Treatment of Intertrochanteric Fracture of the Femur Using a Dyna Locking Trochanteric (DLT) Nail
- Affiliations
-
- 1Department of Orthopaedic Surgery, St. Paul's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. hnsukku@catholic.ac.kr
- 2Department of Orthopaedic Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 1461173
- DOI: http://doi.org/10.5371/jkhs.2010.22.3.216
Abstract
- PURPOSE
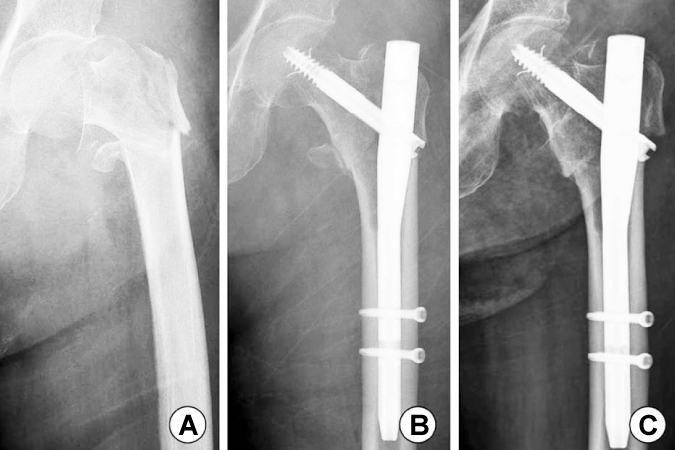
We analyzed the clinical and radiological results after treatment of intertrochanteric fracture of the femur using a Dyna locking trochanteric (DLT) nail.
MATERIALS AND METHODS
From March 2008 to February 2009, 36 patients (10 males and 26 females) who had at least 6 months follow-up among 43 patients were included in our study. The average age of the patients was 76.4 years (range: 65~90 years) and the average follow-up period was 13.4 months (range: 9~21 months). We evaluated the radiological results such as the neck-shaft angle and the sliding length of the lag screw at last follow-up and the clinical results such as intraoperative complications, the operation time, the postoperative blood loss and the incidence of fixation failure.
RESULTS
The average neck-shaft angle at last follow-up was 131.1 degrees and the average sliding length of lag screw was 3.6 mm. Two cases (5.6%) of femoral shaft fracture during the insertion of a lag screw or nail happened and one case of stress fracture of the femoral neck occurred. Two cases of fixation failure developed due to deep infection or varus angulation.
CONCLUSION
Fixation using a DLT nail can be a good option for the treatment of intertrochanteric fractures of the femur.
MeSH Terms
Figure
Cited by 4 articles
-
Mid-term Results of Patients with Femoral Intertrochanteric Fractures Treated with Proximal Femoral Nail Antirotation
Suk Kyu Choo, Hyoung Keun Oh, Sung Jong Woo
Hip Pelvis. 2012;24(2):124-132. doi: 10.5371/hp.2012.24.2.124.Comparison of the Dyna Locking Trochanteric Nail, Proximal Femoral Nail Antirotation and Gamma 3 Nail in Treatment of Intertrochanteric Fracture of the Femur
Sung Soo Kim, Kyu Yeol Lee, Chul Hong Kim, Myung Jin Lee, Lih Wang, Hyeon Jun Kim, Sun Hyo Kim
Hip Pelvis. 2013;25(3):211-219. doi: 10.5371/hp.2013.25.3.211.Proximal Femoral Nail Antirotation and Proximal Femoral Nail in Intertrochanteric Fractures
Sung Soo Kim, Chul Hong Kim, Jin Hun Kang, Dong Hoon Han, Yong Seung O
J Korean Orthop Assoc. 2011;46(5):392-398. doi: 10.4055/jkoa.2011.46.5.392.Intrapelvic Migration of the Lag Screw with Wedge Wing from Dyna Locking Trochanteric Nail: A Case Report and Literature Review
Yong-Woo Kim, Weon-Yoo Kim, Kyong-Jun Kim, Se-Won Lee
Hip Pelvis. 2019;31(2):110-119. doi: 10.5371/hp.2019.31.2.110.
Reference
-
1. Aharonoff GB, Koval KJ, Skovron ML, Zuckerman JD. Hip fractures in the elderly: predictors of one year mortality. J Orthop Trauma. 1997. 11:162–165.
Article2. Strauss E, Frank J, Lee J, Kummer FJ, Tejwani N. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: a biomechanical evaluation. Injury. 2006. 37:984–989.
Article3. Stern MB, Angerman A. Comminuted intertrochanteric fractures treated with a Leinbach prosthesis. Clin Orthop Relat Res. 1987. 218:75–80.
Article4. Kim WY, Han CH, Park JI, Kim JY. Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop. 2001. 25:360–362.
Article5. Min WK, Kim SY, Kim TK, et al. Proximal femoral nail for the treatment of reverse obliquity intertrochanteric fractures compared with gamma nail. J Trauma. 2007. 63:1054–1060.
Article6. Anglen JO, Weinstein JN. American Board of Orthopaedic Surgery Research Committee. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008. 90:700–707.
Article7. Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res. 1998. 348:87–94.
Article8. Laros GS, Moore JF. Complications of fixation intertrochanteric fractures. Clin Orthop Relat Res. 1974. 101:110–119.9. Thomas AP. Dynamic hip screws that fail. Injury. 1991. 22:45–46.
Article10. Bartucci EJ, Gonzalez MH, Cooperman DR, Freedberg HI, Barmada R, Laros GS. The effect of adjunctive methylmethacrylate on failures of fixation and function in patients with intertrochanteric fracture and osteoporosis. J Bone Joint Surg Am. 1985. 67:1094–1107.
Article11. Moroni A, Faldini C, Pegreffi F, Giannini S. HA-coated screws decrease the incidence of fixation failure in osteoporotic trochanteric fractures. Clin Orthop Relat Res. 2004. 425:87–92.
Article12. Madsen JE, Naess L, Aune AK, Alho A, Ekeland A, Strømsøe K. Dynamic hip screw with trochanteric stabilizing plate in the treatment of unstable proximal femoral fractures: a comparative study with the Gamma nail and compression hip screw. J Orthop Trauma. 1998. 12:241–248.
Article13. Godfried Y. The lateral trochanteric wall: a key element in the reconstruction of unstable pertrochantric fractures. Clin Orthop Relat Res. 2004. 425:82–86.14. Simmermacher RK, Ljungqvist J, Bail H, et al. The new proximal femoral nail antirotation (PFNA) in daily practice: results of a multicentre clinical study. Injury. 2008. 39:932–939.
Article15. Lenich A, Mayr E, Rüter A, Möckl Ch, Füchtmeier B. First results with the trochanteric fixation nail (TFN): a report on 120 cases. Arch Orthop Trauma Surg. 2006. 126:706–712.
Article16. Heinert G, Parker MJ. Intramedullary osteosynthesis of complex proximal femoral fractures with the Targon PF nail. Injury. 2007. 38:1294–1299.
Article17. Efstathopoulos NE, Nikolaou VS, Lazarettos JT. Intramedullary fixation of intertrochanteric hip fractures: a comparision of two implant design. Int Orthop. 2007. 31:71–76.
Article18. Mahomed N, Harrinton I, Kellam J, Maisrelli G, Hearn T, Vroemen J. Biomechanical analysis of the Gamma nail and sliding hip screw. Clin Orthop Relat Res. 1994. 304:280–288.
Article19. Flores LA, Harrington IJ, Heller M. The stability of intertrochanteric fractures treated with a sliding screw-plate. J Bone Joint Surg Br. 1990. 72:37–40.
Article20. Bjørgul K, Reikerås O. Outcome after treatment of complications of Gamma nailing: a prospective study of 554 trochanteric fractures. Acta Orthop. 2007. 78:231–235.
Article21. Haidukewych GJ. Intertrochanteric fractures: ten tips to improve results. J Bone Joint Surg Am. 2009. 91:712–719.22. Cameron HU, Pillar RM, Hastings DE, Fornasier VL. Iatrogenic subcapital fracture of the hip: a new complication of intertrochanteric fracture. Clin Orthop Relat Res. 1975. 112:218–220.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the Dyna Locking Trochanteric Nail, Proximal Femoral Nail Antirotation and Gamma 3 Nail in Treatment of Intertrochanteric Fracture of the Femur
- Intrapelvic Migration of the Lag Screw with Wedge Wing from Dyna Locking Trochanteric Nail: A Case Report and Literature Review
- Outcomes of Wedge Wing in the Lag Screw for Unstable Intertrochanteric Fractures in Elderly Patients
- Comparison of Compression Hip Screw, Captured Hip Screw and Gamma-Locking Nail in Intertrochanteric Fracture of Femur
- Rendezvous Surgery for Peri-Implant Fractures around Locking Compression Plate on Anterolateral Bowed Femur - A Case Report -