Yonsei Med J.
2013 Mar;54(2):336-344. 10.3349/ymj.2013.54.2.336.
Early Differential Changes in Coronary Plaque Composition According to Plaque Stability Following Statin Initiation in Acute Coronary Syndrome: Classification and Analysis by Intravascular Ultrasound-Virtual Histology
- Affiliations
-
- 1Department of Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. sglee@uuh.ulsan.kr
- KMID: 1503894
- DOI: http://doi.org/10.3349/ymj.2013.54.2.336
Abstract
- PURPOSE
The aim of this study was to demonstrate the early effects of statin treatment on plaque composition according to plaque stability on Intravascular Ultrasound-Virtual Histology at 6 months after a coronary event. Previous trials have demonstrated that lipid lowering therapy with statins decreases plaque volume and increases plaque echogenicity in patients with coronary artery disease.
MATERIALS AND METHODS
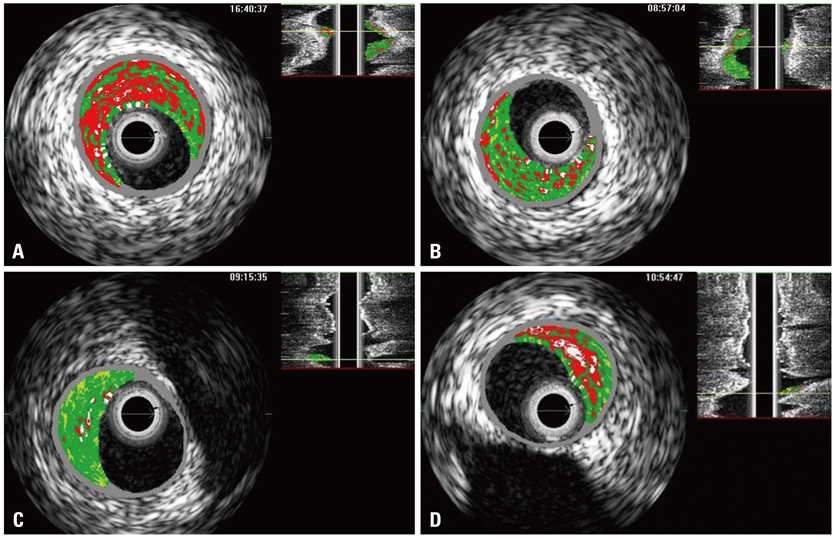
Fifty-four patients (54 lesions) with acute coronary syndrome were prospectively enrolled. We classified and analyzed the target plaques into two types according to plaque stability: thin-cap fibroatheroma (TCFA, n=14) and non-TCFA (n=40). The primary end point was change in percent necrotic core in the 10-mm subsegment with the most disease.
RESULTS
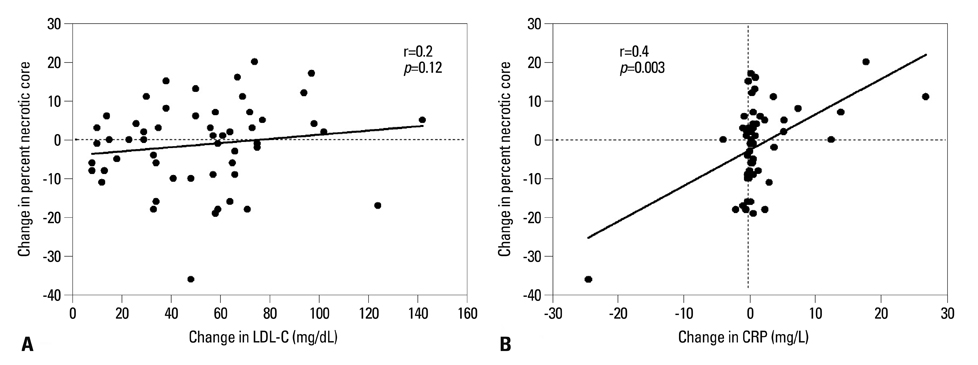
After 6 months of statin therapy, no change was demonstrated in the mean percentage of necrotic core (18.7+/-8.5% to 20.0+/-11.0%, p=0.38). There was a significant reduction in necrotic core percentage in patients with TCFA (21.3+/-7.2% to 14.4+/-8.9%, p=0.017), but not in patients with non-TCFA. Moreover, change in percent necrotic core was significantly correlated with change in high-sensitivity C-reactive protein levels (r=0.4, p=0.003). Changes in low-density lipoprotein cholesterol levels and lipid core percentage demonstrated no significant associations.
CONCLUSION
A clear reduction of lipid core was observed only for the TCFA plaque type, suggesting that changes in plaque composition following statin therapy might occur earlier in vulnerable plaque than in stable plaque; the effect may be related to the anti-inflammatory effects of statins.
Keyword
MeSH Terms
-
Acute Coronary Syndrome/*drug therapy/ultrasonography
Aged
C-Reactive Protein/metabolism
Female
Humans
Hydroxymethylglutaryl-CoA Reductase Inhibitors/*therapeutic use
Male
Middle Aged
Plaque, Atherosclerotic/*ultrasonography
Ultrasonography, Interventional
Hydroxymethylglutaryl-CoA Reductase Inhibitors
C-Reactive Protein
Figure
Reference
-
1. Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 2000. 20:1262–1275.2. Davies MJ, Richardson PD, Woolf N, Katz DR, Mann J. Risk of thrombosis in human atherosclerotic plaques: role of extracellular lipid, macrophage, and smooth muscle cell content. Br Heart J. 1993. 69:377–381.
Article3. Nair A, Kuban BD, Tuzcu EM, Schoenhagen P, Nissen SE, Vince DG. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation. 2002. 106:2200–2206.
Article4. Rodriguez-Granillo GA, García-García HM, Mc Fadden EP, Valgimigli M, Aoki J, de Feyter P, et al. In vivo intravascular ultrasound-derived thin-cap fibroatheroma detection using ultrasound radiofrequency data analysis. J Am Coll Cardiol. 2005. 46:2038–2042.
Article5. Nasu K, Tsuchikane E, Katoh O, Vince DG, Virmani R, Surmely JF, et al. Accuracy of in vivo coronary plaque morphology assessment: a validation study of in vivo virtual histology compared with in vitro histopathology. J Am Coll Cardiol. 2006. 47:2405–2412.6. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994. 344:1383–1389.7. Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002. 360:7–22.8. FRagmin and Fast Revascularisation during InStability in Coronary artery disease Investigators. Invasive compared with non-invasive treatment in unstable coronary-artery disease: FRISC II prospective randomised multicentre study. Lancet. 1999. 354:708–715.9. Schwartz GG, Olsson AG, Ezekowitz MD, Ganz P, Oliver MF, Waters D, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. JAMA. 2001. 285:1711–1718.
Article10. Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004. 350:1495–1504.
Article11. Okazaki S, Yokoyama T, Miyauchi K, Shimada K, Kurata T, Sato H, et al. Early statin treatment in patients with acute coronary syndrome: demonstration of the beneficial effect on atherosclerotic lesions by serial volumetric intravascular ultrasound analysis during half a year after coronary event: the ESTABLISH Study. Circulation. 2004. 110:1061–1068.
Article12. Goldstein JA, Demetriou D, Grines CL, Pica M, Shoukfeh M, O'Neill WW. Multiple complex coronary plaques in patients with acute myocardial infarction. N Engl J Med. 2000. 343:915–922.
Article13. Lee SG, Lee CW, Hong MK, Kim JJ, Park SW, Park SJ. Change of multiple complex coronary plaques in patients with acute myocardial infarction: a study with coronary angiography. Am Heart J. 2004. 147:281–286.
Article14. Ridker PM, Cannon CP, Morrow D, Rifai N, Rose LM, McCabe CH, et al. C-reactive protein levels and outcomes after statin therapy. N Engl J Med. 2005. 352:20–28.
Article15. Newby LK, Kristinsson A, Bhapkar MV, Aylward PE, Dimas AP, Klein WW, et al. Early statin initiation and outcomes in patients with acute coronary syndromes. JAMA. 2002. 287:3087–3095.
Article16. Nissen SE, Tuzcu EM, Schoenhagen P, Brown BG, Ganz P, Vogel RA, et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA. 2004. 291:1071–1080.
Article17. Nissen SE, Nicholls SJ, Sipahi I, Libby P, Raichlen JS, Ballantyne CM, et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA. 2006. 295:1556–1565.
Article18. Schartl M, Bocksch W, Koschyk DH, Voelker W, Karsch KR, Kreuzer J, et al. Use of intravascular ultrasound to compare effects of different strategies of lipid-lowering therapy on plaque volume and composition in patients with coronary artery disease. Circulation. 2001. 104:387–392.
Article19. Kawasaki M, Sano K, Okubo M, Yokoyama H, Ito Y, Murata I, et al. Volumetric quantitative analysis of tissue characteristics of coronary plaques after statin therapy using three-dimensional integrated backscatter intravascular ultrasound. J Am Coll Cardiol. 2005. 45:1946–1953.
Article20. Armstrong ML, Megan MB. Arterial fibrous proteins in cynomolgus monkeys after atherogenic and regression diets. Circ Res. 1975. 36:256–261.
Article21. Aikawa M, Rabkin E, Okada Y, Voglic SJ, Clinton SK, Brinckerhoff CE, et al. Lipid lowering by diet reduces matrix metalloproteinase activity and increases collagen content of rabbit atheroma: a potential mechanism of lesion stabilization. Circulation. 1998. 97:2433–2444.
Article22. Schoenhagen P, Tuzcu EM, Apperson-Hansen C, Wang C, Wolski K, Lin S, et al. Determinants of arterial wall remodeling during lipid-lowering therapy: serial intravascular ultrasound observations from the Reversal of Atherosclerosis with Aggressive Lipid Lowering Therapy (REVERSAL) trial. Circulation. 2006. 113:2826–2834.
Article23. Sawada T, Shite J, Garcia-Garcia HM, Shinke T, Watanabe S, Otake H, et al. Feasibility of combined use of intravascular ultrasound radiofrequency data analysis and optical coherence tomography for detecting thin-cap fibroatheroma. Eur Heart J. 2008. 29:1136–1146.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Statin Therapy with Coronary Plaque Imaging
- Acute coronary syndrome and vulnerable plaque
- Plaque Morphology in Acute Coronary Syndrome: An Intravascular Ultrasound Study
- Practical Application of Coronary Imaging Devices in Cardiovascular Intervention
- Lesion Characteristics in Patients with Acute Coronary Syndrome: A Comparison with Lesion in Patients with Stable Angina by Intravascular Ultrasound