Korean J Physiol Pharmacol.
2008 Oct;12(5):259-265. 10.4196/kjpp.2008.12.5.259.
PKC-Independent Stimulation of Cardiac Na+/Ca2+ Exchanger by Staurosporine
- Affiliations
-
- 1Department of Physiology, SBRI, Sungkyunkwan University School of Medicine, Suwon, Korea. tmkang@yurim.skku.ac.kr
- KMID: 1486108
- DOI: http://doi.org/10.4196/kjpp.2008.12.5.259
Abstract
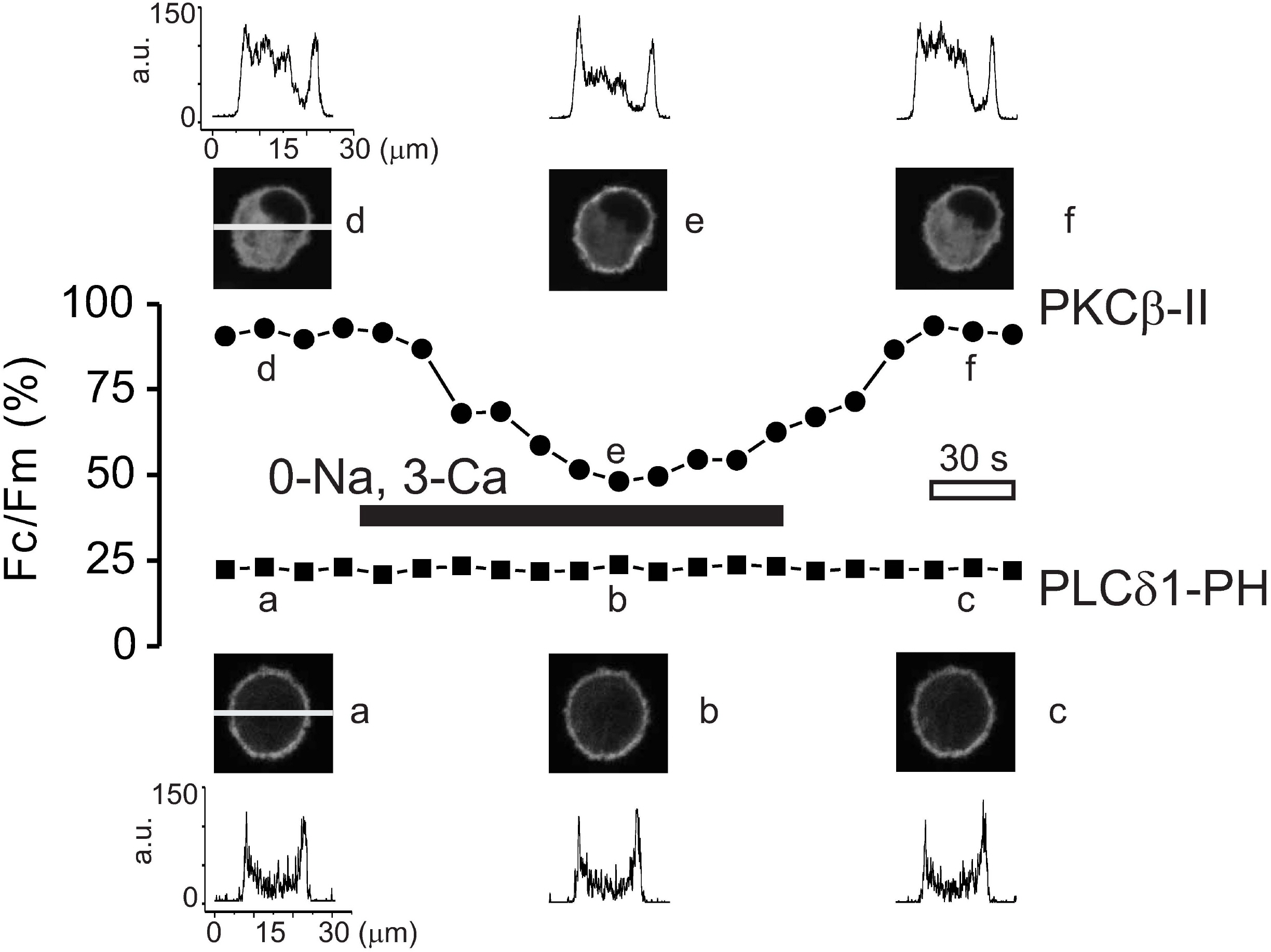
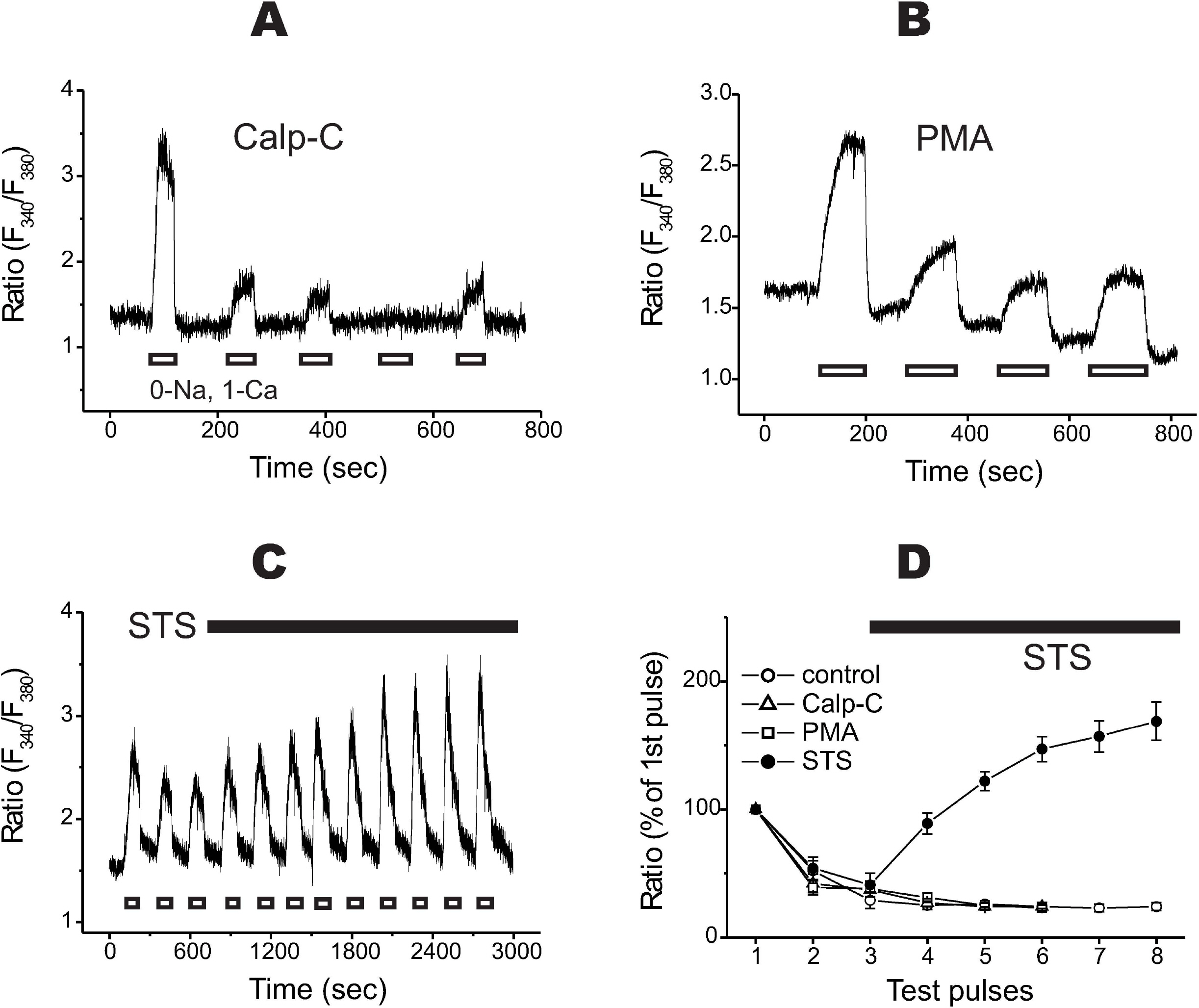
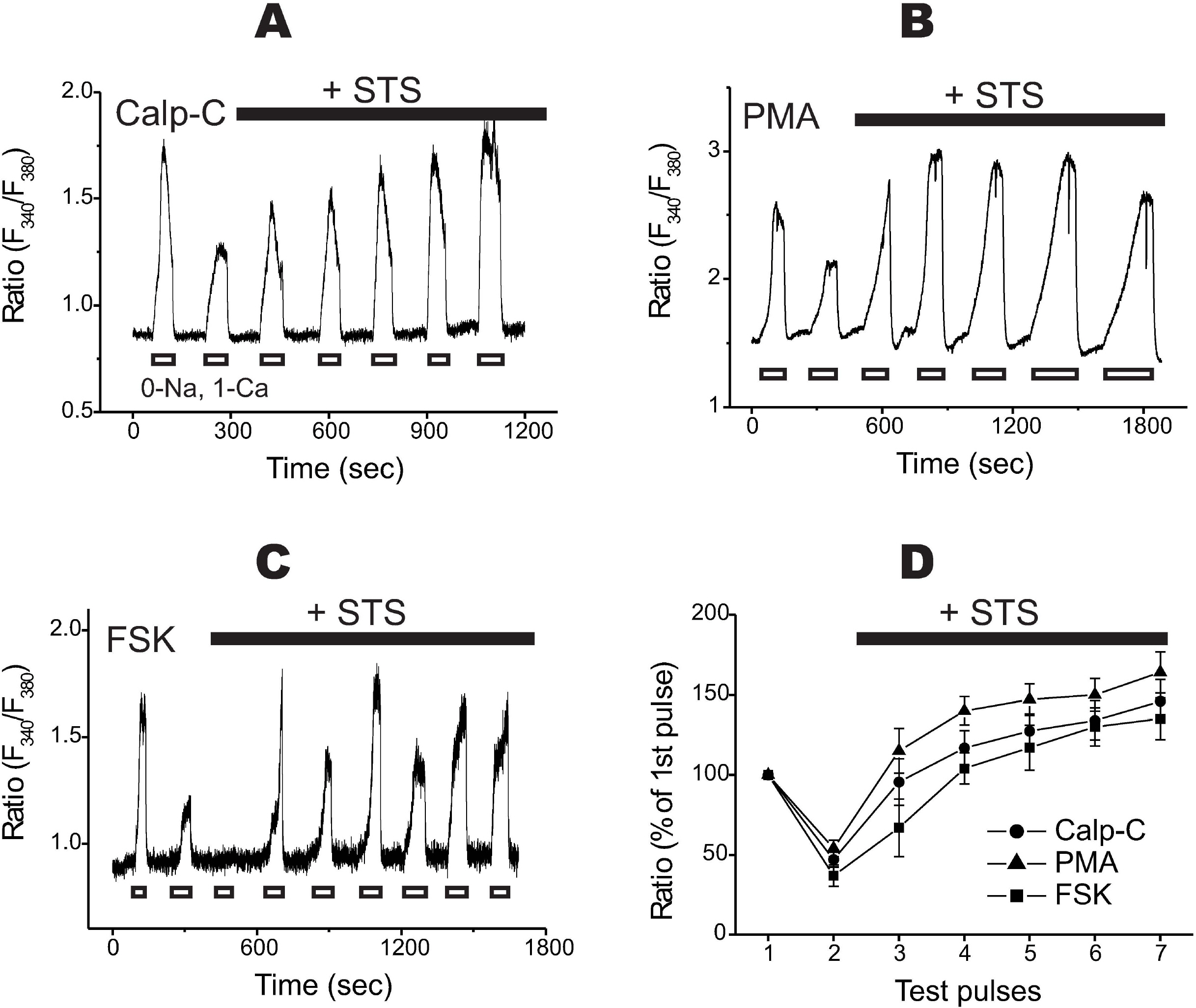
- [Ca2+]i transients by reverse mode of cardiac Na+/Ca2+ exchanger (NCX1) were recorded in fura-2 loaded BHK cells with stable expression of NCX1. Repeated stimulation of reverse NCX1 produced a long-lasting decrease of Ca2+ transients ('rundown'). Rundown of NCX1 was independent of membrane PIP2 depletion. Although the activation of protein kinase C (PKC) was observed during the Ca2+ transients, neither a selective PKC inhibitor (calphostin C) nor a PKC activator (PMA) changed the degrees of rundown. By comparison, a non-specific PKC inhibitor, staurosporine (STS), reversed rundown in a dose-dependent and reversible manner. The action of STS was unaffected by pretreatment of the cells with calphostin C, PMA, or forskolin. Taken together, the results suggest that the stimulation of reverse NCX1 by STS is independent of PKC and/or PKA inhibition.
Keyword
MeSH Terms
Figure
Reference
-
Blaustein MP., Lederer WJ. Sodium/calcium exchange: its physiological implications. Physiol Rev. 79:763–854. 1999.
ArticleChoi JS., Hahn SJ., Rhie DJ., Jo YH., Kim MS. Staurosporine directly blocks Kv1.3 channels expressed in Chinese hamster ovary cells. Naunyn-Schmiedebergs Arch. Pharmacol. 359:256–261. 1999.Egger M., Porzig H., Niggli E., Schwaller B. Rapid turnover of the “functional” Na+-Ca2+ exchanger in cardiac myocytes revealed by an antisense oligodeoxynucleotide approach. Cell Calcium. 37:233–243. 2005.Gescher A. Staurosporine analogues-pharmacological toys or useful antitumor agents? Crit Rev Oncol Hematol. 34:127–135. 2000.Hilgemann DW. Regulation and deregulation of cardiac Na+-Ca2+ exchange in giant excised sarcolemmal membrane patches. Nature. 344:242–245. 1990.Hilgemann DW., Ball R. Regulation of cardiac Na+,Ca2+ exchange and KATP potassium channels by PIP2. Science. 273:956–959. 1996.Hilgemann DW., Collins A., Matsuoka S. Steady-state and dynamic properties of cardiac sodium-calcium exchange. Secondary modulation by cytoplasmic calcium and ATP. J Gen Physiol. 100:933–961. 1992a.
ArticleHilgemann DW., Matsuoka S., Nagel GA., Collins A. Steady-state and dynamic properties of cardiac sodium-calcium exchange. Sodium-dependent inactivation. J Gen Physiol. 100:905–932. 1992b.
ArticleIwamoto T., Pan Y., Nakamura TY., Wakabayashi S., Shigekawa M. Protein kinase C-dependent regulation of Na+/Ca2+ exchanger isoforms NCX1 and NCX3 does not require their direct phosphorylation. Biochemistry. 37:17230–17238. 1998.Kang TM., Hilgemann DW. Multiple transport modes of the cardiac Na+/Ca2+ exchanger. Nature. 427:544–548. 2004.Katanosaka Y., Iwata Y., Kobayashi Y., Shibasaki F., Wakabayashi S., Shigekawa M. Calcineurin inhibits Na+/Ca2+ exchange in phenylephrine-treated hypertrophic cardiomyocytes. J Biol Chem. 280:5764–5772. 2005.Ko JH., Park WS., Earm YE. The protein kinase inhibitor, staurosporine, inhibits L-type Ca2+ current in rabbit atrial myocytes. Biochem Biophys Res Commun. 329:531–537. 2005.Lee JE., Kang TM. Ca2+-dependent long-term inactivation of cardiac Na+/Ca2+ exchanger. Korean J Physiol Pharmacol. 11:183–188. 2007.Linck B., Qiu Z., He Z., Tong Q., Hilgemann DW., Philipson KD. Functional comparison of the three isoforms of the Na+/Ca2+ exchanger (NCX1, NCX2, NCX3). Am J Physiol. 274:C415–423. 1998.Opuni K., Reeves JP. Feedback inhibition of sodium/calcium exchange by mitochondrial calcium accumulation. J Biol Chem. 275:21549–21554. 2000.
ArticlePark WS., Son YK., Han J., Kim N., Ko JH., Bae YM., Earm YE. Staurosporine inhibits voltage-dependent K+ current through a PKC-independent mechanism in isolated coronary arterial smooth muscle cells. J Cardiovasc Pharmacol. 45:260–269. 2005.Reeves JP., Condrescu M. Allosteric activation of sodium-calcium exchange activity by calcium: persistence at low calcium concentrations. J Gen Physiol. 122:621–639. 2003.Reeves JP., Hale CC. The stoichiometry of the cardiac sodium-calcium exchange system. J Biol Chem. 259:7733–7739. 1984.
ArticleRuëgg UT., Burgess GM. Staurosporine, K-252 and UCN-01: potent but nonspecific inhibitors of protein kinases. Trends Pharmacol Sci. 10:218–220. 1989.Shen C., Lin MJ., Yaradanakul A., Lariccia V., Hill JA., Hilgemann DW. Dual control of cardiac Na+/Ca2+ exchange by PIP2: analysis of the surface membrane fraction by extracellular cysteine PEGylation. J Physiol. 582:1011–1026. 2007.Yanagihara N., Tachikawa E., Izumi F., Yasugawa S., Yamamoto H., Miyamoto E. Staurosporine: an effective inhibitor for Ca2+/Calmodulin dependent protein kinase II. J Neurochem. 56:294–298. 1991.Yang J., Liu X., Bhalla K., Kim CN., Ibrado AM., Cai J., Peng TI., Jones DP., Wang X. Prevention of apoptosis by Bcl-2: release of cytochrome c from mitochondria blocked. Science. 275:1129–1132. 1997.
ArticleYaradanakul A., Feng S., Shen C., Lariccia V., Lin MJ., Yang J., Kang TM., Dong P., Yin HL., Albanesi JP., Hilgemann DW. Dual control of cardiac Na+/Ca2+ exchange by PIP2: electrophysiological analysis of direct and indirect mechanisms. J Physiol. 582:991–1010. 2007.Yaradanakul A., Wang TM., Lariccia V., Lin MJ., Shen C., Liu X., Hilgemann DW. Massive Ca-induced membrane fusion and phospholipid changes triggered by reverse Na/Ca exchange in BHK fibroblasts. J Gen Physiol. 132:29–50. 2008.
ArticleZhang XQ., Ahlers BA., Tucker AL., Song J., Wang J., Moorman JR., Mounsey JP., Carl LL., Rothblum LI., Cheung JY. Phospholemman inhibition of the cardiac Na+/Ca2+ exchanger. Role of phosphorylation. J Biol Chem. 281:7784–7792. 2006.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ca2+-dependent Long-term Inactivation of Cardiac Na+/Ca2+ Exchanger
- Hypoxia Delays the Intracellular Ca2+ Clearance by Na+ - Ca2+ Exchanger in Human Adult Cardiac Myocytes
- Interactions between Estradiol-17beta-BSA and Calcitropic Hormones in Ca2+ Uptake in Renal Proximal Tubule Cells
- Effect of PKC-dependent Change of K+ Current Activity on Histamine-induced Contraction of Rabbit Coronary Artery
- Na+-Ca2+ exchanger modulates Ca2+ content in intracellular Ca2+ stores in rat osteoblasts