J Cardiovasc Ultrasound.
2009 Dec;17(4):127-134. 10.4250/jcu.2009.17.4.127.
Comparison of Left Ventricular Hypertrophy, Fibrosis and Dysfunction According to Various Disease Mechanisms such as Hypertension, Diabetes Mellitus and Chronic Renal Failure
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. hojheart@catholic.ac.kr
- KMID: 1473715
- DOI: http://doi.org/10.4250/jcu.2009.17.4.127
Abstract
- BACKGROUND
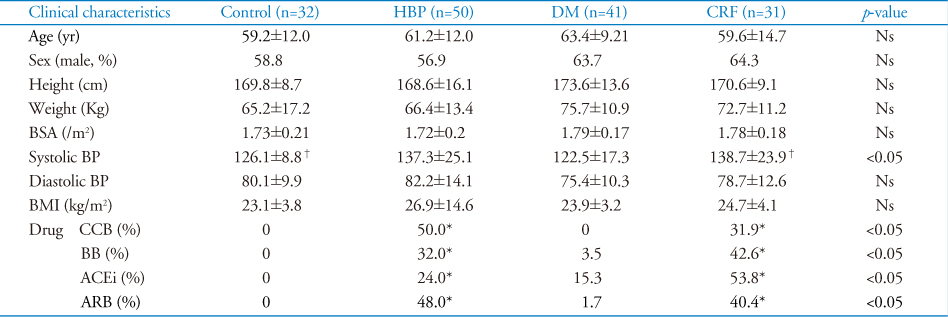
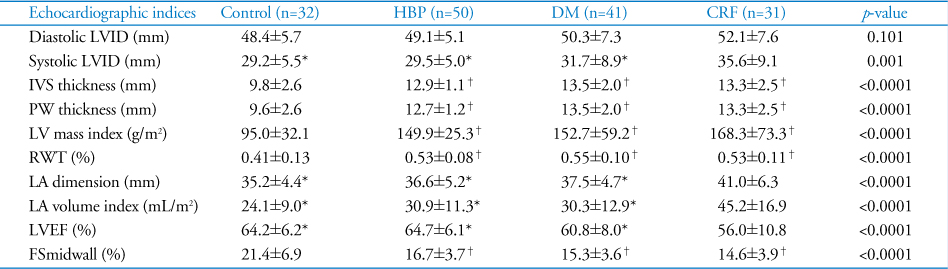
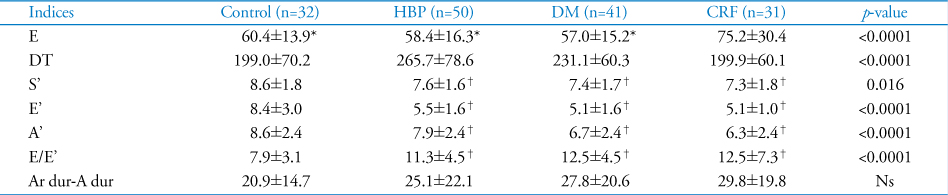
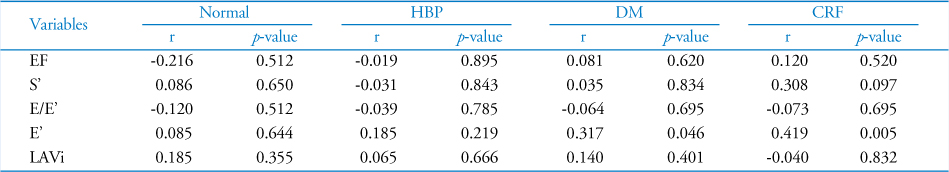
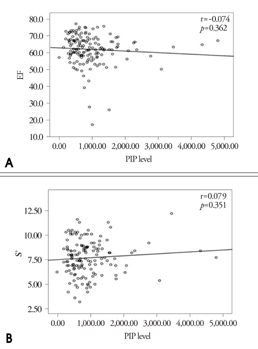
Left ventricular hypertrophy (LVH) has been known as an important predictor of prognosis of cardiovascular disease. Carboxy-terminal propeptide of procollagen type I (PIP) is related with myocardial fibrosis. We sought to analyze the differences in the characteristics of LVH, myocardial fibrosis, and LV functions among hypertension (HBP), diabetes mellitus (DM) and chronic renal failure (CRF). METHODS: We enrolled consecutive patients with LVH. Patients were grouped as HBP (n=50), DM (n=41), CRF (n=31). Age and sex-matched normal control was also enrolled (n=32). Echocardiography and blood sampling for serum PIP level measuring was performedin all participants. RESULTS: There were no differences in baseline characteristics except systolic blood pressure among four groups. In three patients groups, their LV mass indices were significantly increased than control. Serum PIP level in CRF was much higher than others (CRF 1505.5 vs. HBP 868.7 vs. DM 687.5 vs. control 826.4, p<0.0001). LV diastolic and systolic function evaluated by E', E/E, S' and midwall fractional shortening was significantly decreased in three patients groups. However, LAVi was significantly elevated and LV ejection fraction was significantly decreased in CRF compared to others. In correlation analysis, indices of diastolic function were weakly, but statistically correlated with PIP (E': r=0.234, p=0.006; LAVi: r=0.231, p=0.006). CONCLUSION: In CRF, LV function was more deteriorated and serum PIP was more elevated when compared to HBP or DM. Therefore, myocardial fibrosis may play an important role to LV dysfunction as well as LV hypertrophy in CRF in some degree.
MeSH Terms
Figure
Reference
-
1. Díez J, González A, López B, Querejeta R. Mechanisms of disease: pathologic structural remodeling is more than adaptive hypertrophy in hypertensive heart disease. Nat Clin Pract Cardiovasc Med. 2005. 2:209–216.
Article2. Devereux RB, Roman MJ, Paranicas M, O'Grady MJ, Lee ET, Welty TK, Fabsitz RR, Robbins D, Rhoades ER, Howard BV. Impact of diabetes on cardiac structure and function: the strong heart study. Circulation. 2000. 101:2271–2276.
Article3. Guerin AP, Adda H, London GM, Marchais SJ. Cardiovascular disease in renal failure. Minerva Urol Nefrol. 2004. 56:279–288.4. Aurigemma GP, Silver KH, Priest MA, Gaasch WH. Geometric changes allow normal ejection fraction despite depressed myocardial shortening in hypertensive left ventricular hypertrophy. J Am Coll Cardiol. 1995. 26:195–202.
Article5. Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990. 322:1561–1566.
Article6. Casale PN, Devereux RB, Milner M, Zullo G, Harshfield GA, Pickering TG, Laragh JH. Value of echocardiographic measurement of left ventricular mass in predicting cardiovascular morbid events in hypertensive men. Ann Intern Med. 1986. 105:173–178.
Article7. Rossi MA. Pathologic fibrosis and connective tissue matrix in left ventricular hypertrophy due to chronic arterial hypertension in humans. J Hypertens. 1998. 16:1031–1041.
Article8. Ciulla M, Paliotti R, Hess DB, Tjahja E, Campbell SE, Magrini F, Weber KT. Echocardiographic patterns of myocardial fibrosis in hypertensive patients: endomyocardial biopsy versus ultrasonic tissue characterizatien. J Am Soc Echocardiogr. 1997. 10:657–664.
Article9. Querejeta R, Varo N, López B, Larman M, Artiñano E, Etayo JC, Martínez Ubago JL, Gutierrez-Stampa M, Emparanza JI, Gil MJ, Monreal I, Mindán JP, Díez J. Serum cardoxy-terminal propeptide of procollagen type I is a marker of myocardial fibrosis in hypertensive heart disease. Circulation. 2000. 101:1729–1735.
Article10. Díez J, Panizo A, Gil MJ, Monreal I, Hernández M, Pardo Mindán J. Serum markers of collagen type I metabolism in spontaneously hypertensive rats: relation to myocardial fibrosis. Circulation. 1996. 93:1026–1032.
Article11. López B, Querejeta R, Varo N, González A, Larman M, Martínez Ubago JL, Díez J. Usefulness of serum carboxy-terminal propeptide of procollagen type I in assessment of the cardioreparative ability of antihypertensive treatment in hypertensive patients. Circulation. 2001. 104:286–291.
Article12. Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978. 58:1072–1083.
Article13. Schiller NB, Shah PM, Crawford M, Demaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989. 2:358–367.
Article14. Teichholz LE, Kreulen T, Herman MV, Gorlin R. Problems in echocardiographic volume determinations: echocardiographic-angiographic correlations in the presence or absence of asynergy. Am J Cardiol. 1976. 37:7–11.
Article15. Ihm SH, Youn HJ, Kim SR, Park CS, Chang KY, Seung KB, Kim JH, Hong SJ, Choi KB. Relation between serum carboxy-terminal propeptide of type 1 procollagen (PIP), a marker of myocardial fibrosis, and left ventricular diastolic function in patients with early type 2 diabetes mellitus. Korean Circulation J. 2005. 35:500–506.
Article16. Koren MJ, Devereux RB. Mechanism, effects, and reversal of left ventricular hypertrophy in hypertension. Curr Opin Nephrol Hypertens. 1993. 2:87–95.
Article17. Taegtmeyer H, McNulty P, Young ME. Adaptation and maladaptation of the heart in diabetes: part I: general concepts. Circulation. 2002. 105:1727–1733.
Article18. Young ME, McNulty P, Taegtmeyer H. Adaptation and maladaptation of the heart in diabetes: part II: potential mechanisms. Circulation. 2002. 105:1861–1870.
Article19. Candido R, Forbes JM, Thomas MC, Thallas V, Dean RG, Burns WC, Tikellis C, Ritchie RH, Twigg SM, Cooper ME, Burrell LM. A breaker of advanced glycation end products attenuates diabetes-induced myocardial structural changes. Circ Res. 2003. 92:785–792.
Article20. Brownlee M, Cerami A, Vlassara H. Advanced glycosylation end products in tissue and the biochemical basis of diabetic complications. N Engl J Med. 1988. 318:1315–1321.
Article21. Ha SK, Park HS, Kim SJ, Park CH, Kim DS, Kim HS. Prevalence and patterns of left ventricular hypertrophy in patients with predialysis chronic renal failure. J Korean Med Sci. 1998. 13:488–494.
Article22. Ulasi II, Arodiwe EB, Ijoma CK. Left ventricular hypertrophy in African Black patients with chronic renal failure at first evaluation. Ethn Dis. 2006. 16:859–864.23. Vlahakos DV, Hahalis G, Vassilakos P, Marathias KP, Geroulanos S. Relationship between left ventricular hypertrophy and plasma renin activity in chronic hemodialysis patients. J Am Soc Nephrol. 1997. 8:1764–1770.
Article24. Weber KT, Brilla CG, Campbell SE, Zhou G, Matsubara L, Guarda E. Pathologic hypertrophy with fibrosis: the structural basis for myocardial failure. Blood Press. 1992. 1:75–85.
Article25. Nicoletti A, Michel JB. Cardiac fibrosis and inflammation: interaction with hemodynamic and hormonal factors. Cardiovasc Res. 1999. 41:532–543.
Article26. Rix M, Andreassen H, Eskildsen P, Langdahl B, Olgaard K. Bone mineral density and biochemical markers of bone turnover in patients with predialysis chronic renal failure. Kidney Int. 1999. 56:1084–1093.
Article27. Coen G, Mazzaferro S, Ballanti P, Bonucci E, Bondatti F, Manni M, Pasquali M, Perruzza I, Sardella D, Spurio A. Procollagen type I C-terminal extension peptide in predialysis chronic renal failure. Am J Nephrol. 1992. 12:246–251.
Article28. Ha SK, Park CH, Seo JK, Park SH, Kang SW, Choi KH, Lee HY, Han DS. Studies on bone markers and bone mineral density in patients with chronic renal failure. Yonsei Med J. 1996. 37:350–356.
Article29. Yoon SJ, Ha JW, Lee SH, Cho DK, Choi S, Seo HS, Hwang HJ, Choi EY, Chung N. Fibrillar collagen turnover index - The clinical importance in the assessment of ventricular hypertrophy and diastolic function in hypertensive patients. Korean Hypertension J. 2007. 13:32–40.30. Cheong ER, Chae SC, Jun JE, Park WH. LV mass and left ventricular systolic function after antihypertensive therapy. J Kor Soc Echo. 1994. 2:187–191.
Article31. Son KH, Lee KN, Kang HS, Choue CW, Kim KS, Kim MS, Song JS, Bae JH. Assessment of left ventricular mass and diastolic function in patients with essential hypertension after one year antihypertensive therapy. J Kor Soc Echo. 1994. 2:71–79.
Article32. Lee H, Lee S, Lee C, Park K, Choi Y, Shin G, Cho HK, Park S. Effects of renal transplantation on echocardiographic changes. J Kor Soc Echo. 2000. 8:31–35.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Heart Failure: Complications of Type 2 Diabetes
- Echocardiographic Differences between Hemodialysis and Essential Hypertension Patients and the Correlations with Factors Affecting the Differences
- Perioperative management of left ventricular diastolic dysfunction and heart failure: an anesthesiologist's perspective
- Diabetic Cardiomyopathy; Summary of 41 years
- A Case of Acquired Ichthyosis Associated with Diabetes Mellitus, Chronic Renal failure and Hypertension