J Korean Soc Spine Surg.
2009 Mar;16(1):24-29. 10.4184/jkss.2009.16.1.24.
Minimally Invasive Transforaminal Lumbar Interbody Fusion
- Affiliations
-
- 1Department of Orthopaedic Surgery, Boomin Hospital, Busan, Korea. osdcb@yahoo.co.kr
- KMID: 1473386
- DOI: http://doi.org/10.4184/jkss.2009.16.1.24
Abstract
-
STUDY DESIGN: A retrospective study
OBJECTIVES
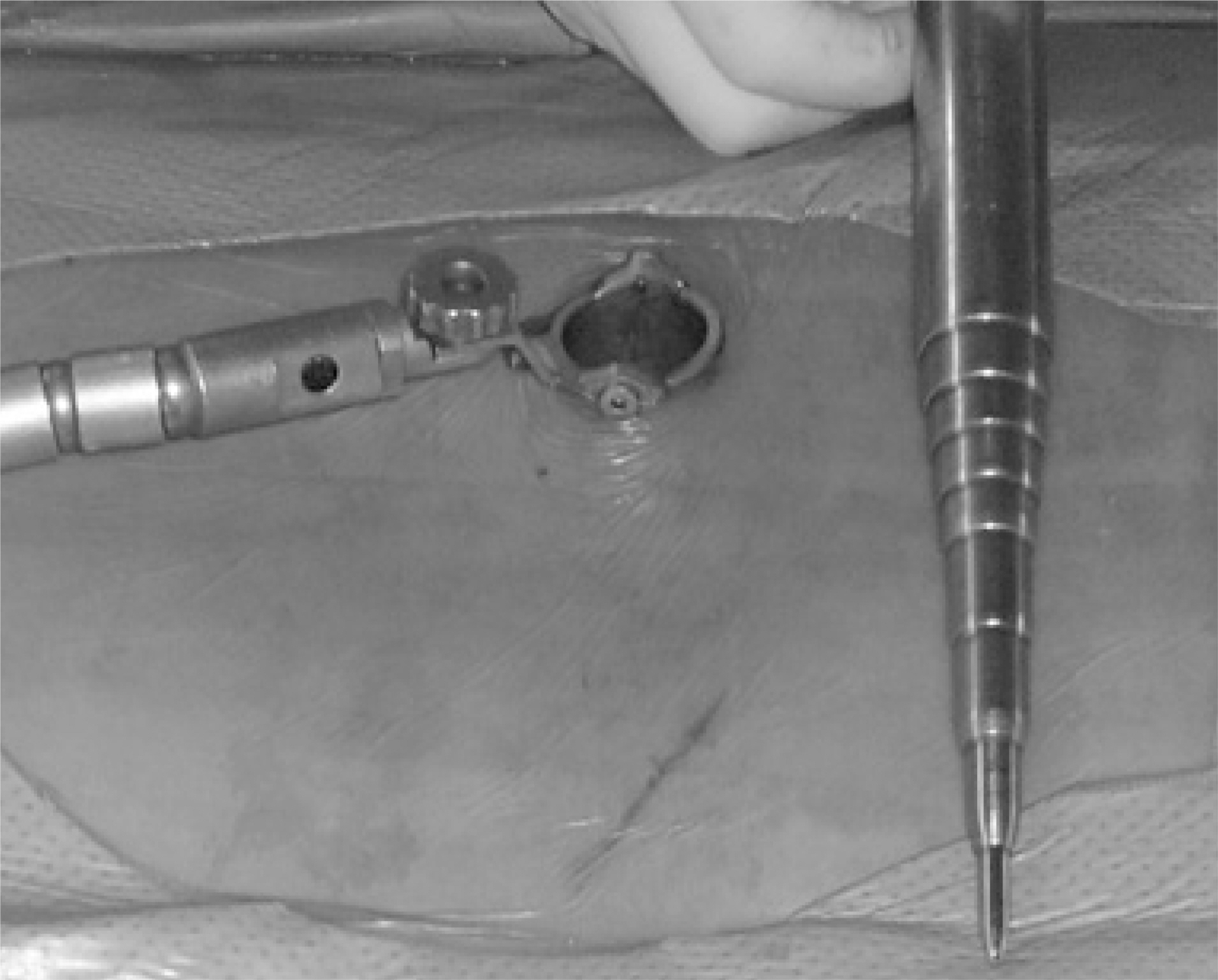
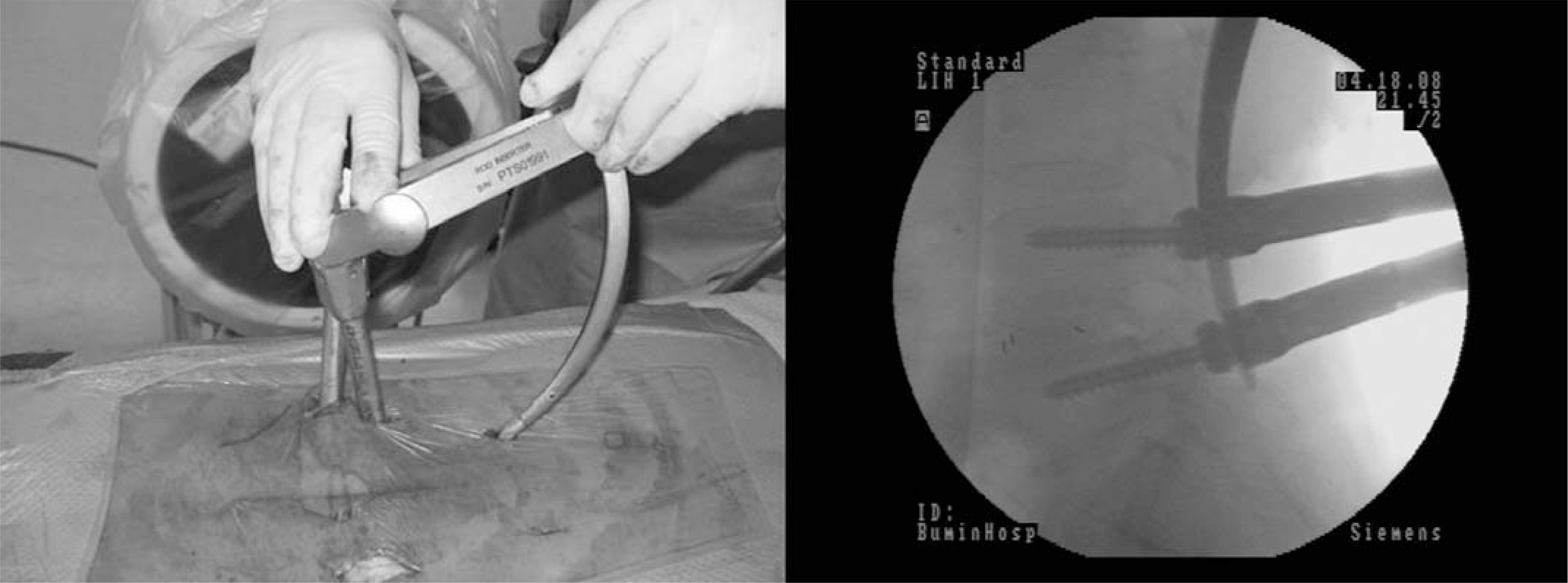
To introduce the technique of minimally invasive transforaminal lumbar interbody fusion and examine its clinical and radiologic results. SUMMARY OF LITERATURE REVIEW: Transforaminal lumbar interbody fusion with a mini-incision using a tubular retractor was recently developed. The aim of this procedure is to reduce the approach-related morbidity and achieve better results in an effective and safe manner.
MATERIALS AND METHODS
Thirty eight patients were followed up for more than 1 year. Their mean age was 57 years and the mean follow-up was 19 months. The diagnosis was spinal stenosis, spondylolisthesis and recurred herniated nucleus pulposus in 22, 14 and 2 patients, respectively. The Oswestry disability index, intervertebral disc space height, fusion rate and complications were evaluated.
RESULTS
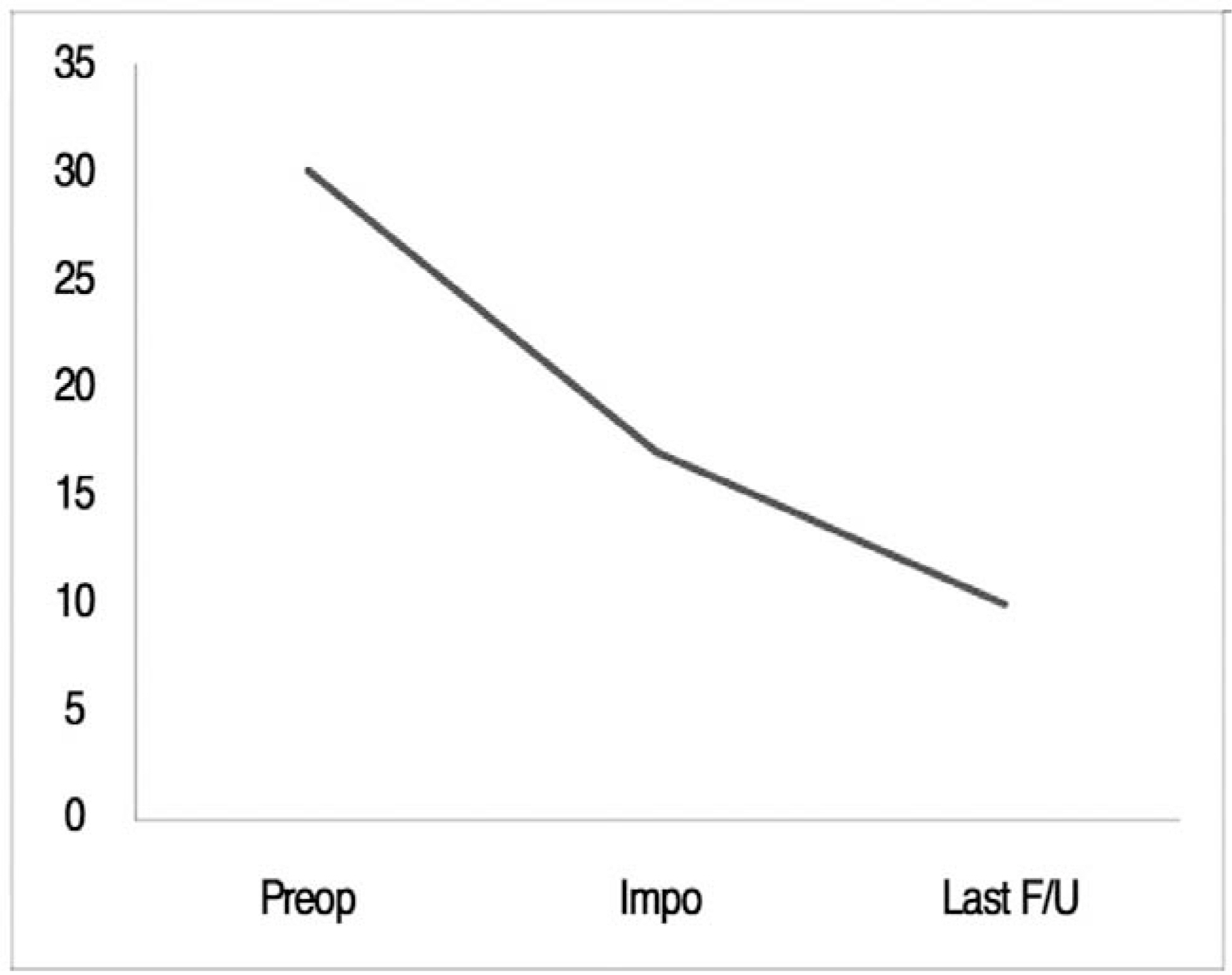
The Oswestry disability index improved from 30 points (range, 50~16 points) to 10 points (range, 2-24 points) at the last follow-up. Thirty-four patients (90%) showed excellent or good results. The intervertebral disc space height increased from 8.7 mm to 10.8 mm. Two cases showed nonunion but the clinical results were good. Complications included one case of infectious spondylitis requiring antibiotics, one case of cage dislodgement requiring additional surgery and one case of a pedicle screw malposition showing no clinical symptoms.
CONCLUSIONS
Minimally invasive transforaminal lumbar interbody fusion reduced the soft tissue injury and blood loss and shortened the recovery period compared to the traditional open techniques.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Old and New Fashion: Minimally Invasive Spine Surgery for Adjacent Segmental Spinal Stenosis after Luque Sublaminar Wiring and Posterolateral Fusion - Case Report -
Seung-Pyo Suh, Jaewon Lee, Chang-Nam Kang
J Korean Soc Spine Surg. 2014;21(4):179-182. doi: 10.4184/jkss.2014.21.4.179.
Reference
-
01). Thomsen K., Christensen FB., Eiskjaer SP., Hansen ES., Fruensuqaard S., B¨ unqer CE. The effects of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion: a prospective, randomized, clinical study. Spine. 1997. 22:2813–2822.02). Steffee AD., Sitkowski DJ. Posterior lumbar interbody fusion and plates. Clin Orthop. 1988. 227:99–102.
Article03). McLaughlin MR., Haid RW., Rodts GE., Subach BR. Posterior lumbar interbody fusion: indications, technique, and results. Clin Neurosurg. 2000. 47:514–527.04). Suk SI., Lee CK., Kim WJ., Lee JH., Cho KJ., Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine. 1997. 22:210–219.
Article05). Foley KT., Holly LT., Schwender JD. Minimally invasive lumbar fusion. Spine. 2003. 15:26–35.
Article06). Schwender JD., Holly LT., Rouben DP., Foley KT. Minimally invasive transforaminal lumbar interbody fusion: technical feasibility and initial results. J Spinal Disord Tech. 2005. 18:1–6.07). Holly LT., Schwender JD., Rouben DP., Foley KT. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus. 2006. 20:1–5.
Article08). Kirkaldy-Willis WH., Paine KWE., Cauchoix J., McIvor G. Lumbar spinal stenosis. Clin Orthop. 1974. 99:30–50.09). Bridwell KH., Lenke LG., McEnery KW., Baldus C., Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine. 1995. 20:1410–1418.
Article10). Lee SH., Kim YB., Kim TS, et al. Transforaminal lumbar interbody fusion for the treatment of nonunion after posterolateral lumbar fusion. J Kor Spine Surg. 2004. 11:223–230.
Article11). Kawaguchi Y., Matsui H., TsujiH . Back muscle injury after posterior lumbar spine surgery. Part 2: Histologic and histochemical analyses in humans. Spine. 1994. 19:2598–2602.12). Kawaguchi Y., Matsui H., Tsuji H. Back muscle injury after posterior lumbar spine surgery. A histologic and enzymatic analysis. Spine. 1996. 21:941–944.13). Gejo R., Matsui H., Kawaguchi Y., Ishihara H., Tsuji H. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine. 1999. 24:1023–1028.
Article14). Rantanen J., Hurme M., Falck B, et al. The lumbar multifidus muscle five years after surgery for a lumbar intervertebral disc herniation. Spine. 1993. 18:568–574.
Article15). Park Y., Ha JW. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine. 2007. 32:537–543.
Article16). Harms JG., Jeszenszky D. The unilateral transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol. 1998. 6:88–99.17). Ray CD. Threaded titanium cages for lumbar interbody fusions. Spine. 1997. 22:667–680.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- Mini-invasive unilateral transforaminal lumbar interbody fusion and pedicle screw fixation
- Technique of Biportal Endoscopic Transforaminal Lumbar Interbody Fusion
- The Result of Minimally Invasive Transforaminal Lumbar Interbody Fusion in Low Grade Spondylolisthesis - Minimum 2 Years Follow Up -
- History and Evolution of the Minimally Invasive Transforaminal Lumbar Interbody Fusion