J Breast Cancer.
2008 Sep;11(3):125-132. 10.4048/jbc.2008.11.3.125.
The Efficacy of Enoxaparin for the Prevention of a Pulmonary Thromboembolism in a Skin-sparing Mastectomy with Immediate Reconstruction in Breast Cancer
- Affiliations
-
- 1Department of Surgery, College of Medicine, Hanyang University, Seoul, Korea.
- 2Department of Surgery, University of Ulsan, College of Medicine and Asan Medical Center, Seoul, Korea. brdrson@korea.com
- 3Department of Plastic Surgery, University of Ulsan, College of Medicine and Asan Medical Center, Seoul, Korea.
- 4Department of Pulmonology, College of Medicine Dongguk University Pohang Hospital, Pohang, Korea.
- 5Department of Surgery, College of Medicine Dongguk University International Hospital, Goyang, Korea.
- KMID: 1485105
- DOI: http://doi.org/10.4048/jbc.2008.11.3.125
Abstract
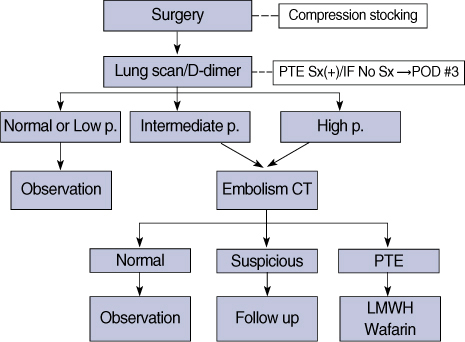
- PURPOSE
Performance of a skin-sparing mastectomy with immediate reconstruction provides psychological satisfaction and good cosmetic outcome for patients with breast cancer. However, this is a lengthy procedure to perform, and there is increased risk of pulmonary thromboembolism (PTE). The purpose of this study was to evaluate the efficiency of the use of low molecular weight heparins (enoxaparin) for prophylaxis against a pulmomary thromboembolism followed by mastectomy with an immediate transverse rectus abdominis myocutaneous flap (TRAM) in breast cancer. METHODS: A total of 123 patients underwent a skin-sparing mastectomy with an immediate TRAM. The "non-enoxaparin group" wore compression stockings for PTE prophylaxis and the "enoxaparin group" received enoxaparin (40 mg SC injection, once daily starting 2 hr before surgery and continuing for 6 days postoperatively) in conjunction with the use of compression stockings. Lung perfusion, inhalation scans, and serum D-dimer assays were performed on postoperative day 3. If findings were clinically suspicious or intermediate to high probability of a PTE in a lungs scan, embolism computed tomography was performed. Patients were prospectively investigated according to the clinicopathological data. We compared the incidence of PTE and hemorrhagic complications between the two groups. RESULTS: There were no significant clinicopathological differences between the two groups. Eleven patients developed a PTE (nine patients in the non-enoxaparin group and two patients in the enoxaparin group). The prevalence rate of a PTE was 17.3% and 3.2% for each group, respectively (p=0.01). One patient in the non-enoxaparin group required a second operation for bleeding control and three patients in the enoxaparin group needed transfusions. There were minor hemorrhagic complications in the enoxaparin group that improved after supportive management. CONCLUSION: Although there were minor hemorrhagic complications, enoxaparin is safe and effective in a preventing PTE in patients that undergo immediate reconstruction after a skin-sparing mastectomy.
Keyword
MeSH Terms
-
Breast
Breast Neoplasms
Cosmetics
Embolism
Enoxaparin
Fibrin Fibrinogen Degradation Products
Hemorrhage
Heparin, Low-Molecular-Weight
Humans
Incidence
Inhalation
Lung
Mastectomy
Perfusion
Prevalence
Prospective Studies
Pulmonary Embolism
Rectus Abdominis
Stockings, Compression
Thromboembolism
Cosmetics
Enoxaparin
Fibrin Fibrinogen Degradation Products
Heparin, Low-Molecular-Weight
Figure
Cited by 1 articles
-
Breast reconstruction using pedicled transverse rectus abdominis musculocutaneous (TRAM) flap
Jin Sup Eom
J Korean Med Assoc. 2011;54(1):12-21. doi: 10.5124/jkma.2011.54.1.12.
Reference
-
1. Lee AY. Cancer and thromboembolic disease: pathogenic mechanisms. Cancer Treat Rev. 2002. 28:137–140.
Article2. Prandoni P, Falanga A, Piccioli A. Cancer and venous thromboembolism. Lancet Oncol. 2005. 6:401–410.
Article3. Bick RL. Cancer-associated thrombosis. N Engl J Med. 2003. 349:109–111.
Article4. Geerts WH, Pineo GF, Heit JA, Bergqvist D, Lassen MR, Colwell CW, et al. Prevention of venous thromboembolism: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest. 2004. 126:S338–S400.5. Rickles FR, Levine MN. Epidemiology of thrombosis in cancer. Acta Haematol. 2001. 106:6–12.
Article6. Lyman GH, Khorana AA, Falanga A, Clarke-Pearson D, Flowers C, Jahanzeb M, et al. American society of clinical oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol. 2007. 25:5490–5505.
Article7. Venous thromboembolic disease clinical practice guidelines in oncology-v.1. 2007. National Comprehensive Cancer Network: http://www.nccn.org/professionals/physician_gls/PDF/vte.pdf accessed June 26, 2008.8. Mismetti P, Laporte S, Darmon JY, Buchmuller A, Decousus H. Meta-analysis of low molecular weight heparin in the prevention of venous thromboembolism in general surgery. Br J Surg. 2001. 88:913–930.
Article9. Yoon HS. Nationwide breast cancer data of 2002 in Korea. J Breast Cancer. 2004. 7:72–83.10. Patiar S, Kirwan CC, McDowell G, Bundred NJ, McCollum CN, Byrne GJ. Prevention of venous thromboembolism in surgical patients with breast cancer. Br J Surg. 2007. 94:412–420.
Article11. Son BH, Kwak BS, Kim JK, Kim HJ, Hong SJ, Lee JS, et al. Symptomatic pulmonary thromboembolism following skin-sparing mastectomy with Immediate TRAM reconstruction in breast cancer patients. J Korean Surg Soc. 2006. 70:281–287.12. Lee JS, Son BH, Choi HS, Jung MS, Hong SJ, Kim JK, et al. Pulmonary thromboembolism following mastectomy with immediate TRAM in the patients with breast cancer: a prospective study. J Breast Cancer. 2006. 9:354–360.
Article13. White RH, Zhou H, Romano PS. Incidence of symptomatic venous throm boembolism after different elective or urgent surgical procedures. Thromb Haemost. 2003. 90:446–455.
Article14. Ibrahim EH, Iregui M, Prentice D, Sherman G, Kollef MH, Shannon W. Deep vein thrombosis during prolonged mechanical ventilation despite prophylaxis. Crit Care Med. 2002. 30:771–774.
Article15. Clahsen PC, van de Velde CJ, Julien JP, Floiras JL, Mignolet FY. Thromboembolic complications after perioperative chemotherapy in women with early breast cancer: a European organization for research and treatment of cancer breast cancer cooperative group study. J Clin Oncol. 1994. 12:1266–1271.
Article16. Wedgwood KR, Benson EA. Non-tumour morbidity and mortality after modified radical mastectomy. Ann R Coll Surg Engl. 1992. 74:314–317.17. Saphner T, Tormey DC, Gray R. Venous and arterial thrombosis in patients who received adjuvant therapy for breast cancer. J Clin Oncol. 1991. 9:286–294.
Article18. Fisher B, Dignam J, Wolmark N, DeCillis A, Emir B, Wickerham DL, et al. Tamoxifen and chemotherapy for lymph node-negative, estrogen receptor-positive breast cancer. J Natl Cancer Inst. 1997. 89:1673–1682.
Article19. Olsson EH, Tukiainen E. Three-year evaluation of late breast reconstruction with a free transverse rectus abdominis musculocutaneous flap in a county hospital in Sweden: a retrospective study. Scand J Plast Reconstr Surg Hand Surg. 2005. 39:33–38.
Article20. Wells PS, Lensing AW, Hirsh J. Graduated compression stockings in the prevention of postoperative venous thromboembolism. A metaanalysis. Arch Intern Med. 1994. 154:67–72.
Article21. Clarke-Pearson DL, Dodge RK, Synan I, McClelland RC, Maxwell GL. Venous thromboembolism prophylaxis: patients at high risk to fail intermittent pneumatic compression. Obstet Gynecol. 2003. 101:157–163.
Article22. Agnelli G, Bolis G, Capussotti L, Scarpa RM, Tonelli F, Bonizzoni E, et al. A clinical outcome-based prospective study on venous thromboembolism after cancer surgery: the @RISTOS project. Ann Surg. 2006. 243:89–95.
Article23. Bergqvist D, Agnelli G, Cohen AT, Eldor A, Nilsson PE, Le Moigne-Amrani A, et al. Duration of prophylaxis against venous thromboembolism with enoxaparin after surgery for cancer. N Engl J Med. 2002. 346:975–980.
Article24. Lee RE, Ho KN, Karran SJ, Taylor I. Haemorrhagic effects of sodium heparin and calcium heparin prophylaxis in patients undergoing mastectomy. J R Coll Surg Edinb. 1989. 34:149–151.25. Steele RJ, Richmond JD, Lee D, Chetty U, Davies GC. The effect of low-dose subcutaneous heparin on wound haemorrhage, a controlled study of mastectomy patients. Br J Clin Pract. 1983. 37:95–98.26. Bakker XR, Roumen RM. Bleeding after excision of breast lumps. Eur J Surg. 2002. 168:401–403.
Article27. Hussien M, Lee S, Malyon A, Norrie J, Webster M. The impact of intraoperative hypotension on the development of wound haematoma after breast reduction. Br J Plast Surg. 2001. 54:517–522.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Immediate Breast Reconstruction with TRAM Flap after Nipple-Areolar Sparing Mastectomy
- Skin - sparing Mastectomy with Circumareolar Incision and Immediate TRAM & One - stage Star Flap Nipple - areolar Complex Reconstruction
- The Lazy S Design: A Novel Skin Closure Design in Skin-Sparing Mastectomy for Implant-Based Breast Reconstruction
- Immediate One-Stage Breast Reconstruction Including Nipple-Areolar Complex
- Skin-Sparing Mastectomy with Circumareolar Incision and Immediate Reconstruction in Breast Cancer