J Korean Surg Soc.
2010 Jul;79(1):71-74. 10.4174/jkss.2010.79.1.71.
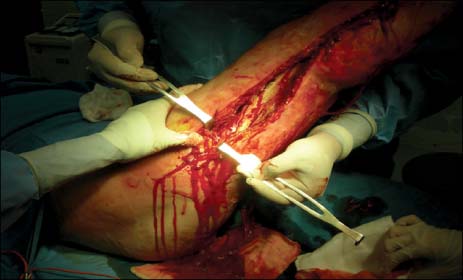
Necrotizing Fasciitis Following a Small Burn
- Affiliations
-
- 1Department of Surgery, Burn Center, Hangang Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea. dohern@hallym.ac.kr
- 2Department of Dermatology and Cutaneous Biology Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1455490
- DOI: http://doi.org/10.4174/jkss.2010.79.1.71
Abstract
- Necrotizing fasciitis (NF) is a life-threatening soft tissue infection that manifests with a rapid course of inflammation and necrosis of the skin, subcutaneous fat, and fascia. NF commonly follows trauma to the skin, such as a laceration, scratch or insect bite. NF is a surgical emergency and requires both a high index of suspicion for diagnosis and prompt operative intervention. Early aggressive surgical intervention is important for improving survival rates. Mortality and morbidity can be decreased with early diagnosis, adequate and urgent surgical debridement, intensive supportive care, and wound resurfacing. Recently, we experienced a case of NF secondary to a third-degree contact burn on the dorsum of the right foot (1% body area). We report our therapeutic experience in this case, with a review of the literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Wong CH, Yam AK, Tan AB, Song C. Approach to debridement in necrotizing fasciitis. Am J Surg. 2008. 196:e19–e24.2. Bono G, Argo A, Zerbo S, Triolo V, Procaccianti P. Cervical necrotizing fasciitis and descending necrotizing mediastinitis in a patient affected by neglected peritonsillar abscess: a case of medical negligence. J Forensic Leg Med. 2008. 15:391–394.3. Faucher LD, Morris SE, Edelman LS, Saffle JR. Burn center management of necrotizing soft-tissue surgical infections in unburned patients. Am J Surg. 2001. 182:563–569.4. Hsiao CT, Weng HH, Yuan YD, Chen CT, Chen IC. Predictors of mortality in patients with necrotizing fasciitis. Am J Emerg Med. 2008. 26:170–175.5. Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL, Low CO. Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am. 2003. 85-A:1454–1460.6. Hasham S, Matteucci P, Stanley PR, Hart NB. Necrotising fasciitis. BMJ. 2005. 330:830–833.7. Tsai CC, Lin SD, Lai CS, Chou CK. A clinical analysis of necrotizing fasciitis: a review of 54 cases. Gaoxiong Yi Xue Ke Xue Za Zhi. 1995. 11:673–677.8. Ku HW, Chang KJ, Chen TY, Hsu CW, Chen SC. Abdominal necrotizing fasciitis due to perforated colon cancer. J Emerg Med. 2006. 30:95–96.9. Akhtar S, Hasham S, Abela C, Phipps AR. The use of Integra in necrotizing fasciitis. Burns. 2006. 32:251–254.10. Jallali N, Withey S, Butler PE. Hyperbaric oxygen as adjuvant therapy in the management of necrotizing fasciitis. Am J Surg. 2005. 189:462–466.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Necrotizing Fasciitis in an Uncontrolled Diabetic Alcoholic with a Small Untreated Wound
- Fatal Necrotizing Fasciitis Due to Pseudomonas aeruginosa After Vaccination : A Case Report
- Necrotizing Fasciitis of the Chest Wall Complicating Acupuncture
- A Case of Necrotizing Fasciitis of the Face
- A Case of Necrotizing Fasciitis