J Korean Soc Radiol.
2010 Apr;62(4):383-388. 10.3348/jksr.2010.62.4.383.
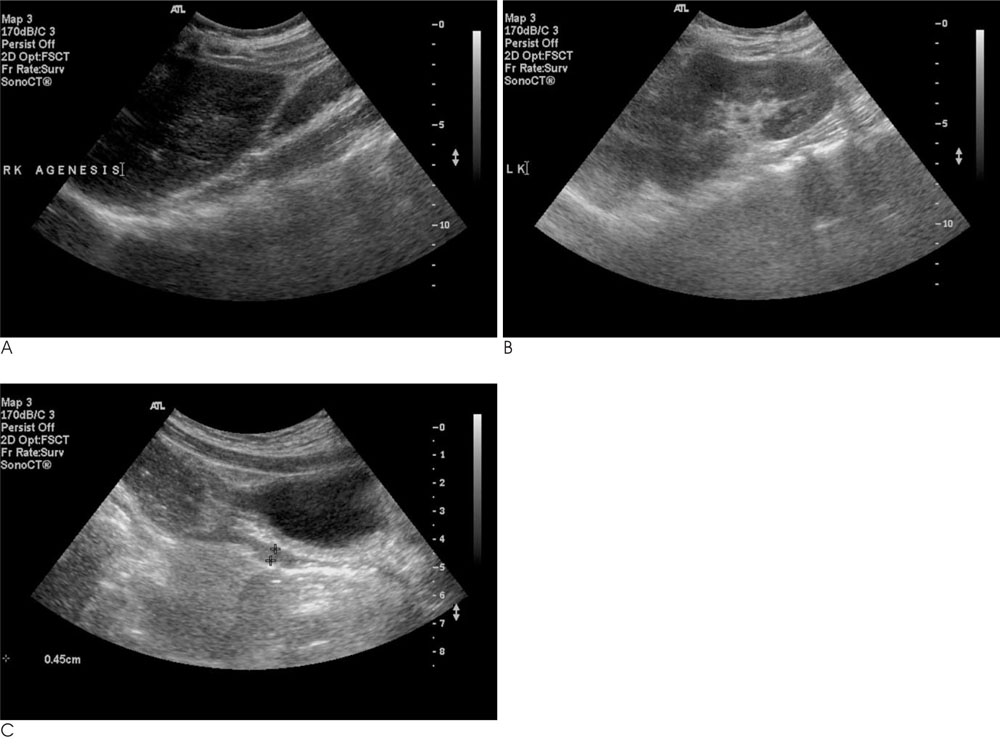
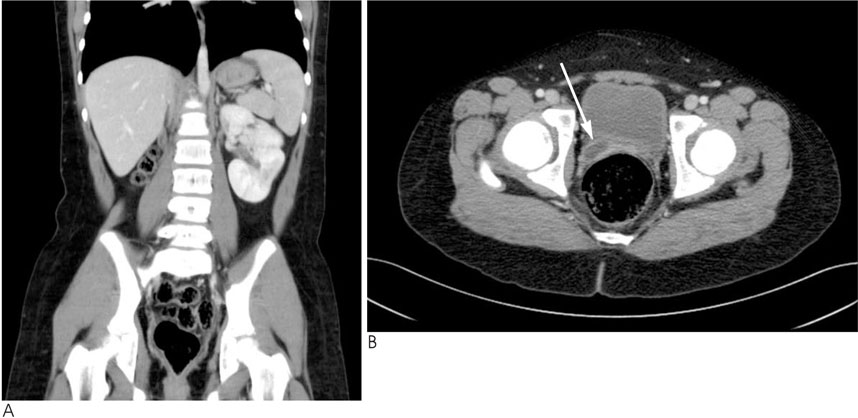
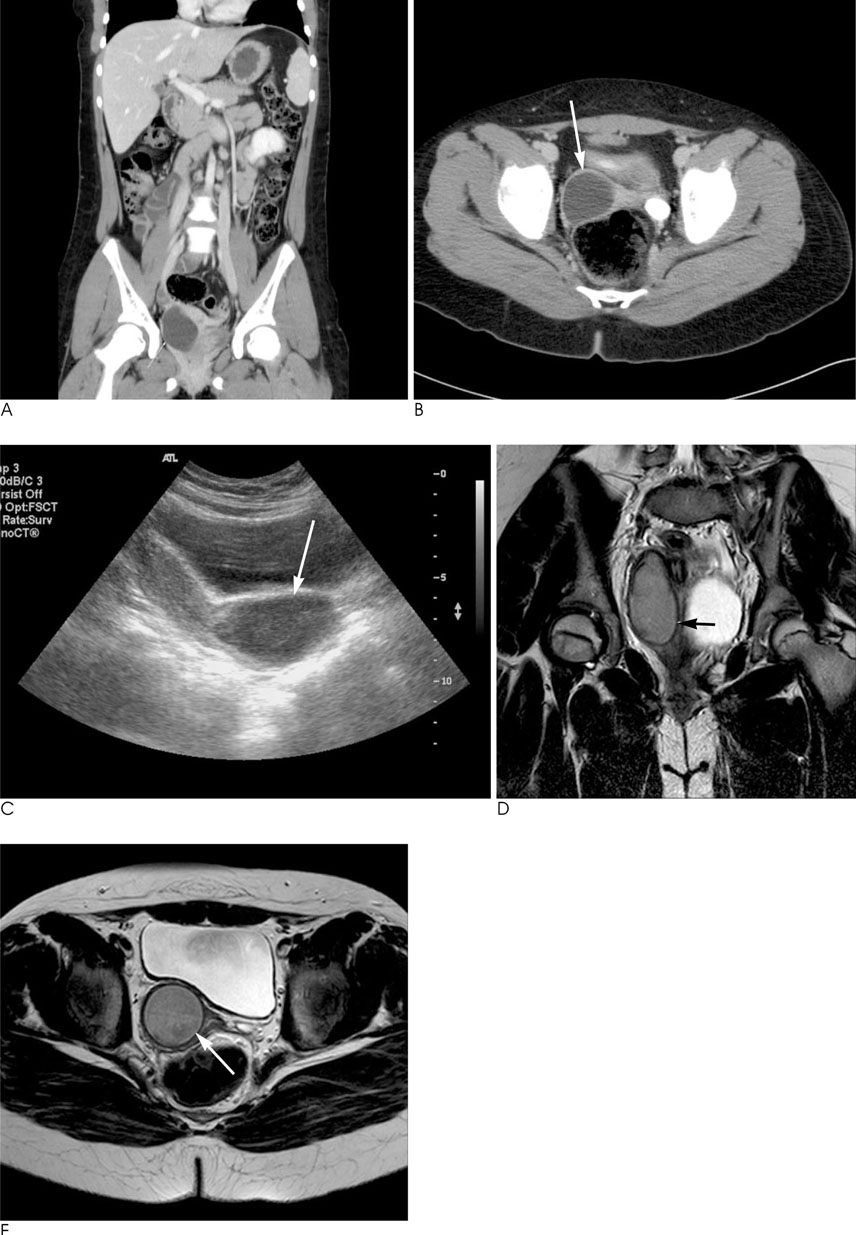
Herlyn-Werner-Wunderlich Syndrome with Unilateral Hemivaginal Obstruction, Ipsilateral Renal Agenesis, and Contralateral Renal Thin GBM Disease: A Case Report with Radiological Follow Up
- Affiliations
-
- 1Department of Radiology, Myongji Hospital, Kwandong University, College of Medicine, Korea.
- 2Department of Radiology, Bucheon Hospital, Soonchunhyang University, Korea.
- KMID: 1460074
- DOI: http://doi.org/10.3348/jksr.2010.62.4.383
Abstract
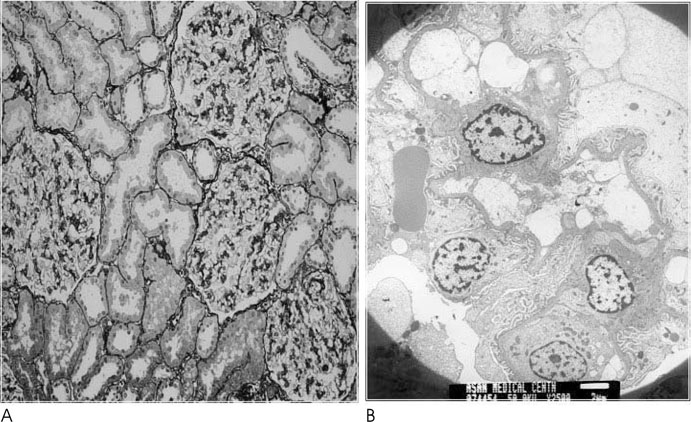
- Herlyn-Werner-Wunderlich syndrome is a rare Mullerian ductal anomaly that is characterized by the presence of a hemivaginal septum, a didelphic uterus and ipsilateral renal agenesis. It is generally difficult to diagnose the uterine malformation before menarche owing to its small size. Therefore, a follow-up study is very important for confirming the uterine malformation in girls with renal agenesis. We report a patient with renal agenesis and microscopic hematuria, who showed symptoms before menarche. A follow-up study eventually revealed uterine didelphys with a hemivaginal obstruction. A biopsy proved that the microscopic hematuria was caused by thin glomerular basement membrane disease of the contralateral kidney.
MeSH Terms
Figure
Reference
-
1. Purslow CE. A case of unilateral haematocolpos, haematometra and haematosalpinx. J Obstet Gynaecol Br Emp. 1922; 29:643.2. Siegelman ES, Outwater EK, Banner MP, Ramchandani P, Anderson TL, Schnall MD. High resolution MR imaging of the vagina. Radiographics. 1997; 17:1183–1203.3. Gholoum S, Puligandla PS, Hui T, Su W, Quiros E, Laberge JM. Management and outcome of patients with combined vaginal septum, bifid uterus and ipsilateral renal agenesis (Herlyn-Werner-Wunderlich syndrome). J Pediatr Surg. 2006; 41:987–992.4. Herlyn U, Werner H. Simultaneous occurrence of an open Gartner-duct cyst. A homolateral aplasia of the kidney and a double uterus as a typical syndrome of abnormalities. Geburtshilfe Frauenheilkd. 1971; 31:340–347.5. Wunderlich M. Unusual form of genital malformation with aplasia of the right kidney. Zentralbl Gynakol. 1976; 98:559–562.6. Orazi C, Lucchetti MC, Schingo PM, Marchetti P, Ferro F. Herlyn-Werner-Wunderlich syndrome: uterus didephys, blind hemivagina and ipsilateral renal agenesis. Sonographic and MR findings in 11 cases. Pediatr Radiol. 2007; 37:657–665.7. Kiechl-Kohlendorfer U, Geley TE, Unsinn KM, Gaβner I. Diagnosing neonatal female genital anomalies using saline-enhanced sonography. AJR Am J Roentgenol. 2001; 177:1041–1044.8. Candiani GB, Fedele L, Candiani M. Double uterus, blind hemivagina and ipsilateral renal agenesis: 36 cases and long-term follow-up. Obstet Gynecol. 1997; 90:26–32.9. Prada Arias M, Muguerza Vellibre R, Montero Sánchez M, Vázquez Castelo JL, Arias González M, Rodriguez Costa A. Uterus didelphys with obstructed hemivagina and multicystic dysplastic kidney. Eur J Pediatr Surg. 2005; 15:441–445.10. Tanaka YO, Kurosaki Y, Kobayashi T, et al. Uterus didelphys associated with obstructed hemvagina and ipsilateral renal agenesis: MR findings in seven cases. Abdom Imaging. 1998; 23:437–441.11. Mishra A. Renal agenesis: report of an interesting case. Br J Radiol. 2007; 80:e167–e169.12. Morcel K, Camborieux L. Programme de Recherches sur les Aplasies Müllériennes (PRAM). Guerrier D. Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. Orphanet J Rare Dis. 2007; 2:13.13. Zurawin RK, Dietrich JE, Heard MJ, et al. Didelphic uterus and obstructed hemivagina with renal agenesis: case report and review of the literature. J Pediatr Adolesc Gynecol. 2004; 17:137–141.14. Batt RE, Mitwally MF. Endometriosis from thelarche to midteens: pathogenesis and prognosis, prevention and pedagogy. J Pediatr Adolesc Gynecol. 2003; 16:337–347.15. Sanfilippo JS, Wakim NG, Schikler KN, Yussman MA. Endometriosis in association with uterine anomaly. Am J Obstet Gynecol. 1986; 154:39–43.16. Royat CS, Joshi K, Dey P, Sakhuja V, Minz RW, Datta U. Glomerular morphometry in biopsy evaluation of minimal change disease, membranous glomerulonephritis, thin basement membrane disease and Alport's syndrome. Anal Quant Cytol Histol. 2007; 29:173–182.17. Kashtan CE. Familial hematuric syndromes-Alport syndrome, thin glomerular basement membrane disease and Fechtner/Epstein syndromes. Contrib Nephrol. 2001; (136):79–99.18. Kashtan CE. Alport syndrome and thin glomerular basement membrane disease. J Am Soc Nephrol. 1998; 9:1736–1750.19. Hebert A, Betts JA, Sedmak DD, Cosio FG, Bay WH, Carlton S. Loin pain-hematuria syndrome associated with thin glomerular basement membrane disease and hemorrhage into renal tubules. Kidney Int. 1996; 49:168–173.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thin Glomerular Basement Membrane Disease with Herlyn-Werner-Wunderlich Syndrome: Uterus Didelphys, Blind Hemivagina and Ipsilateral Renal Agenesis
- Two Cases of Herlyn-Werner-Wunderlich Syndrome
- Herlyn-Werner-Wunderlich Syndrome: A Mini-review
- Two Cases of Herlyn-Werner-Wunderlich Syndrome Diagnosed in Perinatal Period
- A case of Herlyn-Werner-Wunderlich syndrome diagnosed in asymptomatic newborn