J Korean Acad Nurs.
2012 Dec;42(6):783-790. 10.4040/jkan.2012.42.6.783.
Effects of Passive Upper Arm Exercise on Range of Motion, Muscle Strength, and Muscle Spasticity in Hemiplegic Patients with Cerebral Vascular Disease
- Affiliations
-
- 1Chungnam National University Hospital, Daejeon, Korea.
- 2College of Nursing, Chungnam National University, Daejeon, Korea. songry@cnu.ac.kr
- KMID: 1499505
- DOI: http://doi.org/10.4040/jkan.2012.42.6.783
Abstract
- PURPOSE
The purpose of this study was to investigate the effects of passive upper arm exercise on range of motion, muscle strength, and muscle spasticity in hemiplegic patients with cerebral vascular disease.
METHODS
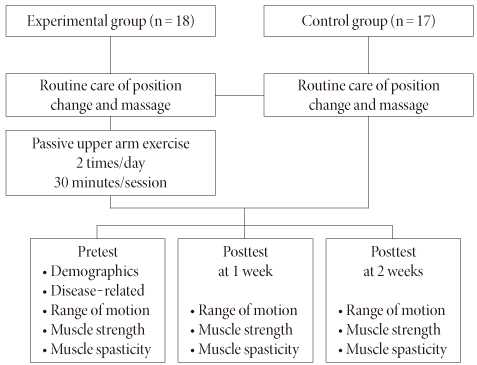
A quasi-experimental design with nonequivalent control group was utilized. According to inclusion criteria, 25 patients were assigned to the control group with routine care, followed by 25 to the intervention group with passive exercise for 30 minutes per session, twice a day for 2 weeks. Eighteen patients in the intervention group and 17 in the control group completed the posttest measurement, including range of motion for upper arm joints, manual muscle test, and Modified Ashworth Scale for muscle spasticity.
RESULTS
The intervention group had a significantly improved range of motion in the shoulder and wrist joints. No interaction effect was found for the elbow joint. No significant differences were found in muscle strength or muscle spasticity between the groups.
CONCLUSION
Results of the study indicate that passive exercise safely applied for two weeks improves range of motion in joints of the upper arm in these patients. Further study with long-term follow-up is needed to verify the role of passive exercise in preventing muscle spasticity in this population.
MeSH Terms
Figure
Reference
-
1. Bohannon RW, Smith MB. Interrater reliability of a Modified Ashworth Scale of muscle spasticity. Phys Ther. 1987. 67:206–207.2. Butler A, Blanton S, Rowe V, Wolf S. Attempting to improve function and quality of life using the FTM protocol: Case report. J Neurol Phys Ther. 2006. 30(3):148–156.3. Choi SH, Lee JC, Bae JJ. The effect of complex rehabilitation exercise program on hemodynamics, functional fitness and lower extremity isokinetic strength in hemiplegia. J Adapt Phys Act Exerc. 2010. 18(3):127–138.4. Erdfelder E, Faul F, Buchner A. GPOWER: A general power analysis program. Behav Res Methods Instrum Comput. 1996. 28:1–11. http://dx.doi.org/10.3758/BF03203630.5. Hendricks HT, van Limbeek J, Geurts AC, Zwarts MJ. Motor recovery after stroke: A systematic review of the literature. Arch Phys Med Rehabil. 2002. 83:1629–1637. http://dx.doi.org/10.1053/apmr.2002.35473.6. Hislop HJ, Montgomery J, Connelly B, Daniels L. Daniels and Worthingham's muscle testing: Techniques of manual examination. 1995. 6th ed. St Louis, MO: Saunders.7. Kim HJ. Effects of bilateral passive range of motion exercise on the function of upper extremities and ADL's in patients with acute stroke. 2009. Seoul: The Catholic University of Korea;Unpublished doctoral dissertation.8. Kim KS, Kang JY. Upper extremity exercise training effects on motor activity, ADL and health related QOL of hemiplegic patients. Korean J Rehabil Nurs. 2002. 5(2):134–144.9. Kim TH, Lee DY, Kim NJ, Song CH. Predicting activities of daily living by the motor assessment in subacute hemiplegia. J Korea Sport Res. 2006. 17(6):331–340.10. Kim WH, Hwang MO, Park EY. The effect of physical occupational therapy on activities of daily living in stroke inpatients at least 3 months after stroke. J Korean Acad Univ Trained Phys Ther. 2007. 14(1):74–81.11. Korean Statistical Information Service. Statistical database on health. 2011. Retrieved December 30, 2011. from http://kosis.kr/abroad/abroad_01List.jsp.12. Lynch D, Ferraro M, Krol J, Trudell CM, Christos P, Volpe BT. Continuous passive motion improves shoulder joint integrity following stroke. Clin Rehabil. 2005. 19:594–599. http://dx.doi.org/10.1191/0269215505cr901oa.13. Mangold S, Schuster C, Keller T, Zimmermann-Schlatter A, Ettlin T. Motor training of upper extremity with functional electrical stimulation in early stroke rehabilitation. Neurorehabil Neural Repair. 2009. 23:184–190. http://dx.doi.org/10.1177/1545968308324548.14. Pandyan AD, Johnson GR, Price CI, Curless RH, Barnes MP, Rodgers H. A review of the properties and limitations of the Ashworth and modified Ashworth scales as measures of spasticity. Clin Rehabil. 1999. 13(5):373–383. http://dx.doi.org/10.1191/026921599677595404.15. So HY, Cho BH, Seo YO. Rehabilitation nursing. 2007. Seoul: Hyunmoonsa.16. Trombly CA, Radomski MV. Occupational therapy for physical dysfunction. 2002. 5th ed. Baltimore: Lippincott.17. Tseng CN, Chen CC, Wu SC, Lin LC. Effect of a range of motion exercise programme. J Adv Nurs. 2007. 57(2):181–191. http://dx.doi.org/10.1111/j.1365-2648.2006.04078.x.18. Yang EJ, Kim HJ, Ahn HS, Lee EH. The effect of early upper extremities passive exercise on the hand edema and upper spasticity of the hemiplegia patient after stroke. Clin Nurs Res. 2006. 12(1):147–157.19. Yoon CG. Adult hemiplegia: Evaluation and treatment. 2010. 2nd ed. Seoul: Hyunmoonsa.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Passive Leg Range of Motion Exercise in Hemiplegic Patients
- Effects of Biofeedback Exercise Training in Hemiplegic Patients after Stroke
- The Effects of Electrical Stimulation on Upper Extremity Spasticity in Hemiplegic Patients
- The Immediate Effect of Wrist Joint Mobilization with Taping on Range of Motion, Grip Strength, Spasticity in Stroke Patients
- Botulinum Toxin A Injection into the Subscapularis Muscle to Treat Intractable Hemiplegic Shoulder Pain