrow reinfusion and hyperfractionated irradiation for children with high-risk brain tumors. Med Pediatr Oncol. 1994; 23:428–436. PMID: 8084310.
Article9. Bouffet E, Khelfaoui F, Philip I, Biron P, Brunat-Mentigny M, Philip T. High-dose carmustine for high-grade gliomas in childhood. Cancer Chemother Pharmacol. 1997; 39:376–379. PMID: 9025780.
Article10. Dunkel IJ, Garvin JH Jr, Goldman S, Ettinger LJ, Kaplan AM, Cairo M, et al. Childrens Cancer Group. High dose chemotherapy with autologous bone marrow rescue for children with diffuse pontine brain stem tumors. J Neurooncol. 1998; 37:67–73. PMID: 9525840.11. Broniscer A, Leite CC, Lanchote VL, Machado TM, Cristofani LM. Brainstem Glioma Cooperative Group. Radiation therapy and high-dose tamoxifen in the treatment of patients with diffuse brainstem gliomas: results of a Brazilian cooperative study. J Clin Oncol. 2000; 18:1246–1253. PMID: 10715294.
Article12. Kaplan E, Meier P. Nonparametricestimation from incomplete observations. J Am Stat Assoc. 1958; 53:457–481.13. Mantel N, Haenszel W. Chi-square test with one degree of freedom: extension of the Mantel-Haenszel procedure. J Am Stat Soc. 1963; 58:690–700.14. Thames HD Jr, Withers HR, Peters LJ, Fletcher GH. Changes in early and late radiation responses with altered dose fractionation: implications for dose-survival relationshils. Int J Radiat Oncol Biol Phys. 1982; 8:219–226. PMID: 7085377.15. Mantravadi RV, Phatak R, Bellur S, Liebner EJ, Haas R. Brain stem gliomas: an autopsy study of 25 cases. Cancer. 1982; 49:1294–1296. PMID: 6277461.
Article16. Walker MD, Strike TA, Sheline GE. An analysis of dose effect relationship in the radiotherapy of malignant gliomas. Int J Radiat Oncol Biol Phys. 1979; 5:1725–1731. PMID: 231022.17. Packer RJ, Boyett JM, Zimmerman RA, Rorke LB, Kaplan AM, Albright AL, et al. A Childrens Cancer Group Phase I/II Trial. Hyperfractionated radiation therapy (72Gy) for children with brain stem gliomas. Cancer. 1993; 72:1414–1421. PMID: 8339232.18. Albright AL, Guthkelch AN, Parker RJ, Price RA, Rourke LB. Prognostic factors in pediatric brain stem gliomas. J Neurosurg. 1986; 65:751–755. PMID: 3772472.19. Cartmill M, Punt J. Diffuse brain stem glioma: a review of stereotactic biopsies. Childs Nerv Syst. 1999; 15:235–237. PMID: 10392494.20. Galanis E, Buckner JC. Chemotherapy of brain tumors. Curr Opin Neurol. 2000; 13:619–625. PMID: 11148660.
Article21. Gilbertson RJ, Hill DA, Hernan R, Kocak M, Geyer R, Olson J, et al. ERBB1 is amplified and overexpressed in high grade diffusely infiltrative pediatric brain stem glioma. Clin Cancer Res. 2003; 9:3620–3624. PMID: 14506149.22. Daw NC, Furman WL, Stewart CF, Hawkins DR, Houghton PJ, et al. A phase I trial and pharmacokinetic study of gefitinib in pediatric patients with refractory solid tumors: a Children's Oncology Group Study. J Clin Oncol. 2004; 22(14S):8522.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical observation on brainstem glioma in childhood
- Brainstem Gliomas: Classification, Growth Patterns, and Prognosis
- Combined Treatment With Radiotherapy and Immunotherapy for Isocitrate Dehydrogenase Mutant Brainstem Glioma in Adult: A Case Report
- Spontaneous Regression of Glioma–Mimicking Brainstem Lesion in a Child: A Case Report
- Overview of CNS Gliomas in Childhood