J Korean Soc Spine Surg.
2008 Mar;15(1):1-8. 10.4184/jkss.2008.15.1.1.
Posterior Hemivertebra Excision in Congenital Scoliosis
- Affiliations
-
- 1Seoul Spine Institute, Sanggye Paik Hospital, College of Medicine, Inje University, Seoul, Korea. toetotoe1@sanggyepaik.ac.kr
- 2Department of Orthopaedic Surgery, Sanggye Paik Hospital, College of Medicine, Inje University, Seoul, Korea.
- KMID: 1482837
- DOI: http://doi.org/10.4184/jkss.2008.15.1.1
Abstract
-
STUDY DESIGN: Retrospective study
OBJECTIVES
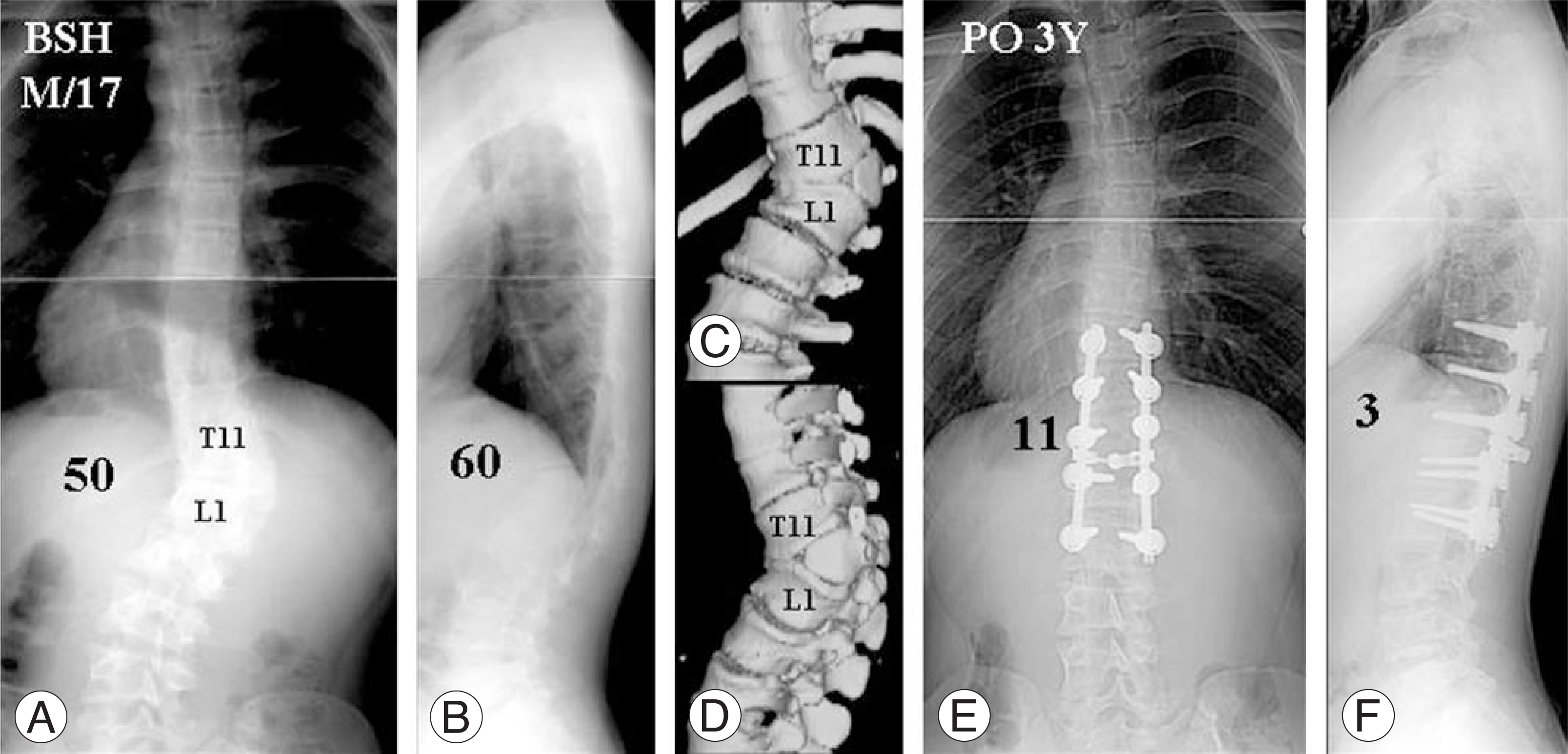
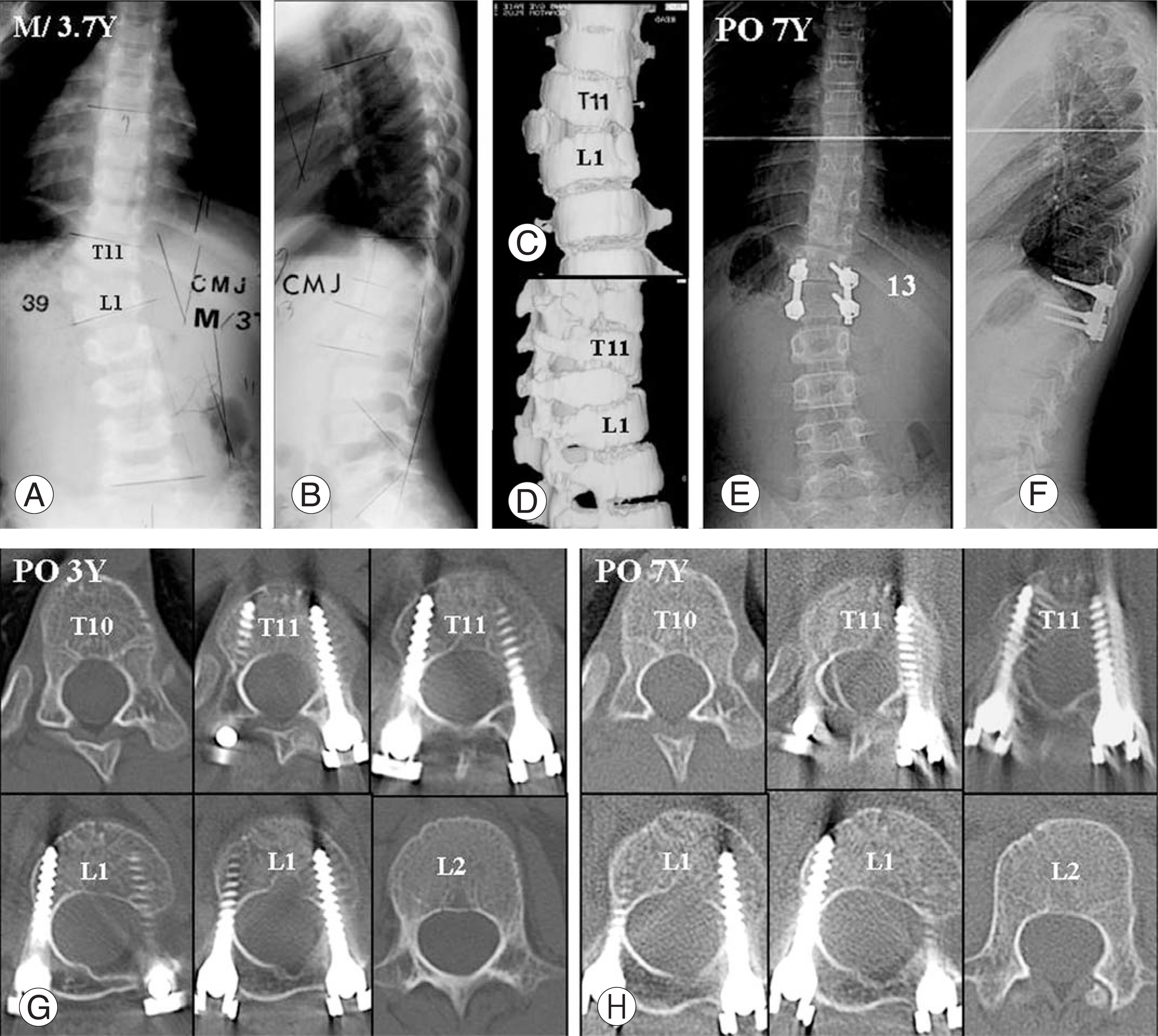
To evaluate the surgical outcome of congenital scoliosis with a hemivertebra treated by posterior hemivertebra excision and pedicle screw instrumentation. SUMMARY OF LITERATURE REVIEW: Posterior hemivertebra excision can be accomplished through a single posterior approach, and excellent correction and outcome may be achieved.
MATERIALS AND METHODS
Forty patients with one fully segmented hemivertebra treated by posterior hemivertebra excision with pedicle screw instrumentation were retrospectively analyzed after a minimum follow-up of 2 years (range 2~7.7 years). The mean age at surgery was 15.9 years (range 2.6~37.9 years). Preoperative and postoperative standing radiographs were used to assess radiographic parameters.
RESULTS
The average number of vertebrae in the major curve was 4.2 (range 3~8), and the average flexibility was 29% (range 8~59%). The average length of fusion was 3.5 segments (range 1~6). The number of fused vertebrae had a positive correlation with age at the index surgery (r=0.345, p<0.05). Mean preoperative scoliosis of 48+/-12degrees was corrected to a mean of 17+/-10degrees (65% correction), and mean preoperative kyphosis of 46+/-18degrees was corrected to a mean of 12+/-12degrees at the most recent follow-up. The compensatory curve had a mean of 25+/-10degrees preoperatively and spontaneously corrected to a mean of 8+/-8degrees (70% correction) at the most recent follow-up. The mean operating time was 233+/-81 min, with an average blood loss of 2904 ml. There was neither crankshaft phenomenon nor iatrogenic spinal stenosis in 6 patients under the age of 5 years after an average follow-up of 6 years.
CONCLUSIONS
Posterior hemivertebra excision using pedicle screw instrumentation in congenital scoliosis due to a hemivertebra is a safe and effective procedure. Posterior hemivertebra excision at an early age may reduce the fusion length while avoiding the induction of iatrogenic spinal stenosis during follow-up.
Keyword
MeSH Terms
Figure
Reference
-
1). Leatherman KD, Dickson RA. Two-stage corrective surgery for congenital deformities of the spine. J Bone Joint Surg Br. 1979; 61:324–328.
Article2). Bradford DS, Boachie-Adjei O. One-stage anterior and posterior hemivertebra resection and arthrodesis for congenital scoliosis. J Bone Joint Surg Am. 1990; 72:536–540.3). Nakamura H, Matsuda H, Konishi S, Yamano Y. Single-stage excision of hemivertebra via the posterior approach alone for congenital spinal deformity: follow-up period longer than ten years. Spine. 2002; 27:110–115.4). Roaf R. The treatment of progressive scoliosis by unilateral growth arrest. J Bone Joint Surg Br. 1963; 4:637–651.5). Royle ND. The operative removal of an accessory vertebra. Med J Aust. 1928; 1:467–468.
Article6). Suk SI, Chung ER, Kim JH, Kim SS, Lee JS, Choi WK. Posterior vertebral column resection for severe rigid scoliosis. Spine. 2005; 30:1682–1687.
Article7). McMaster MJ, Ohtsuka K. The natural history of congenital scoliosis: a study of two hundred and fifty-one patients. J Bone Joint Surg Am. 1982; 64:1128–1147.
Article8). Winter RB. Congenital spinal deformity in the Moe’s textbook of scoliosis and other spinal deformities. 3rd ed.Philadelphia: WB Saunders Co;p. 257–294. 1995.9). Slabaugh PB, Winter RB, Lonstein JE, Moe JH. Lumbosacral hemivertebra: a review of twenty-four patients, with excision in eight. Spine. 1980; 5:234–244.10). Ruf M, Harms J. Hemivertebra resection by a posterior approach: innovative operative technique and first results. Spine. 2002; 27:1116–1123.11). Ruf M, Harms J. Posterior hemivertebra resection with transpedicular instrumentation: early correction in children aged 1 to 6 years. Spine. 2003; 28:2132–2138.
Article12). Papp T, Porter RW, Aspden RM. The growth of the lumbar vertebral canal. Spine. 1994; 19:2770–2773.
Article13). Porter RW, Pavitt D. The vertebral canal: I. Nutrition and development, an archaeological study. Spine. 1987; 12:901–906.14). Jeffrey JE, Campbell DM, Golden MH, Smith FW, Porter RW. Antenatal factors in the development of the lumbar vertebral canal: a magnetic resonance imaging study. Spine. 2003; 28:1418–1423.15). Ferree BA. Morphometric characteristics of pedicles of the immature spine. Spine. 1992; 17:887–891.
Article16). Zindrick MR, Knight GW, Sartori MJ, Camevale TJ, Patwardhan AG, Lorenz MA. Pedicle morphology of the immature thoracolumbar spine. Spine. 2000; 25:2726–2735.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and treatment of congenital scoliosis
- Surgical treatment of Quadrant Hemivertebra in Congenital Kyphoscoliosis
- Outcomes of Posterior Lumbar Hemivertebra Resection and Short Fusion in Patients With Severe Sacral Tilt
- Treatment of Congenital Scoliosis
- Vertebral and Intraspinal Anomalies in Indian Population with Congenital Scoliosis: A Study of 119 Consecutive Patients