J Korean Fract Soc.
2008 Oct;21(4):304-311. 10.12671/jkfs.2008.21.4.304.
The Relationship between Progression of Body Collapse and MRI Findings in Osteoporotic Stable Thoracolumbar Fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, Ewha Womans University School of Medicine, Seoul, Korea. ydkoh@ewha.ac.kr
- KMID: 1480920
- DOI: http://doi.org/10.12671/jkfs.2008.21.4.304
Abstract
-
PURPOSE: To find out the relationship between the initial Magnetic Resonance Image (MRI) findings and the progression of vertebra collapse when treated with Jewett brace in osteoporotic stable thoracolumbar fractures.
MATERIALS AND METHODS
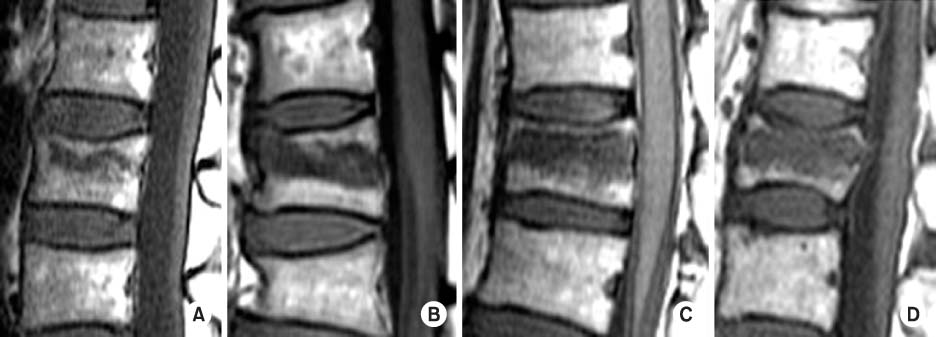
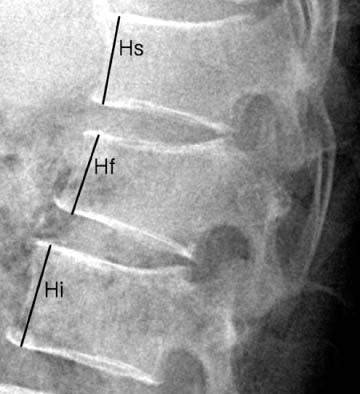
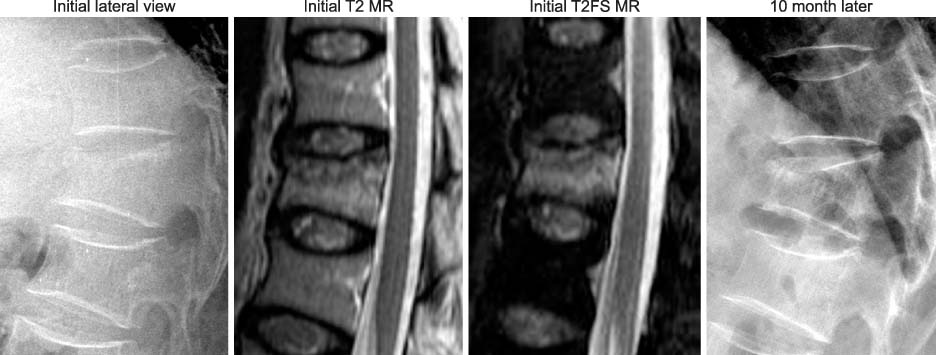
We divided 38 cases of 37 patients of thoracolumbar osteoporotic stable thoracolumbar fractures who were treated with Jewett brace into two groups. One group was composed of those body collapse progressed more than 10% compared with the initial state, and the other group less than 10%. We analyzed the relationships between the progression of collapse and the superior endplate fractures, the fracture line extending to posterior cortex, the size of bone marrow edema, the signal intensity on T1 and T2 weighted MR images, the presence of paravertebral hematoma, and the degree of posterior extensor muscle atrophy using MR images.
RESULTS
The body collapse was more likely to progress when there was superior endplate fracture, when it showed larger size of bone marrow edema on T1 weighted image, and transverse low signal on T2 weighted image. But extending of fracture line to posterior cortex, presence of paravertebral hematoma, and degree of posterior extensor muscle atrophy did not show any statistical correlations to progression of collapse.
CONCLUSION
The body collapse is more likely to progress when there was superior endplate fracture, larger low signal on T1 weighted image and low signal on T2 weighted image at initial MRI treated with Jewett brace.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Influence of Initial Magnetic Resonance Imaging Findings on the Compression Rate of Thoracolumbar Osteoporotic Vertebral Compression Fracture
Seok-Ha Hwang, Seung-Pyo Suh, Young-Kyun Woo, Ho-Seung Jeon, Ho-Won Jeong
J Korean Orthop Assoc. 2018;53(4):341-349. doi: 10.4055/jkoa.2018.53.4.341.
Reference
-
1. Ağuş H, Kayali C, Arslantaş M. Nonoperative treatment of burst-type thoracolumbar vertebra fractures: clinical and radiological results of 29 patients. Eur Spine J. 2005; 14:536–540.
Article2. Akbarnia BA, Crandall DG, Burkus K, Matthews T. Use of long rods and a short arthrodesis for burst fractures of the thoracolumbar spine. A long-term follow-up study. J Bone Joint Surg Am. 1994; 76:1629–1635.
Article3. Alanay A, Yazici M, Acaroglu E, Turhan E, Cila A, Surat A. Course of nonsurgical management of burst fractures with intact posterior ligamentous complex: an MRI study. Spine. 2004; 29:2425–2431.
Article4. Baba H, Maezawa Y, Kamitani K, Furusawa N, Imura S, Tomita K. Osteoporotic vertebral collapse with late neurological complications. Paraplegia. 1995; 33:281–289.
Article5. Cantor JB, Lebwohl NH, Garvey T, Eismont FJ. Nonoperative management of stable thoracolumbar burst fractures with early ambulation and bracing. Spine. 1993; 18:971–976.
Article6. Chow GH, Nelson BJ, Gebhard JS, Brugman JL, Brown CW, Donaldson DH. Functional outcome of thoracolumbar burst fractures managed with hyperextension casting or bracing and early mobilization. Spine. 1996; 21:2170–2175.
Article7. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994; 304:78–83.8. Jacobs RR, Asher MA, Snider RK. Thoracolumbar spinal injuries. A comparative study of recumbent and operative treatment in 100 patients. Spine. 1980; 5:463–477.9. James KS, Wenger KH, Schlegel JD, Dunn HK. Biomechanical evaluation of the stability of thoracolumbar burst fractures. Spine. 1994; 19:1731–1740.
Article10. Kaneda K, Ito M, Taneichi H, Sato S, Abumi K, Asano S. Osteoporotic posttraumatic vertebral collapse with neurological deficits of the thoracolumar spine: anterior decompression and reconstruction. Rinsho Seikei Geka. 1996; 31:463–470.11. Kaplan PA, Orton DF, Aselson RJ. Osteoporosis with vertebral compression fractures, retropulsed fragments, and neurologic compromise. Radiology. 1987; 165:533–535.
Article12. Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994; 3:184–201.
Article13. McAfee PC, Yuan HA, Fredrickson BE, Lubicky JP. The value of computed tomography in thoracolumbar fractures. An analysis of one hundred consecutive cases and a new classification. J Bone Joint Surg Am. 1983; 65:461–473.
Article14. Mumford J, Weinstein JN, Spratt KF, Goel VK. Thoracolumbar burst fractures. The clinical efficacy and outcome of nonoperative management. Spine. 1993; 18:955–970.15. Oner FC, van Gils AP, Dhert WJ, Verbout AJ. MRI findings of thoracolumbar spine fractures: a categorization based on MRI examinations of 100 fractures. Skeletal Radiol. 1999; 28:433–443.
Article16. Oner FC, van Gils AP, Faber JA, Dhert WJ, Verbout AJ. Some complications of common treatment schemes of thoracolumbar spine fractures can be predicted with magnetic resonance imaging: prospective study of 53 patients with 71 fractures. Spine. 2002; 27:629–636.
Article17. Tezer M, Erturer RE, Ozturk C, Ozurk I, Kuzgun U. Conservative treatment of fractures of thoracolumbar spine. Int Orthop. 2005; 29:78–82.18. Tropiano P, Huang RC, Louis CA, Poitout DG, Louis RP. Functional and radiographic outcome of thoracolumbar and lumbar burst fractures managed by closed orthopaedic reduction and casting. Spine. 2003; 28:2459–2465.
Article19. Weinstein JN, Collalto P, Lehmann TR. Thoracolumbar "burst" fractures treated conservatively: a long-term follow-up. Spine. 1988; 13:33–38.
Article20. Young MH. Long-term consequences of stable fractures of the thoracic and lumbar vertebral bodies. J Bone Joint Surg Br. 1973; 55:295–300.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prediction of Subsequent Vertebral Collapse after Osteoporotic Thoracolumbar Vertebral Fractures
- Influence of Compression Ratio Differences between Magnetic Resonance Images and Simple Radiographs on Osteoporotic Vertebral Compression Fracture Prognosis after Vertebroplasty
- The Diagnosis of Osteoporotic Occult Vertebral Fracture and Vertebroplasty
- Differences of Fracture Patterns by the Level of the Thoracolumbar and Lumbar Burst Fractures
- Relationship between the Progression of Kyphosis in Thoracolumbar Osteoporotic Vertebral Compression Fractures and Magnetic Resonance Imaging Findings