Hanyang Med Rev.
2009 Aug;29(3):245-254. 10.7599/hmr.2009.29.3.245.
Surgical Management of Sinonasal Cancer
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Ilsong Memorial Institute of Head and Neck Cancer, Hallym University Medical Center, Seoul, Korea. ys20805@chol.com
- KMID: 1505101
- DOI: http://doi.org/10.7599/hmr.2009.29.3.245
Abstract
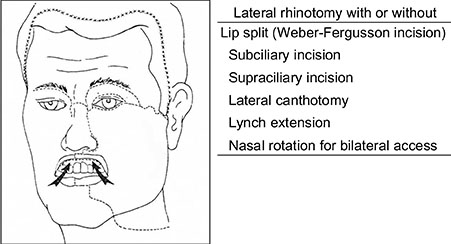
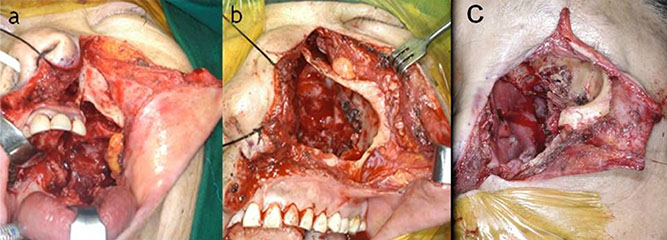
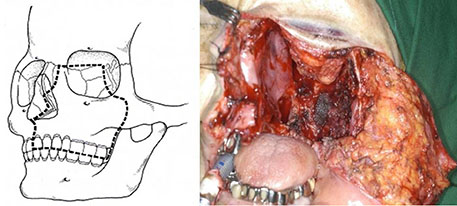
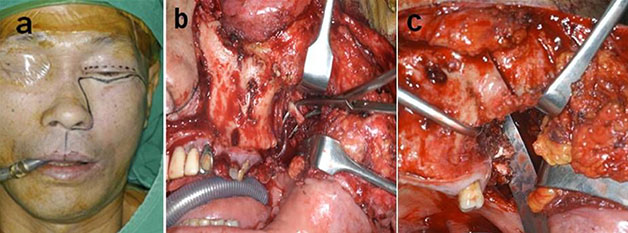
- Sinonasal cancers account for less than 1% of all malignancies and comprise 3% of all head and neck malignancies. The most common malignant neoplasm in the sinuses and nose is squamous cell carcinoma, which accounts for 70% of these neoplasms. Most of these arise in the maxillary antrum, and only 10% to 30% occur in the nasal cavity or ethmoid sinus. It is well known the surgery is primary treatment for sinonasal malignancies. Adjunctive irradiation and/or chemoradiatioin has resulted in improved locoregional control and increased survival rates. The goal of surgical resection is to remove the cancer en bloc, with clear margin devoid of neoplastic cells. For maxillary sinus neoplasms, maxillectomy is a standard surgical procedure. Neoplasms involving the ethmoid, frontal, or sphenoid sinuses may require a craniofacial approach because of frequent invasion into the skull base. The proximity of the nasal cavity and paranasal sinuses to the adjacent structures including the orbit, dura, brain, cranial nerves, and carotid arteries mandates careful radiologic and neurologic evaluations throughout the course of the disease. Surgical advances now permit complex tumor removal and reconstruction surrounding these structures resulting in functional and cosmetic improvements when compared to earlier techniques.
Keyword
MeSH Terms
Figure
Reference
-
1. Resto VA, Deschler DG. Sinonasal malignancies. Otolaryngol Clin North Am. 2004; 37:473–487.
Article2. Dulguerov P, Jacobsen MS, Allal AS. Nasal and paranasal sinus carcinoma: are we making progress? A series of 220 patients and a systematic review. Cancer. 2001; 92:3012–3029.
Article3. Lee MM, Vokes EE, Rosen A. Multimodality therapy in advanced paranasal sinus carcinoma: superior long-term results. Cancer J Sci Am. 1999; 5:219–223.
Article4. Jho HD, Ha HG. Endoscopic endonasal skull-base surgery: part 1-the midline anterior fossa skull base. Minim Invasive Neurosurg. 2004; 47:1–8.
Article5. Jho HD, Ha HG. Endoscopic endonasal skull-base surgery: part 2-the cavernous sinus. Minim Invasive Neurosurg. 2004; 47:9–15.6. Lund VJ, Howard DJ, Wei WI, Cheesman AD. Craniofacial resection for tumors of the nasal cavity and paranasal sinuses. A 17-year experience. Head Neck. 1998; 20:97–105.
Article7. Roh HJ, Moon YI. Endoscopic Surgery for Sinonasal tumor. J Clin Otolaryngol Head Neck Surg. 2002; 13:165–171.
Article8. Batra PS, Citardi MJ. Endoscopic management of sinonasal malignancy. Otolaryngol Clin North Am. 2006; 39:619–637.
Article9. Sisson GA. Symposium III. Treatment of malignancies of paranasal sinuses : Discussion and summary. Laryngoscope. 1970; 80:945–953.10. Carrau RL, Segas J, Nuss DW. Squamous cell carcinoma of the sinonasal tract invading the orbit. Laryngoscope. 1999; 109:230–235.
Article11. Ji YB, Song MN, Sung YS, Lee YS, Kim KB, Tae K. The significance of orbital preservation in surgery of the sinonasal malignancies. Korean J Otorhinolaryngol-Head Neck Surg. 2009; 52:349–353.
Article12. Raveh J, Turk JB, Ladrach K. Extended anterior subcranial approach for skull base tumors: long-term results. J Neurosurg. 1995; 82:1002–1010.
Article13. Moore CE, Ross DA, Marentette LJ. Subcranial approach to tumors of the anterior cranial base: analysis of current and traditional surgical techniques. Otolaryngol Head Neck Surg. 1999; 120:387–390.
Article14. Ganly I, Patel SG, Singh B. Craniofacial resection for malignant paranasal sinus tumors: report of an international collaborative study. Head Neck. 2005; 27:575–584.
Article15. Suarez C, Llorente JL, Fernandez de Leon R, Maseda E. Prognostic factors in sinonasal tumors involving the anterior skull base. Head Neck. 2004; 26:136–144.
Article16. Day TA, Davis BK. Skull-base reconstruction and rehabilitation. Otolaryngol Clin North Am. 2001; 34:1241–1257.17. Le QT, Fu KF, Kaplan MJ. Lymph node metastasis in maxillary sinus carcinoma. Int J Radiat Oncol Biol Phys. 2000; 46:541–549.
Article18. Kim GE, Chung EJ, Lim JJ. Clinical significance of neck node metastasis in squamous cell carcinoma of the maxillary antrum. Am J Otolaryngol. 1999; 20:383–390.
Article19. Cordeiro PG, Disa JJ. Challenges in midface reconstruction. Semin Surg Oncol. 2000; 19:218–225.
Article20. Carrillo JF, Guemes A, Ramirez-Ortega MC, Onate-Ocana LF. Prognostic factors in maxillary sinus and nasal cavity carcinoma. Eur J Surg Oncol. 2005; 31:1206–1212.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical outcomes of endoscopic versus open resection for the management of sinonasal malignancies
- Inverted Papilloma of the Sinonasal Cavity: The Surgical Strategy of Endoscopic Management Based on the Site of Attachment
- Management of Paranasal Sinusitis in the Patient with Transplantation
- Sinonasal Undifferentiated Pleomorphic Sarcoma in Five Patient Cases
- Long-Term Treatment Outcomes in Endoscopic Management of Sinonasal Benign Tumors