J Korean Hip Soc.
2010 Mar;22(1):66-72. 10.5371/jkhs.2010.22.1.66.
Staged Revision of Infected Hip Arthroplasty Using an Antibiotics-Loaded Intra-Articular Cement Spacer with Retention of the Stem
- Affiliations
-
- 1Department of Orthopedic Surgery, Sang-Gye Paik Hospital, College of Medicine, Inje University, Seoul, Korea. ybs58@paik.ac.kr
- KMID: 1461081
- DOI: http://doi.org/10.5371/jkhs.2010.22.1.66
Abstract
- PURPOSE
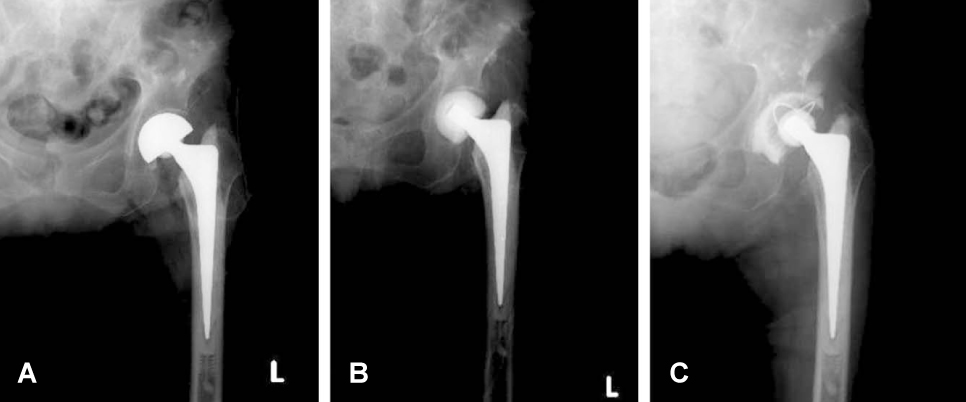
When the femoral stem was well fixed in patients with a deep prosthetic hip infection, the authors performed a two-stage revision procedure using antibiotic-loaded cement spacers (ALCS) without removal of the stem, and the efficacy of this treatment was assessed.
MATERIALS AND METHODS
For 12 cases of infected hip arthroplasties, a two-stage procedure was performed, and the patients were followed up for over 2 years. After the acetabular component and head was removed, debridement was done. The molded ALCS was inserted. Revision was then performed after eradication of the infection. The results were analyzed, including the changes in the clinical manifestation, the radiologic findings, the laboratory results, the functional score and the complications.
RESULTS
Of all 12 cases, the two-stage revision arthroplasty using an ALCS with retention of the stem was performed in 11 cases (92%), on an average of 66 days (range: 40~152 days). In the 11 revised cases, there was no evidence of recurrence of infection. In the 11 cases, the mean Harris hip score improved from 40.1 points preoperatively to 91.8 points at last the follow-up. The mean WOMAC score improved from 41.8 points preoperatively to 81 points at the last follow-up. The mean Harris hip score was 85.3 points and the WOMAC score was 72.4 points during the ALCS insertion-period.
CONCLUSION
For the case of a perioprosthetic hip infection with a well-fixed femoral stem, two-staged revision using an ALCS without stem removal could be an alternative method in terms of effective infection control and preservation of the joint function.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Long-Term Clinical Outcome of Two Stage Revision Surgery for Infected Hip Arthroplasty Using Cement Spacer
Joon-Soon Kang, Kyoung Ho Moon, Tong-Joo Lee, Young-Tae Kim, Dong-Jin Ryu, Jae-Hwang Choi
J Korean Orthop Assoc. 2014;49(5):355-365. doi: 10.4055/jkoa.2014.49.5.355.Staged Revision of Infected-hip Arthroplasty Using an Antibiotics-loaded Intra-articular Cement Spacer: Impact on Cemented and Cementless Stem Retention
Kyu-Sub Um, Joong-Won Lee, Byung-Ho Yoon, Yerl-Bo Sung
Hip Pelvis. 2020;32(1):26-34. doi: 10.5371/hp.2020.32.1.26.
Reference
-
1. Canner GC, Steinberg ME, Heppenstall BR, Richard B. The infected hip after total hip arthroplasty. J Bone Joint Surg Am. 1984. 66:1393–1399.
Article2. Phillips JE, Crane TP, Noy M, Elliott TS, Grimer RJ. The incidence of deep prosthetic infections in a specialist orthopaedic hospital: a 15-year prospective survey. J Bone Joint Surg Br. 2006. 88:943–948.3. Volin SJ, Hinrichs SH, Garvin KL. Two-stage reimplantation of total joint infections: a comparison of resistant and non-resistant organisms. Clin Orthop Relat Res. 2004. 427:94–100.4. Deshmukh RG, Thevarajan K, Kok CS, Sivapathasundaram N, George SV. An intramedullary cement spacer in total hip arthroplasty. J Arthroplasty. 1998. 13:197–199.
Article5. Garvin KL, Hanssen AD. Infection after total hip arthroplasty. Past, present, and future. J Bone Joint Surg Am. 1995. 77:1576–1588.
Article6. Booth RE, Lotke PA. The results of spacer block technique in revision of infected total knee arthroplasty. Clin Orthop Relat Res. 1989. 248:57–60.
Article7. Ivarsson I, Wahlström O, Djerf K, Jacobsson SA. Revision of infected hip replacement. Two-stage procedure with a temporary gentamicin spacer. Acta Orthop Scand. 1994. 65:7–8.
Article8. Lord GA, Hardy JR, Kummer FJ. An uncemented total hip replacement: experimental study and review of 300 madreporique arthroplasties. Clin Orthop Relat Res. 1979. 141:2–16.9. Fitzgerald RH Jr, Nolan DR, Ilstrup DM, Van Scoy RE, Washington JA 2nd, Coventry MB. Deep wound sepsis following total hip arthroplasty. J Bone Joint Surg Am. 1977. 59:847–855.
Article10. Lonner JH, Desai P, Dicesare PE, Steiner G, Zuckerman JD. The reliability of analysis of intraoperative frozen sections for identifying active infection during revision hip or knee arthroplasty. J Bone Joint Surg Am. 1996. 78:1553–1558.
Article11. Mirra JM, Amstutz HC, Matos M, Gold R. The pathology of the joint tissues and its clinical relevance in prosthesis failure. Clin Orthop Relat Res. 1976. 117:221–240.
Article12. Buchholz HW, Elson RA, Engelbrecht E, Lodenkämper H, Röttger J, Siegel A. Management of deep infection of total hip replacement. J Bone Joint Surg Br. 1981. 63:342–353.
Article13. Callaghan JJ, Katz RP, Johnston RC. One-stage revision surgery of the infected hip. A minimum 10-year follow up study. Clin Orthop Relat Res. 1999. 369:139–143.14. Bittar ES, Petty W. Girdlestone arthroplasty for infected total hip arthroplasty. Clin Orthop Relat Res. 1982. 170:83–87.
Article15. Antii-Poikia I, Santavirta S, Konttinen YT, Honkanen V. Outcome of the infected hip arthroplasty. A retrospective study of 36 patients. Acta Orthop Scand. 1989. 60:670–675.
Article16. Balderston RA, Hiller WD, Iannotti JP, et al. Treatment of the septic hip with total hip arthroplasty. Clin Orthop Relat Res. 1987. 221:231–237.
Article17. Lieberman JR, Callaway GH, Salvati EA, Pellicci PM, Brause BD. Treatment of the infected total hip arthroplasty with a two-stage reimplantation protocol. Clin Orthop Relat Res. 1994. 301:205–212.
Article18. Salvati EA, Chekofsky KM, Brause BD, Wilson PD Jr. Reimplantation in infection: a 12-year experience. Clin Orthop Relat Res. 1982. 170:62–75.19. Younger AS, Duncan CP, Masri BA. Treatment of infection associated with segmental bone loss in the proximal part of the femur in two stages with use of an antibiotic-loaded interval prosthesis. J Bone Joint Surg Am. 1998. 80:60–69.
Article20. Kendall RW, Masri BA, Duncan CP, Beauchamp CP, McGraw RW, Bora B. Temporary antibiotic loaded acrylic hip replacement: a novel method for management of the infected THA. Semin Arthroplasty. 1994. 5:171–177.21. Sanchez-Sotelo J, Berry DJ, Hanssen AD, Cabanela ME. Midterm to long-term followup of staged reimplantation for infected hip arthroplasty. Clin Orthop Relat Res. 2009. 467:219–224.
Article22. Cordero J, Munuera L, Folgueira MD. Influence of bacterial strains on bone infection. J Orthop Res. 1996. 14:663–667.
Article23. Struhl S, Harwin SF, Stern RE, Kulick RG. Infected uncemented hip arthroplasty. Preserving the femoral stem with a two-stage revision procedure. Orthopaedic Rev. 1989. 18:707–712.24. Yoon TR, Rowe SM, Park CH, Jung SN. Treatment of infected uncemented total hip arthroplasty: two-stage revision procedure by preserving well-fixed femoral components in four cases. J Korean Orthop Assoc. 2000. 35:467–471.
Article25. Gristina AG, Naylor PT, Webb LX. Molecular mechanisms in musculoskeletal sepsis: the race for the surface. Instr Course Lect. 1990. 39:471–482.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Staged Revision of Infected-hip Arthroplasty Using an Antibiotics-loaded Intra-articular Cement Spacer: Impact on Cemented and Cementless Stem Retention
- Treatment of Infected uncemented Total Hip Arthroplasty: Two-stage revision procedure by preserving well-fixed femoral components in four cases
- Long-Term Clinical Outcome of Two Stage Revision Surgery for Infected Hip Arthroplasty Using Cement Spacer
- Functional Outcome after Reimplantation in Patients Treated with and without an Antibiotic-Loaded Cement Spacers for Hip Prosthetic Joint Infections
- Staged Reimplantation using PROSTALAC in Infected Total Hip Arthroplasty: A Case Report